

Articles - Year 1997 - Volume 12 -
Giant Dermatofibrosarcoma Protuberans
Dermatofibrossarcoma Protuberans Gigante
ABSTRACT
Dermatofibrosarcoma protuberans is arare malignant skin tumor; locally aggressive. It has a high raie of local recurrence but metastasis is very rare. Aggressive excision is required with a surgieal margin of at least 3 cm. The authors analyse a remarcable case weighing 3850 g and measuring 28 x 23 x 16 cm) on the upper limb of a male patient, treated at the Plastic Surgery Service of the Hospital Universitário Clementino Fraga Filho (UFRJ) in 1993. A retrospective study of this pathology) performed at the same Service between January 1984 and May 1994) detected other four casessited in different areas of the body and which were also surgically treated. Using data from the pertinent literature, the authors discuss the etiopathogenic aspects and the treatment methods of this tumor which, in addition to its rarity, presents special characteristics as to size, malignity and evolution.
Keywords:
RESUMO
O "Dermatofibrossarcoma protuberans" é um raro tumor cutâneo maligno, localmente agressivo, com elevada recidiva local, mas que raramente dá metástases. Apresentamos análise de caso gigante em membro superior, medindo 28 x 23 x 16 cm e pesando 3.850 gramas, tratado no serviço de Cirurgia Plástica do Hospital Universitário Clementino Fraga Filho - UFRJ, em 1993. Um estudo restropectivo desta patologia em nosso serviço, entre janeiro de 1984 e maio de 1994, constatou outros quatro casos localizados em diferentes regiões do corpo tratados cirurgicamente. Através de dados da literatura discutimos os aspectos etiopatogênicos e as suas formas de tratamento deste tumor que, além de raro, possui características especiais quanto ao tamanho, malignidade e evolução.
Palavras-chave:
Dermatofibrosarcoma protuberans was described for the first time in 1924 by Darier and Ferrand, who recognized it as a clinical entity and named it "Progressive Recurrent Dermatofibroma" or "Skin Fibrosarcoma" (2). In 1925, Hoffman was the first to utilize the term "Dermatofibrosarcoma protuberans" (5). The diagnosis was based on the patient's clinical history and the macroscopic aspects of the lesion until 1962, when Taylor and Helwig thoroughly described its microscopical characteristics(12).
This kind of sarcoma represents 0.1% of all malignant tumors(1).
Rutgers and colleagues, in 1992, presented an extensive literature review with 913 cases. In this report, the primary size of the tumor ranges from 1 to 8 cm(9). Taylor and Helwig (1962), in a series of 115 cases, describe the largest tumor as presenting a 12 cm diameter(12).
The tumor histopathogenesis is quite controversial. Histological and ultrastructural data and tissue cultures point to a fibrohistiocytic origin(7, 12). Others have suggested a neurogenic derivation, based on morphological characteristics and electron microscopy(3, 4). Recent citogenetic studies associate this pathology with chromosomal aberrations(11).
The tumor presents a localiy aggressive behaviour and infiltrative growth. Local recurrences are freguent but the metastasis are rare. It may affect any area of the body; particularly the thorax and proximal extrernities, and is more freguent in males between the second and fifth decades in life.
The case described in this work was chosen on account of its characteristics as a giant tumor which rapidly reached extremely large dimensions in an upper limb. The tumor occurrence on limbs determines major hindrances, due to the circulatory problems it may cause and the difficult covering of the bloody area after the tumor removal.
CASE REPORT
A.C.S., 38, male, sought our Service in October 1992, presenting a primary multinodular tumor at the proximal third of the right upper limb. The clinical picture had begun 30 months ago with a small hardened cutaneous nodule, which evolved slowly during 12 months. After this period the lesion began to grow rapidly and became vegetative, in a torus formation, erythematous, friable, partially covered by a fetid seropurulent secretion, with some uleerations, small neerose areas and increased local vascularization. At the patient's first visit to our Service the tumor had 28 x 23 x 16 em in measure and 3,850 grams in weight (fig. 1).

Fig. 1 - View of the ulcerated lesion, with 28 x 23 x 16 cm in measure and which weighed, after being removed, 3850 g. Intense colateral circulation, as it can be observed at the arm internal side and at the clavicular area.
In June 2nd, 1993 an arteriography was performed, showing a hypervascularized mass nourished mainly by the first muscular branch of the right brachial artery.
In July 16, 1993, the embolization of the two arterial pedicles which nourished the tumoral mass was performed with a polyvinylic alcohol sponge and two metallic springs, one at each pedicle (fig. 2). The tumor volume was moderately reduced and its turgescence was markedly reduced.

Fig. 2 - Another view of the tumor, with the catheter introduced in the subclavian artery to perform the nourishing vessels embolization.
In July 19, 1993, an ample resection of the lesion was performed with peripherical margins of 2 cm, reaching, in depth, the subaponeurotic plan and partially including the deltoid muscle and the aponeurosis of the biceps and triceps, which were adhered to the tumor (figs. 3 & 4).

Fig. 3 - Immediate post-operative period, showing the extension of the resection which partially included the deltoid muscle.

Fig. 4 - A strip of sane skin remained at the arm internal side, protecting the limb vasculoneural bundle.
Daily dressings were made on the bloody area with an antiseptic (hexachlorophene) and uncture (collagenase), providing a satisfactory growth of granulation tissue. However, two months after the surgery and before the bloody area healing, the patient moved to another address and stopped coming to the ambulatorial control. Only in June 1994 it was possible to find out his whereabouts; he was in good conditions, with the bloody area completely healed, with no important functional restrictions and no signs of tumor recurrence (figs. 5 & 6).

Fig. 5 - After one year post-operative, the area completely healed by second intention, with no local recurrences nor metastasis.

Fig. 6 - View of the arm posterior side, showing only a discreet restriction of the arm raising beyond the horizontal plane.
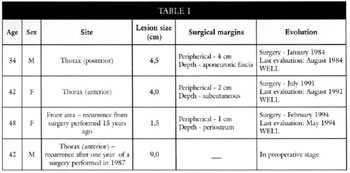
In a retrospective study of the period comprised between January 1984 and May 1994, other four cases of dermatofibrosarcoma protuberans were detected; these cases are analysed in Table I.
DISCUSSION
The most extensive literature reviews were performed by Taylor and Helwig in 1962 (115 cases) and by Rutgers and colleagues in 1992 (913 cases). The largest tumor described had a 12 em diameter. The case reported in this work presented dimensions of 28 x 23 x 16 cm, representing, for what it seems, the largest volume already described in the literature for this type of tumor.
The "Dermatofibrosarcoma protuberans" histopathogenesis is controversial. The first references as to its origin were made in 1962 by Taylor and Helwig, who analysed the histological characteristics of 115 cases and stated that the pathology origin was fibrohistiocytic(12). In 1976, by means of a tissue culture and an ultrastructural study, Ozzelo and Hamels expressed the same opinion(7). However, with an extensive study by electron microscopy, Hashimoto and colleagues (1974) suggested that the main cell originates from a neural cell modified as endoneural or perineural cell(4). In 1985, Fletcher and colleagues corroborated this hypothesis(6), Stephenson and colleagues associated the tumor with the trisomy of the chromosome 7 and chromosomal ring(ll), but suggested additional studies might be performed to determine these data significance, for the citogenetic knowledge of the pathology in the literature is quite limited.
As to the patients' most affected body areas and age, the authors' observations, in their majority, are uniform(1, 6, 9, 12), etecting a greater incidence on the thorax, followed by the limbs proximal extremities and, less frequently, the head and neck, in patients between 20 and 50 years in age. In our casuisty, however small, we have observed the same prevalence.
Rutgers and colleagues and Lanskin report a slight prevalence on the male sex(6, 9), while Bendix-Hansen and colleagues have detected the same frequency on both sexes(1).
The local recurrence index is of about 50%, even after the adequate excision of the lesion. Rutgers and colleagues and Lanskin observe that surgical margins wider than 3 cm cause this index to drop to 20 - 30%(6, 9). Smola and colleagues, on their turn, suggest the aponeurotic fascia resection to minimize the recurrences(10).
The metastasis are rare (5% of the cases). In accordance with the studies of Platil and colleagues, the dissemination occurs hematogenically (4%) and lynphatically for regionallynphatic ganglia (1%), occurring between 7 and 15 years after the primary tumor coming out(8). For Lanskin(6), the lung is the preferred target (80%), with less common occurrences in the brain, bones, heart and pancreas. According to these authors, the metastasis are more frequent after multiple local recurrences.
In our casuisty, only one patient was controlled for 12 months after surgery, and he did not present local recurrences nor metastasis. As to the giant tumor case, after one year the patient was well, even without medical follow-up and with the bloody area healed by second intention. In accordance with our patients' characteristics, this generally occurs because they are feeling well and do not want to be absent from work or have transportation expenses "just to be seen by the doctor". In case of recurrence, they will undoubtely come back.
As far as the treatment is concerned, the authors unanimously advise local surgical resection with peripherical margins of 2-3 cm, including the subjacent fascia. We have opted for the same procedure, but in infiltrative lesions the resection must go beyond the fascia as far as necessary.
The preoperative embolization of the tumoral mass was indicated only for the giant tumor, reducing significantly its size and turgescence and facilitating the surgical act with minimal bleeding.
In a conjoint evaluation with our hospital Oncology Service, we have opted not to use radiotherapy as adjuvant or therapeutic procedure. Referring to the literature, we have found out that the radiotherapy role is still undefined. The authors whose works we have used in our research emphatically state that the "Dermatofibrosarcoma protuberans" cases treated with radiotherapy did not present any response(1, 9, 12). Among them, only Taylor and colleagues consider that readiotherapy may represent a therapeutic alternative in unresectionable lesions(12).
REFERENCES
1. BENDIX-HANSEN, K., MYHRE-IENSEN, 0., KAAE, S. Dermatofibrosarcoma protuberans: A clinico-pathological study of nineteen cases and review of the world literature. Scand. J. Plast. Reconstr. Surg. 17:247-252, 1983.
2. DARIER, J.; FERRAND, M. Dermatofibromes progressifs et recidivants ou fibrosarcomes de la peau. Ann. de Dermat. 6:545-62, 1924.
3. FLETCHER, C. D.; EVANS, B. J.; MACARTNEY, J. C. Dermatofibrosarcoma protuberans: a clinico-pathological and immunohistochemical study with a review of the literature. Histopathology 9:921-938, 1985.
4. HASHIMOTO, K.; BROWNSTEIN, M. H.; JAKOBIAC, F. A. Dermatofibrosarcoma protuberans. Arch. Dermatol. 110:874-885, 1974.
5. HOFFMAN, E. Uber das Knollentreibende Fibrosarkon der Haut (Dermatofibrosarcoma protuberans). Dermat. Zeitschn 43:1-8, 1925.
6. LANSKIN, W B. Dermatofibrosarcoma protuberans. Cancer journal for Clinicians 42(2):116-125,1992.
7. OZZELO, L.; HAMELS, J. The Histiocytic Nature of Dermatofibrosarcoma protuberans - Tissue culture and electron microscopic study. Am. J. Clin. Pathol. 65:136-148, 1976.
8. PATIL, P. K.; PATEL, S. G.; KRISHNAMURTHY, S.; MISTRY, R. C., DESPHANDE, R. K. AND DESAI, P. B. Dermatofibrosarcoma protuberans Metastatic to the Lung. A case report. Tumori 78:49-51, 1992.
9. RUTGERS, E. J.; KROON, B. B.; ALBUS-LUTTER, C. E.; GORTZAK, E. Dermatofibrosarcoma protuberans: Treatment and prognosis. European journal of Surgical Oncology 18:241-248, 1992.
10. SMOLA, M. G.; SOYER, H. P.; SCHARNAGL, E. Surgical Treatment of Dermatofibrosarcoma protuberans. A retrospective study of 20 cases with review of literature. European journal of Surgical Oncology 17:447-453, 1991.
11. STEPHENSON, C. E; BENGER, C. S.; LEONG, S. P. L.; DAVIS, J. R. AND SANDBERG, A. A. Ring Chromosome in a Dermatofibrosarcoma protuberans. Cancer Genet. Cytogenet. 58:52-54, 1991.
12. TAYLOR, H. B.; HELWIG, E. B. Dermatofibrosarcoma protuberans: A Study of 115 cases. Cancer 15:717-725, 1962.
I - Staff members, Plastic Surgery Service of the Hospital Universitário Clementino Fraga Filho, UFRJ
II - Residem physicians, Plastic Surgery Service of the Hospital Universitário Clementino Fraga Filho, UFRJ
III - Chief, Plastic Surgery Service of the Hospital Universitário Clementino Fraga Filho, UFRJ
Adress for Correspondence:
Talita Franco, MD
Rua Ramon Franco, 98 - Urca
22290-290 - Rio de Janeiro - RJ - Brazil
Work performed by the Plastic Surgery Service of the Hospital Universitário Clementino Fraga Filho, UFRJ


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter