

Original Article - Year 2022 - Volume 37 -
Inferior pedicle nasolabial flap in nasal ala reconstruction
Retalho nasogeniano de pedículo inferior na reconstrução de asa nasal
ABSTRACT
Introduction: The nasal alar has always been a major reconstructive diflculty, and in the search for a flap with skin characteristics similar to this one, we came across the inferiorly based nasolabial flap. The objective of this study was to demonstrate the viability of the proposed flap for reconstruction of the nasal alar after removal of skin tumors.
Methods: This study analysed twenty cases of inferiorly based nasolabial flap performed with the same surgical technique in the period between 2008-2019 and followed up for one year of postoperative.
Results: Of the 20 studied cases, 13 (65%) did not present complications, being the most described: partial defect coverage and partial disappearance of the nasolabial sulcus.
Conclusion: The inferiorly based nasolabial flap proved to be a viable flap for nasal alar reconstruction due to the quality of the skin, easy execution, and minimal complication rates.
Keywords: Skin neoplasms; Carcinoma, basal cell; Surgical flaps; Nasal surgical procedures; Reconstructive surgical procedures.
RESUMO
Introdução: A asa nasal sempre foi uma grande dificuldade reconstrutiva e, na busca de um retalho com características da pele semelhantes a esta, deparamos com o retalho nasogeniano de pedículo inferior. O objetivo do trabalho foi demonstrar a viabilidade do retalho proposto para reconstrução da asa nasal após a retirada de tumores cutâneos.
Métodos: Foram analisados 20 casos de retalho nasogeniano de pedículo inferior realizados com a mesma técnica cirúrgica no período entre 2008 e 2019 e acompanhados por um ano de pós-operatório.
Resultados: Dos 20 casos estudados, 13 (65%) não apresentaram complicações, sendo as mais relatadas: cobertura parcial do defeito e desaparecimento parcial do sulco nasogeniano.
Conclusão: O retalho nasogeniano de base inferior mostrou ser um retalho viável à reconstrução da asa nasal pela qualidade de pele, fácil execução e índices mínimos de complicações.
Palavras-chave: Neoplasias cutâneas; Carcinoma basocelular; Retalhos cirúrgicos; Procedimentos cirúrgicos nasais; Procedimentos cirúrgicos reconstrutivos
INTRODUCTION
The first descriptions of flaps in the history of plastic surgery (6th century BC) were for nasal reconstruction in ancient India; the technique became known as the mid-frontal flap or the Indian method. Gaspare Tagliacozzi, in 1597, described a new option for nose reconstruction: a direct cutaneous flap of the upper limb called the Italian method1. Dieffenbach described the nasolabial flap and Converse the scalp flap based on the superficial temporal artery2-4.
The nasal ala has always been a major reconstructive difficulty due to its thin skin, which, after being reconstructed, normally required surgical refinements for a better appearance. Looking for an alternative to correct these defects, in which the skin would present similar characteristics of the nasal ala and allow reconstruction in a single surgical procedure, we came across the nasolabial flap with an inferior pedicle.
OBJECTIVE
To demonstrate the viability of the inferior nasolabial flap for nasal ala reconstruction after removal of skin tumors.
METHODS
The study was carried out with primary data obtained from a retrospective study of 20 cases of nasal alar reconstruction using an inferior pedicle nasolabial flap, after removal of basal cell carcinoma, in the period between 2008 and 2019. The patients were operated on at the Hospital de Câncer de Campo Grande Alfredo Abrao, MS. The results of the immediate postoperative period were analyzed, with seven, 30 and 90 days after surgery and after 1 year and the occurrence or not of complications.
We selected the cases of patients with tumors restricted to the nasal ala, who had been previously biopsied with a positive diagnosis for basal cell carcinoma and who agreed to sign the Free and Informed Consent Form. The Ethics Committee approved the study of the Hospital de Câncer de Campo Grande Alfredo Abrão (n.º 002.2021).
Surgical technique
After demarcating the tumor with oncological safety margins with methylene blue, the tumor area was anesthetized with modified Klein’s solution [100 ml of 0.9% SF + 1 ampoule of adrenaline (millesimal solution) + 20 ml of lidocaine at 2 % (without vasoconstrictor) + 4 ml of 8.4% Na+ bicarbonate] + infraorbital nerve block associated with sedation with midazolam and fentanyl performed by the anesthesiologist.
After vasoconstriction, the tumor was resected, and rigorous hemostasis of the excised area was performed.
The search for thin skin, similar to that of the nasal ala, led us to use the skin of the lateral nasal dorsum. We demarcated the flap to be made, extending from the nasal ala to the inner corner of the eye, preserving the area of the internal canthal ligament and the lacrimal duct. Then, we made the inferior pedicle nasolabial skin flap (Figure 1A) and rotated it to its new bed (Figure 1B), in which it was sutured with 5.0 nylon. After slight detachment and hemostasis, the donor area was sutured with 4.0 vicryl and 5.0 nylon, generating a scar without tension (Figure 1C).
The excised tumor was sent for anatomopathological examination to confirm the safety margins.
RESULTS
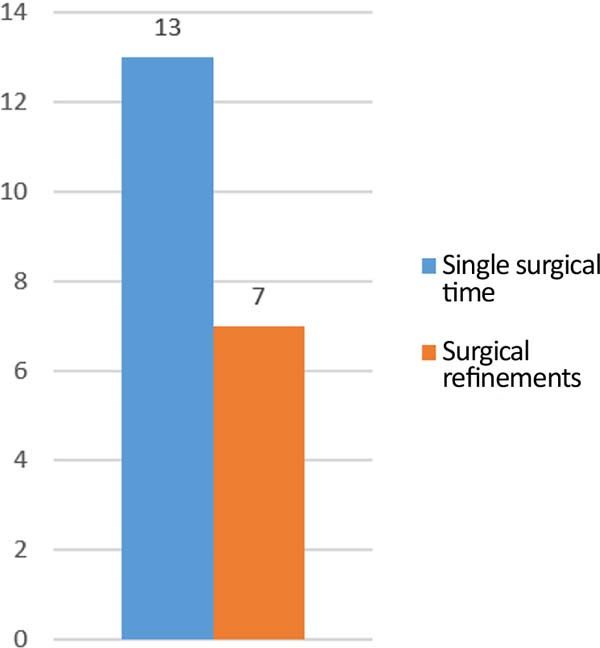
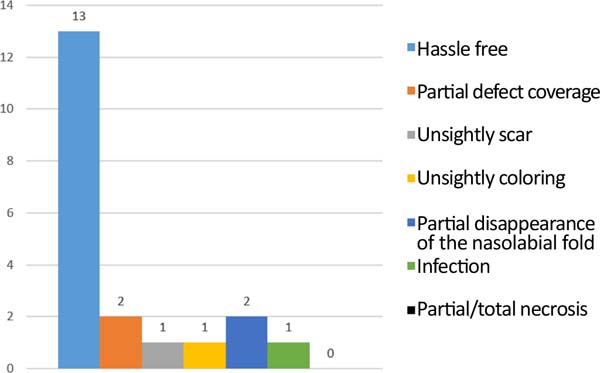
During 11 years, 20 cases of patients needing nasal ala reconstruction after basal cell carcinoma excision were analyzed and operated on, 13 (65%) were male, and 7 (35%) were female. The age of the patients ranged between 45 and 80 years, with 50% in the age group from 61 to 70 years. All patients presented Fitzpatrick between I and III. Only 7 (35%) required refinements for the operated patients, performed in only one additional surgical time (Figure 2). In the immediate postoperative period, two patients had partial coverage of the defect, and another two patients had complications, one being an infection and the other an unsightly staining of the flap.
At the consultation after 60 days, one patient evolved with an unsightly scar, and two had partial disappearance of the nasolabial fold. In the follow-up up to one year after the surgeries, thirteen patients (65%) did not present any complications, and no patient evolved with necrosis (Figure 3).
Figures 4 and 5 illustrate the surgical technique, and Figures 6 and 7 illustrate the long-term follow-up of some cases in the series.
DISCUSSION
In the literature, there is a large arsenal described for nose reconstruction. However, due to its limits and concave shape, the nasal ala represents a challenge for the surgeon to preserve its function allied to a satisfactory aesthetic result.
Some authors reported the bilobed flap (44%) as the most used for this nasal subunit (nasal wing), followed by the VY flap and the superior pedicle nasolabial flap5; other authors reported a predominance of the use of the superior pedicle nasolabial flap (55.84%)6,7. In the present study, we did not find, in the literature, a case series of the inferior pedicle nasolabial flap to serve as a comparison with our work.
The inferior pedicle nasolabial flap is based, in the design, on the Limberg rhomboid flap. This one, which considers the resection area as a diamond, proposes making the flap parallel to one of the four axes of the lesion, making the “V” of the donor area close by approximation when rotating the flap. The inferior pedicle nasolabial flap, in essence, is the Limberg flap designed in the most suitable axis for the correction of the nasal ala defect.
Skin thickness is one of the limiting factors for the reconstruction to be aesthetically similar to that of the nasal ala. The mid-frontal flap is an option for major reconstructions that encompass more than half of the nose, including the nasal wings, being described as the most appropriate for safety, amount of skin obtained and similarity in skin characteristics8; however, it requires several refinement surgeries in Caucasian patients for esthetic improvement due to the thickness of this flap. Despite its limited coverage area, the inferior pedicle nasolabial flap, being restricted to defects in the nasal ala, presented a skin thickness practically compatible with the anterior thickness, not requiring refinements to thin the flap in 70% of the cases performed.
According to Gokrem et al.9, the VY myocutaneous advancement flap is an option for nasal reconstruction of small and medium defects, avoiding the disadvantages of the frontal flap and presenting the advantages of safety and similar characteristics between the donor and recipient areas, and can be used in various regions of the nose. However, it requires great experience from the surgeon to guarantee the viability of this flap due to the narrow pedicle. In contrast, the inferior pedicle nasolabial flap is easy to make, not requiring great experience on the surgeon’s part to perform it.
According to Laitano et al.5, the bilobed flap has the advantage of being a simple procedure, performed in a single stage, with good aesthetic and functional results and a high degree of patient acceptance, unlike the superior pedicle nasolabial flap. The bilobed flap for nasal alar reconstruction showed the same specificities compared to the inferior pedicle nasolabial flap.
The interpolation flap for nasal ala correction, cited by Sakai et al.10, promotes the preservation of the nasolabial fold; however, when the patient is male, hair follicles may be transferred, which does not happen with the inferior pedicle nasolabial flap because their skin does not contain hair follicles.
CONCLUSION
The inferior base nasolabial flap proved to be a viable flap for nasal ala reconstruction due to the quality of the skin, easy execution and minimal complication rates.
| COLLABORATIONS | |
|---|---|
| MR | Conception and design study, Final manuscript approval, Methodology, Realization of operations and/or trials, Supervision, Writing - Review & Editing |
| DNS | Analysis and/or data interpretation, Final manuscript approval, Writing - Review & Editing |
| ALCL | Analysis and/or data interpretation, Final manuscript approval, Visualization, Writing - Original Draft Preparation, Writing - Review & Editing |
| ALCL | Final manuscript approval, Writing - Original Draft Preparation, Writing - Review & Editing |
| ACR | Analysis and/or data interpretation, Final manuscript approval, Writing - Review & Editing |
1. Campo Grande Alfredo Abrao Cancer Hospital, Plastic Surgery Service, Campo Grande,
MS, Brazil.
2. Federal University of Mato Grosso do Sul, Plastic Surgery, Campo Grande, MS, Brazil.
3. State University of Mato Grosso do Sul, Medicine, Campo Grande, MS, Brazil.
4. Anhanguera-Uniderp University, Medicine, Campo Grande, MS, Brazil.
5. University of Marília, Medicine, Marília, SP, Brasil.
Corresponding author: Marcelo Rosseto, Rua Raul Pires Barbosa, 1477, Chácara Cachoeira, Campo Grande, MS, Brazil, Zip Code 79040-150, E-mail: marcelorosseto@yahoo.com.br
















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter