INTRODUCTION
The eccrine poroma is a benign lesion, usually solitary, which presents as a sessile
or pedicled nodule of skin color and most often affects the palm or plant of the foot.
It derives from the intradermal component of the eccrine sudoriparous duct1,2. Due to its rarity, the pigmented variant can easily be confused with melanoma, in
addition to other tumor lesions. Thus, dermatoscopy is an important tool to aid in
diagnosing, but only histology can define it. A clinical case of pigmented poroma
on the scalp is reported, a location considered atypical, simulating malignant melanoma.
CASE REPORT
A 73-year-old male patient, phototype IV on the Fitzpatrick Scale, has a personal
history of hypertension, diabetes, arrhythmia, chronic non-dialysis renal failure,
gout, and previous coronary angioplasty with the placement of 4 stents and stroke
10 years ago. He informed the appearance of painless scalp injury, growing in the
last 6 months, associated with sporadic bleeding and healing difficulty.
He sought care with a dermatologist, and some diagnostic hypotheses of tumor lesion
subtypes were suggested, being the main melanoma nodular. On dermatological examination,
the lesion presented as a blackened nodule with an erythematous center of firm consistency,
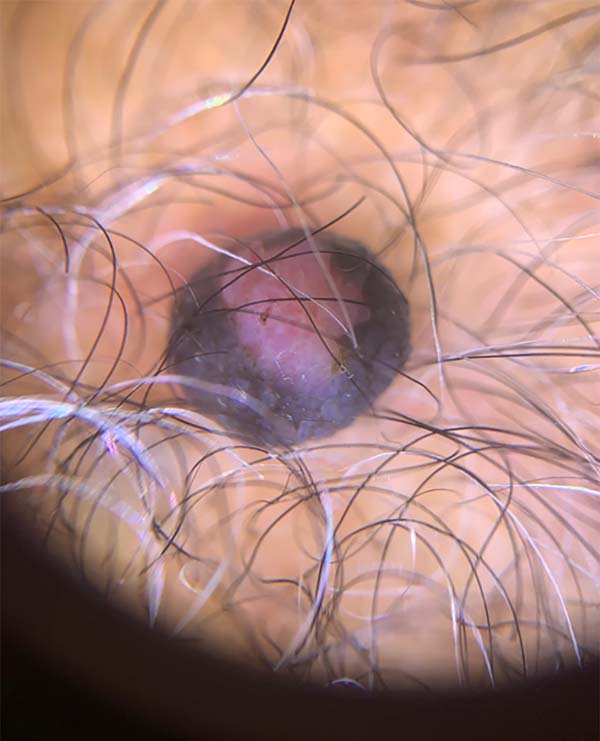
measuring approximately 1.5 cm in diameter (Figure 1). The dermoscopic examination showed a circumscribed nodule with blackened edges
and a center with a predominant vascular pattern in blood cells (Figure 2).
Figure 1 - Blackened nodule with erythematous center on the scalp.
Figure 1 - Blackened nodule with erythematous center on the scalp.
Figure 2 - Dermatoscopy evidencing circumscribed nodule with blackened edges and center with
predominant vascular pattern in blood cells.
Figure 2 - Dermatoscopy evidencing circumscribed nodule with blackened edges and center with
predominant vascular pattern in blood cells.
It was decided to perform exeresis with minimal margins. The material was referred
for pathological study, whose report was partially pigmented eccrine poroma with surgical
margins free of neoplasia. The clinical hypothesis of malignant melanoma was ruled
out, and the patient is under outpatient follow-up, with no signs of recurrence to
date.
DISCUSSION
Pinkus was the first to describe the eccrine Poroma in 19562. This benign neoplasm appears as a firm nodule, pediculated or not, being more common
in the palmar or plantar region. It may grow in weeks or years and is more frequent
between the fourth and sixth decades of life3,4. It has no predilection for sex or race, except for the pigmented variant, which
affects slightly more black people5.
The term poroma refers to rare cutaneous attached tumors, in which its structure presents
cells similar to those of the acrosyringium. Clinical variants include poromatosis,
linear and pigmented eccrine poroma6. Its pathophysiology is unknown, but it is related to trauma, radiation or scarring7.
Due to the rarity of this lesion, there are few studies and cases published in the
literature. It can often be clinically confused with seborrheic keratosis, pyogenic
granuloma, basal cell carcinoma, squamous cell carcinoma, angiofibroma, or melanoma.
For these reasons, it is considered a “great simulator,” and other tools can be used
as a diagnostic aid, such as dermatoscopy and confocal microscopy 8,9, but there is no consensus on the findings.
Minagawa and Koga, in 20106, described 12 cases of pigmented eccrine poroma in which
dermoscopy had some structural patterns, the most common being the vascular pattern,
with polymorphic, arboriform and staple vessels. Since the eccrine poroma can simulate
several benign and malignant tumors on the dermatoscopic aspects, the authors state
that it is important to consider the possibility of pigmented eccrine poroma in cases
of pigmented lesions that present non-melanocytic patterns in dermatoscopy.
The poroma’s main histopathological finding is a circumscribed and compact proliferation
of cuboidal keratinocytes that present monomorphic nuclei and eosinophilic cytoplasm.
In this clinical case, after dermatological examination and dermoscopic evaluation,
the main diagnostic hypothesis was malignant melanoma. The few clinical cases published
with a dermatoscopic study presented a similar history and diagnostic doubt, and the
diagnosis was clarified only after histopathological evaluation8,10.
The choice of treatment, in this case, was surgical excision, considered the gold
standard. However, there are other therapeutic options as an alternative, including
shaving or electrocautery. Because it is a benign lesion, the eccrine poroma has a
good prognosis, with a very low recurrence rate.
CONCLUSION
It is concluded that it is important that the evaluation of pigmented skin lesions
is done both clinically and with dermatoscopy, used as a tool that corroborates the
diagnosis. Although eccrine poroma is a rare tumor, it should be considered a diagnostic
hypothesis in cases where pigmented lesions do not have melanocytic characteristics,
and the diagnosis is confirmed only after histopathological evaluation.
REFERENCES
1. Mélega JM. Cirurgia plástica fundamentos e arte. Rio de Janeiro: MEDSI; 2002.
2. Goldman P, Pinkus H, Rogin JR. Eccrine poroma; tumors exhibiting features of the epidermal
sweat duct unit. AMA Arch Derm. 1956 Nov;74(5):511-21.
3. Abenoza P, Ackerman AB. Ackerman's histologic diagnosis of neoplastic skin diseases.
Philadelphia: Lea and Febiger; 1990.
4. Rivera OL, Mora S, Gutiérrez RM, Novales J. Poroma ecrino simulando un melanoma maligno.
Reporte de un caso y revisión de la literatura. Rev Cent Dermatol Pascua. 1999;8(1):35-8.
5. Hu SCS, Chen GS, Wu CS, Chai CY, Chen WT, Lan CCE. Pigmented eccrine poromas: expression
of melanocyte-stimulating cytokines by tumor cells does not always result in melanocyte
colonization. J Eur Acad Dermatol Venereol. 2008;22(3):303-10. DOI: https://doi.org/10.1111/j.1468-3083.2007.02406.x
6. Minagawa A, Koga H. Dermoscopy of pigmented poromas. Dermatology. 2010;221:78-83.
DOI: https://doi.org/10.1159/000305435
7. Avilés-Izquierdo JA, Velàzquez-Tarjuelo D, Lecona-Echevarria M, et al. Dermoscopic
features of eccrine poroma. Acta Dermosifiliogr. 2009 Abr;100(2):133-6.
8. Bombonato C, Piana S, Moscarella E, Lallas A, Argenziano G, Longo C. Pigmented eccrine
poroma: dermoscopic and confocal features. Dermatol Pract Concept. 2016;6(3):12. DOI:
https://doi.org/10.5826/dpc.0603a12
9. Almeida FC, Cavalcanti SMM, Medeiros ACR, Teixeira MAG. Pigmented eccrine poroma:
report of an atypical case with the use of dermoscopy. An Bras Dermatol. 2013 Out;88(5):803-6.
10. Sano D, Yang J, Cristiano J, Pegas J. Poroma écrino pigmentado simulando melanoma
maligno. Surg Cosmet Dermatol. 2014;6(1):93-5.
1. Federal University of São Paulo (UNIFESP), Hospital São Paulo, São Paulo, SP,
Brazil.
Corresponding author: Bruno de Oliveira Barbosa, Rua Américo Brasiliense, 508, Sala 508, Centro, Ribeirão Preto, SP, Brazil. Zip Code:
14015-050. E-mail: bobstz@gmail.com
Article received: January 16, 2020.
Article accepted: July 15, 2020.
Conflicts of interest: none
COLLABORATIONS
BOB Analysis and/or data interpretation, Conception and design study, Conceptualization,
Data Curation, Final manuscript approval, Formal Analysis, Funding Acquisition, Investigation,
Methodology, Project Administration, Realization of operations and/or trials, Supervision,
Visualization, Writing - Original Draft Preparation, Writing - Review & Editing
ISPB Analysis and/or data interpretation, Data Curation, Final manuscript approval, Investigation,
Project Administration, Realization of operations and/or trials, Supervision, Visualization,
Writing - Original Draft Preparation, Writing - Review & Editing