

Original Article - Year 2022 - Volume 37 -
Giant lipomas of the hand, case series
Lipomas gigantes da mão, série de casos
ABSTRACT
Introduction: Lipomas are sporadic in hand and represent less than 5% of soft tissue tumors in this topography. Giant lipomas, even less common, are defined as having a diameter greater than 5 cm.
Methods: We performed a retrospective analysis of the cases of patients with giant lipomas of the hand seen in the period 2017-2020, at Hospital Pasteur and Hospital de Clínicas, in Montevideo, Uruguay.
Results: We obtained four patients during the study period. The age of presentation was between 51 and 62 years (mean 57 years). Three lipomas were deep intramuscular, and one was superficial to the regional muscles. The largest had a longer axle of 70mm. All were symptomatic. Marginal resection was performed in all of them, and the postoperative period was uneventful or recurrent. Histopathology confirmed typical lipoma in three cases and lipoma with bone metaplasia in the other.
Conclusion: Giant lipomas of the hand present as painless, slow-growing tumors that may be symptomatic when compressing adjacent structures. Magnetic resonance imaging is the imaging study of choice for these cases. The applicable treatment is marginal surgical resection, and recurrence is uncommon.
Keywords: Lipoma; Hand; Sarcoma; Soft tissue neoplasms; Case reports.
RESUMO
Introdução: Os lipomas são esporádicos na mão e representam menos de 5% dos tumores de partes moles nesta topografia. Os lipomas gigantes, ainda menos comuns, são definidos por terem um diâmetro maior do que 5cm.
Métodos: Executamos uma análise retrospectiva dos casos de pacientes com lipomas gigantes de mão, atendidos no período de 2017-2020, no Hospital Pasteur e Hospital de Clínicas, em Montevidéu, Uruguai.
Resultados: Obtivemos quatro pacientes no período estudado. A idade de apresentação foi entre 51 e 62 anos (média de 57 anos). Três dos lipomas eram intramusculares profundos e um era superficial aos músculos regionais. O maior possuía eixo mais extenso de 70mm. Todos eram sintomáticos. A ressecção marginal foi realizada em todos eles, e o pós-operatório transcorreu sem intercorrências ou recorrências. A histopatologia confirmou lipoma típico em três casos, e lipoma com metaplasia óssea no outro.
Conclusão: Lipomas gigantes de mão se apresentam como tumores indolores e de crescimento lento, que podem ser sintomáticos ao comprimir estruturas adjacentes. A ressonância magnética é o estudo de imagem escolhido para estes casos. O tratamento aplicável é a ressecção cirúrgica marginal e a recorrência é pouco comum.
Palavras-chave: Lipoma; Mãos; Sarcoma; Neoplasias de tecidos moles; Relatos de casos
INTRODUCTION
Lipoma is the most common benign soft-tissue tumor, but it is rare in hand, representing less than 5% in this topography1,2. Giant lipomas are those larger than 5 cm and are even less common3.
OBJECTIVE
This paper presents our experience with giant lipomas of the hand and reviews the bibliography associated with its clinical presentation, imaging studies, differential diagnoses, and treatment.
METHODS
A retrospective analysis of the cases of patients diagnosed with lipoma of the hand treated in 2017-2020 was carried out at the two training centers for residents in Plastic Surgery in Uruguay (Hospital Pasteur, Hospital de Clínicas).
Lipomas that presented at least one of their dimensions greater than 5cm were included.
Clinical case 1
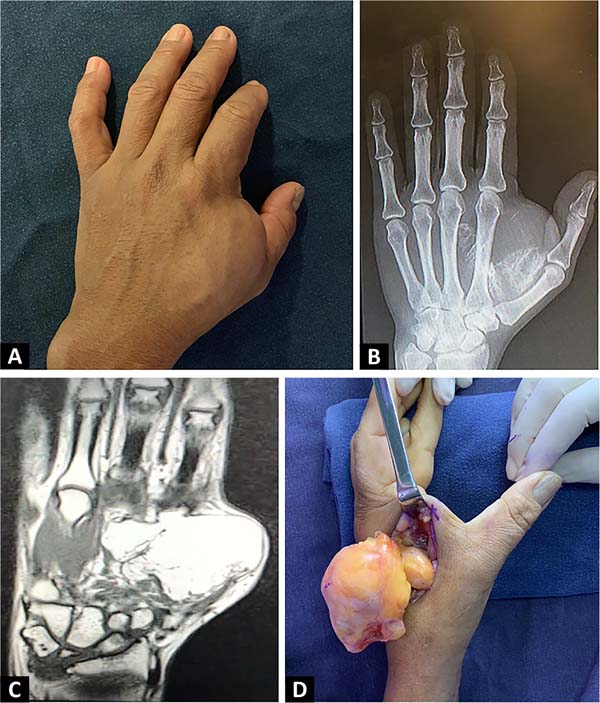
51-year-old female, domestic worker, righthanded. Left hand tumor with 10 years of evolution, slow and progressive growth, without traumatic antecedents. She had pain and paresthesia in the first and second fingers. The examination confirms the presence of a tumor in the first commissure with regular contours, measuring 6 cm in diameter, with a smooth surface and firm elastic consistency, adhered in deep planes and without alterations at the skin level (Figure 1A).
At the level of the digital pulp of the first and second fingers, she presented hypoesthesia with an altered two-point discrimination test, 8 mm, with a negative Tinel sign and no motor alterations. The radiograph showed a tumor with calcifications (Figure 1B). Magnetic resonance imaging showed a polylobulated tumor with well-defined limits, located in the thenar region and at the level of the first interosseous space, deep to the regional muscles, with deep medial extension to the flexor tendons of the second and third fingers. The signal was similar to that of adjacent adipose tissue, with saturation in the fat sat sequence, and presented linear and speckled calcifications in its periphery without contrast enhancement (Figure 1C). The report concluded that it was a lipoma with calcifications without nodular areas of abnormal enhancement. Marginal tumor resection was performed dorsally (Figure 1D).
The postoperative period was uneventful, and the paresthesias disappeared within 48 hours. Pathological anatomy showed a well-defined fat cell tumor due to mesencemática proliferation, composed of mature adipocytes, without atypia or necrosis, accompanied by fibroconnective tracts and focal areas of bone metaplasia. In the 18-month follow-up, she presented a good quality scar, sensitive recovery and no evidence of tumor recurrence.
Clinical case 2
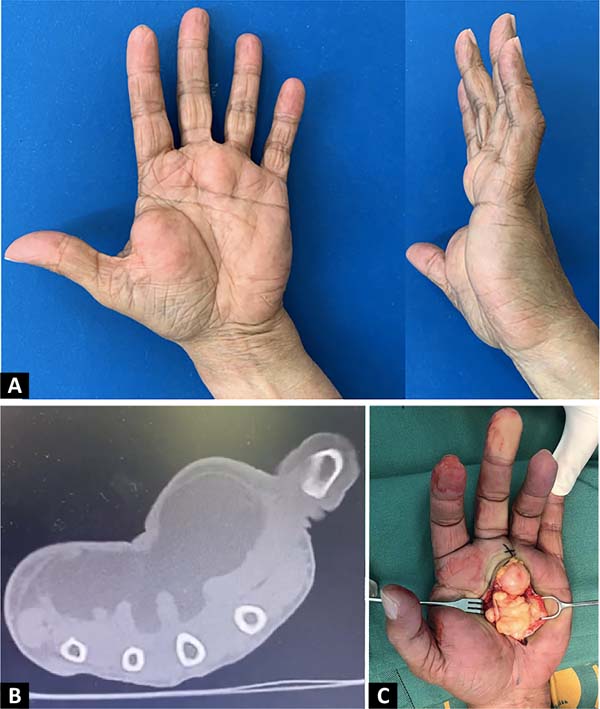
A 60-year-old female with implantable cardioverter-defibrillator colon cancer undergoing chemotherapy. Tumor of the left hand with 1 year of evolution, later added by paresthesias and difficulty in gripping. The examination revealed a polylobulated tumor of firm elastic consistency, topography at thenar eminence, hypothenar eminence, and middle palmar cell at the base of the third and fourth fingers (Figure 2A). Distal sensitivity was normal. Bearing in mind that, because of her history, it was not possible to perform magnetic resonance imaging, a computed tomography scan was requested, which reported a polylobulated tumor with well-defined limits, 70 mm in diameter; of fairly homogeneous fat density, with some thin and dense tracts, located in front of the flexors of the second to fifth fingers, with lobulations that enter between them; with 20mm rounded distal lobulation at the base of the third and fourth fingers (Figure 2B).
Marginal resection was performed with a palmar approach. A well-delimited lipomatous tumor surrounded by a thin capsule was exposed, deep to the superficial palmar aponeurosis. Inside the tumor, the digital nerve of the third invaginated space was identified, which was released by resecting the entire tumor with its capsule (Figure 2C). The postoperative period was uneventful, and the paresthesias disappeared after two days. The pathological anatomy reported a tumor of adipose tissue with a thin capsule and homogeneous section, given by a benign mesenchymal proliferation composed of mature adipocytes with a delicate fibrovascular stroma, with areas of fat necrosis and fibrosis tracts; no lipoblasts, cytonuclear atypia or mitosis. At the 3-month follow-up, she presented an immature scar without new tumors.
Clinical case 3
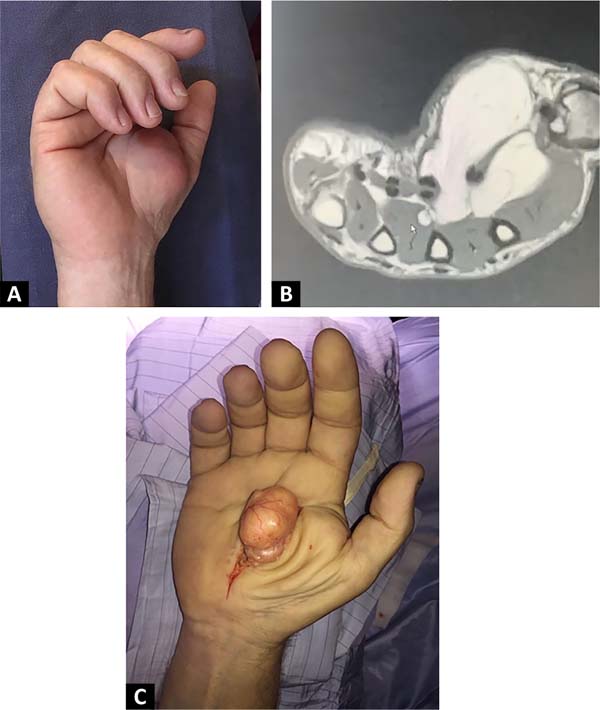
55-year-old male, mechanic, right-handed, hypertensive and smoker. Slow-growing, 10-year-old right hand tumor that, due to its volume, prevented the proper grasping of objects. On examination, he had a tumor on the thenar eminence, with welldefined limits and firm elastic consistency, measuring 6 cm in diameter, without sensory deficit (Figure 3A). Ultrasonography was requested, which showed a solid, heterogeneous, well-defined process, with no evidence of vascularization with Doppler, and its etiology could not be concluded.
The MRI showed a tumor at the level of the superficial thenar eminence to the flexor tendons of the first and second fingers, with an intramuscular extension that interdigitates between the muscles of the first commissure; well delimited, lobulated, with an epicenter at the thenar eminence, measuring 56 mm in its long axis, hyperintense on T1-weighted images, with a diffuse homogeneous drop in its signal in the fat sat sequence; some thin septa, minimal enhancement after contrast administration in the septa and periphery (Figure 3B). With a diagnosis of lipoma, marginal resection was performed via the palmar approach (Figure 3C). The postoperative period was uneventful. A cellulosic specimen was sent to the pathology department, which reported a benign mesenchymal proliferation composed of mature adipocytes without atypia or mitosis.
Clinical case 4
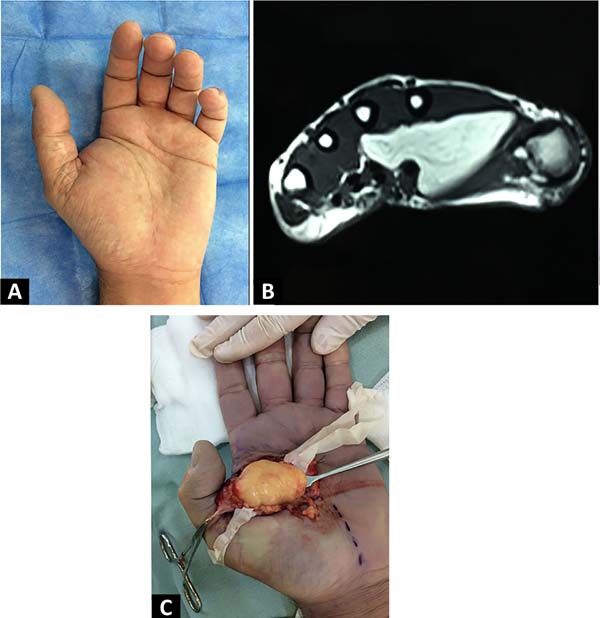
A 62-year-old male, right-handed, retired, with dyslipidemia and Crohn’s disease. A tumor at the level of thenar eminence was noted two months before consultation, without paresthesia or sensory or motor deficits. On examination, he had a firm, elastic, painless tumor in the left hand at the first space level (Figure 4A). Magnetic resonance imaging was performed, which reported a lipomatous, deep, intermuscular tumor between the thenar muscles and the first dorsal interosseous, 50 mm in its greatest diameter, with expansion between the second and third metacarpals and flexor tendons, with well-defined lobulated contours, with a thin capsule and thin septa inside, without contrast enhancement (Figure 4B). Marginal resection was performed with a palmar approach (Figure 4C). Pathological anatomy reported an adipose tumor measuring 55 x 35 x 22mm, homogeneous in section, given by an encapsulated adipose proliferation composed of homogeneous and mature adipocytes and a scarce fibrocollagen stroma without lipoblasts or atypia.
RESULTS
Of the four patients, two were women and two men. Two were operated on at Hospital de Clínicas and two at Hospital Pasteur. The age of presentation was between 51 and 62 years (mean 57 years). Three were deep intramuscular, raised in the thenar region; one was superficial to the regional muscles and occupied the thenar, hypothenar and middle palmar regions. Regarding dimensions, the largest had a major axis of 70mm, while the smallest of 55mm.
All were symptomatic, and only one patient had pain, two patients had paresthesia, one had hypoesthesia, two had difficulty gripping due to the size of the tumor and one was consulted only because of the deformity. Marginal resection was performed in all of them, three via the palmar route and one via the dorsal route. The postoperative period was uneventful in all of them. Paresthesias disappeared in the immediate postoperative period when present, and the patient who presented hypoesthesia returned to normal sensitivity.
Histopathology confirmed typical lipoma in three cases, one with areas of necrosis. In one case, it was a lipoma variant with bone metaplasia or osteolipoma. The mean follow-up was 25.75 months, with no recurrence (Table 1).
| Case | Sex | Age | Location | Dimensions | Symptoms | Treatment | Pathologic anatomy | Controls until | Center of attention |
|---|---|---|---|---|---|---|---|---|---|
| 1 | F | 51 | Thenar region, intramuscular | 62mm x 53mm x 41mm |
Pain, paresthesia, hypoesthesia | Marginal resection, dorsal approach | Lipoma with bone metaplasia | 1 year and 6 months | Hospital de Clínicas |
| 2 | F | 60 | Thenar, hypothenar and middle palmar region, subcutaneous |
70mm x 67mm x 40mm |
Paresthesias, difficulty gripping | Marginal resection, palmar ap- proach |
Typical lipoma with areas of necrosis | 3 months | Pasteur Hospital |
| 3 | M | 55 | Thenar region, intramuscular | 56mm x 53mm x 45mm |
Gripping difficulty | Marginal resection, palmar ap- proach |
Typical lipoma | 3 years | Hospital de Clínicas |
| 4 | M | 62 | Thenar region, intermuscular | 55mm x 35mm x 22mm |
Deformity | Marginal resection, palmar ap- proach |
Typical lipoma | 3 years and 10 months | Pasteur Hospital |
F: female, M: male.
DISCUSSION
Lipoma is the most common soft tissue tumor in adults, but it is rare in hands, where synovial or ganglion cysts are the most common, followed by giant cell tumors 1.
Giant lipomas are those that exceed 5 cm in diameter and are extremely rare in hand, with only individual case reports and small case series in the literature 4-9.
Its location can be subcutaneous or deep subfascial, being the most frequent subcutaneous location. Deep lipomas can be intramuscular, intermuscular or paraosseous when they are on a bone surface 10.
Histologically, it is a well-defined benign tumor of mesenchymal origin composed of mature adipocytes without atypia, but which can be associated with other mesenchymal tissues, configuring variants of lipoma that acquire their name according to the tissue they associate (fibrolipoma, chondrolipoma, osteolipoma, myxolipoma, angiolipoma) 11.
Clinically, they are painless and slow-growing tumors that can cause deformity, symptoms of nerve compression or functional deficits when their volume limits hand mobility 3,12.
The main differential diagnosis of lipomatous tumors larger than 5 cm is an atypical lipoma or welldifferentiated (low-grade) liposarcoma. Differentiation is important because it is a malignant tumor with similar clinical and imaging characteristics, which, although it has no metastatic potential, has a local recurrence rate of 10%, with marginal resection, and can differentiate into high-grade liposarcoma. , requiring strict monitoring 13.
Ultrasound is a diagnostic approach study because it is fast, economical and readily available. On ultrasound, lipomas are well-defined tumors, often isoechoic or hypoechoic concerning the adjacent adipose tissue, with wavy echogenic lines, without acoustic shadowing and minimal or no Doppler signal. Ill-defined margins, non-homogeneous echotexture such as focal nodularity and necrotic areas, and vascularization with Doppler should lead to suspicion of liposarcoma. With an ultrasound compatible with lipoma, when subfascial or larger than 5 cm, it is recommended to extend the evaluation 14.
Magnetic resonance imaging is the imaging test of choice, as it aids in the diagnosis and allows for surgical planning. It is especially indicated in lipomatous tumors larger than 5 cm to differentiate them from low-grade liposarcoma. Gaskin & Helms 15 reported a sensitivity of 100% and specificity of 83% for diagnosing this malignant tumor, with a specificity of 100% for the diagnosis of simple lipoma, which is slightly lower for some lipoma variants as osteolipoma, chondrolipoma, angiolipoma or hibernoma.
Lipomas are seen as well-defined tumors with the same signal intensity as subcutaneous fat in all sequences, signal suppressed in fat suppression sequences, and may have a small number of thin septa (<2mm) or muscle fibers when it is intramuscular. Contrast enhancement is usually not seen except in the fibrous capsule. In contrast, atypical lipomas have large (>2mm) and irregular septa and increased nonadipose content, with intense T2 foci.
Tomography can be useful when magnetic resonance imaging cannot be performed, showing a well-defined hypodense lesion with thin septa without nodular areas or contrast enhancement, which may present calcifications 16. If the clinical-imaging diagnosis is a lipoma, the treatment is excisional biopsy or marginal resection of the lesion with anatomopathological study to confirm the diagnosis. If there is clinical and imaging suspicion of sarcoma, the evaluation should be expanded, and a biopsy performed or referred to a specialized sarcoma service 4,17,18.
Histopathological analysis confirms the diagnosis of lipoma when it shows a proliferation of mature and uniform adipocytes without atypia. On the other hand, low-grade liposarcomas have different sizes of adipocytes and nuclear atypia and are generally positive for the MDM2 gene19.
The prognosis after marginal lipoma resection is good, and recurrence is rare 16,20,21.
CONCLUSION
Giant lipomas of the hand are not common, magnetic resonance imaging is the imaging test of choice, and the curative treatment is surgical with marginal resection and histopathological analysis for diagnostic confirmation. Recurrence is rare.
REFERENCES
1. Tripoli M, Cordova A, Moschella F. Characteristics, Management Techniques, and Outcomes of the Most Common Soft-Tissue Hand Tumors: A Literature Review and Our Experience. Ann Plast Surg. 2017;79(6):558-65. PMID: 28570445 DOI: https://doi.org/10.1097/SAP.0000000000001148
2. Cavit A, Özcanli H, Sançmiş M, Ocak GA, Gürer Eİ. Tumorous conditions of the hand: A retrospective review of 402 cases. Turk Patoloji Derg. 2018;34(1):66-72. PMID: 28984347
3. Cribb GL, Cool WP, Ford DJ, Mangham DC. Giant lipomatous tumours of the hand and forearm. J Hand Surg Br. 2005;30(5):509-12. PMID: 15992974 DOI: https://doi.org/10.1016/j.jhsb.2005.05.002
4. Chatterton BD, Moores TS, Datta P, Smith KD. An exceptionally large giant lipoma of the hand. BMJ Case Rep. 2013;2013:bcr2013200206. DOI: 10.1136/bcr-2013-200206 PMID: 23839616 DOI: https://doi.org/10.1136/bcr-2013-200206
5. Bocchiotti MA, Lovati AB, Pegoli L, Pivato G, Pozzi A. A case report of multi-compartmental lipoma of the hand. Case Reports Plast Surg Hand Surg. 2018;5(1):35-8. PMID: 29736408 DOI: https://doi.org/10.1080/23320885.2018.1469988
6. Iyengar KP, Matar HE, Loh WY. Giant hand lipoma invaginating the thenar muscles. BMJ Case Rep. 2014;2014:bcr2014203963. DOI:10.1136/bcr-2014-203963 PMID: 24663254 DOI: https://doi.org/10.1136/bcr-2014-203963
7. Ribeiro G, Salgueiro M, Andrade M, Fernandes VS. Giant palmar lipoma - an unusual cause of carpal tunnel syndrome. Rev Bras Ortop. 2017;52(5):612-5. PMID: 29062828 DOI: https://doi.org/10.1016/j.rbo.2016.08.003
8. Papakostas T, Tsovilis AE, Pakos EE. Intramuscular Lipoma of the Thenar: A Rare Case. Arch Bone Jt Surg. 2016;4(1):80-2. PMID: 26894225
9. Yadav SP, Jategaonkar PA, Haldar PJ. Giant hand lipoma revisited: report of a thenar lipoma & its literature review. J Hand Microsurg. 2016;5(2):84-5. PMID: 24426682 DOI: https://doi.org/10.1007/s12593-013-0093-3
10. Bancroft LW, Kransdorf MJ, Peterson JJ, O’Connor MI. Benign fatty tumors: classification, clinical course, imaging appearance, and treatment. Skeletal Radiol. 2016;35(10):719-33. DOI: https://doi.org/10.1007/s00256-006-0189-y
11. Fletcher CDM, Bridge JA, Hogendoorn PCW. WHO Classification of Tumors of Soft Tissue and Bone. 4th ed. Lyon: IARC Press; 2013.
12. Balvís-Balvís P, Yañez-Calvo J, Castro-Menéndez M, Ferreirós-Conde MJ. Giant Lipomas of the Hand. Our Experience. Rev Iberam Cir Mano. 2020;48:72-8. DOI: https://doi.org/10.1055/s-0040-1716559
13. Cair Cairncross L, Snow HA, Strauss DC, Smith MJF, Sjokvist O, Messiou C, et al. Diagnostic performance of MRI and histology in assessment of deep lipomatous tumours. Br J Surg. 2019;106(13):1794-9. DOI: https://doi.org/10.1002/bjs.11309
14. Wagner JM, Rebik K, Spicer PJ. Ultrasound of Soft Tissue Masses and Fluid Collections. Radiol Clin North Am. 2019;57(3):657-69. PMID: 30928084 DOI: https://doi.org/10.1016/j.rcl.2019.01.013
15. Gaskin CM, Helms CA. Lipomas, lipoma variants, and welldifferentiated liposarcomas (atypical lipomas): results of MRI evaluations of 126 consecutive fatty masses. AJR Am J Roentgenol. 2004;182(3):733-9. PMID: 14975977 DOI: https://doi.org/10.2214/ajr.182.3.1820733
16. Ingari JV, Faillace JJ. Benign tumors of fibrous tissue and adipose tissue in the hand. Hand Clin. 2004;20(3):243-8. PMID: 15275683 DOI: https://doi.org/10.1016/j.hcl.2004.03.013
17. Johnson CN, Ha AS, Chen E, Davidson D. Lipomatous Soft-tissue Tumors. J Am Acad Orthop Surg. 2018;26(22):779-88. PMID: 30192249 DOI: https://doi.org/10.5435/JAAOS-D-17-00045
18. Leclère FM, Casoli V, Pelissier P, Vogt PM, Desnouveaux E, Spies C, et al. Suspected adipose tumours of the hand and the potential risk for malignant transformation to sarcoma: a series of 14 patients. Arch Orthop Trauma Surg. 2015;135(5):731-6. PMID: 25736165 DOI: https://doi.org/10.1007/s00402-015-2170-5
19. Hameed M. Pathology and genetics of adipocytic tumors. Cytogenet Genome Res. 2007;118(2-4):138-47. PMID: 18000364 DOI: https://doi.org/10.1159/000108294
20. Ozcanli H, Ozaksar K, Cavit A, Gurer EI, Cevikol C, Ada S. Deep palmar tumorous conditions of the hand. J Orthop Surg (Hong Kong). 2019;27(2):2309499019840736. DOI: https://doi.org/10.1177/2309499019840736
21. Lichon S, Khachemoune A. Clinical presentation, diagnostic approach, and treatment of hand lipomas: a review. Acta Dermatovenerol Alp Pannonica Adriat. 2018;27(3):137-9. PMID: 30244263 DOI: https://doi.org/10.15570/actaapa.2018.27
1. Hospital Pasteur, Servicio de Cirugía Plástica y Microcirugía, Montevideo, Uruguay
2. Hospital de Clínicas, Cátedra de Cirugía Plástica, Reparadora y Estética, Montevideo,
Uruguay
Corresponding author: Maria Eugenia Torres Larravide, nº 2.458, Montevideo, Uruguay Zip Code: 11400, E-mail: mariaeugeniatorres@outlook.com
Article received: February 17, 2021.
Article accepted: April 19, 2021.
Conflicts of interest: none.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter