INTRODUCTION
According to ISAPS (International Society of Aesthetic Plastic Surgery) 1, in 2018, liposuction was the second most performed surgical procedure among plastic
surgeons, totaling 1,732,620 surgeries worldwide, representing a growth of 10 % concerning
the previous survey, and 26% when compared to 2014, denoting the increase in procedures
and visibility of this surgery.
Since the late 1980s, there has been an increase in anatomical interest in the subcutaneous
tissue and its fascias2. In this search, in 1988, Bozola and Psillakis3 described the abdominal shape similar to a lyre. In the same sense, in 1989, Avelar2 observed the existence of areas of convexities and concavities, studies that inspired
the later polishing of the human body contour, promoting results within a more natural
aesthetic pattern.
With the advent of superficial liposuction, performed in the subdermal plane, described
in the late 804 and early 905-7, other possibilities and indications arose that traditional liposuction, deep or
subfascial, did not allow, such as removing fat from more superficial areas aiming
to promote skin retraction, to reduce the indications for abdominoplasty5 drastically.
Combining the concepts, in 1993, Mentz et al.8 were the first to perform superficial liposuction to define the abdominal muscle
lines, coining the term abdominal etching, in eight male patients of athletic size.
In 1997, Ersek and Salisbury9 described superficial abdominal liposuction in 25 male cases.
In 2003, Hoyos et al.10, during the Colombian Congress of Plastic Surgery and later in a 2007 publication10, conceptualized a new type of liposuction: high definition liposculpture, HDL or
HD Lipo, from the English term high definition. The described technique combined the
concepts of superficial liposuction to obtain more robust results, refining the previous
work8, associated with a global, three-dimensional and artistic body approach. For this,
he pointed out differences between male and female patients, in which not only the
abdomen and the back, arms and legs are treated, recommending the use of the third-generation
ultrasonic liposuction device Vaser®, to obtain better results11.
However, nowadays, the tendency to define body contour has evolved to obtain smoother
results. In our practice, we have observed since 201812 that most patients ask for HD Lipo, which is already widespread in society. However,
they aim for results that are not so evident concerning the musculature marking, which
has been more recently called medium or moderate definition liposuction, MD Lipo13 for short. In this line of reasoning, some classification proposals have emerged14-16.
The purpose of this study is to present a liposuction technique that meets the current
desires of patients, which is easy for plastic surgeons to learn, using conventional
liposuction material, accessible from an economic point of view, with satisfactory
aesthetic results and a low incidence of complications.
OBJECTIVES
Describe superficial abdominal liposuction technique, with the definition of the alba
and semilunaris lines and the tendinous intersections of the rectus abdominis muscle,
using conventional liposuction material.
METHODS
The present study is a series of retrospective cases of patients undergoing MD Lipo
in a private hospital in the city of Florianópolis, state of Santa Catarina, Brazil,
from May 2018 to May 2019, with a minimum follow-up of 6 months. The study was submitted
and authorized for publication by the hospital’s medical ethics committee, and followed
the Helsinki declaration rules and all patients signed an informed consent form, including
authorization to publish images for academic purposes.
The inclusion criteria observed were the clinical picture of abdominal lipodystrophy
assessed by the surgeon; body mass index less than 28; stable weight for at least
1 year; without prior abdominoplasty.
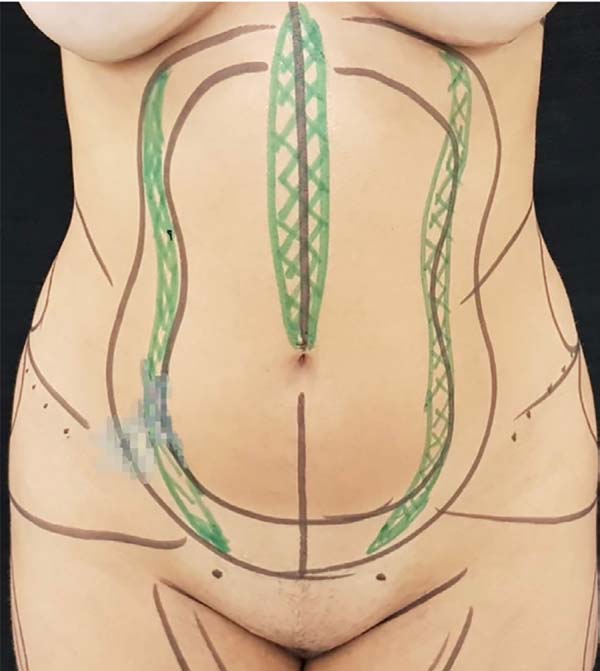
On the day of the surgery, with the patients in an orthostatic position, the alba,
semilunaris lines and the tendinous intersections of the rectus abdominis muscle were
marked (Figures 1 and 2).
Figure 1 - Immediate preoperative marking, female pattern. In black the areas of liposuction,
in green the projections of the semilunar lines and alba line.
Figure 1 - Immediate preoperative marking, female pattern. In black the areas of liposuction,
in green the projections of the semilunar lines and alba line.
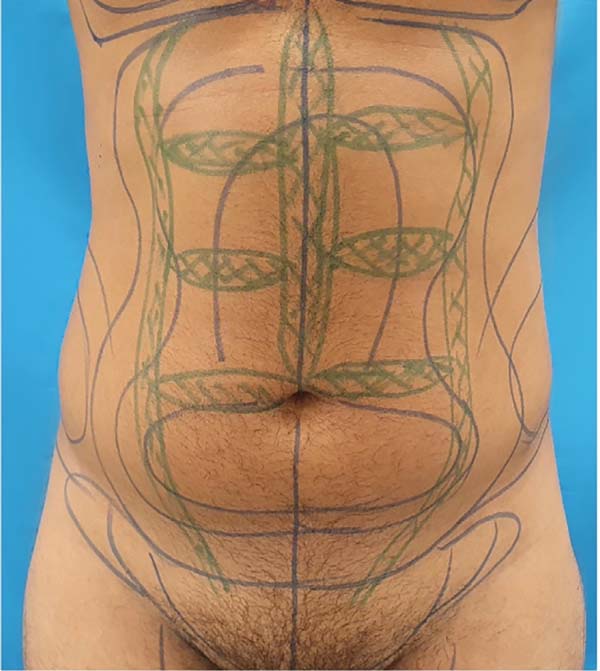
Figure 2 - Immediate preoperative marking, male pattern. In blue the areas of liposuction; in
green the projections of the semilunar lines, alba line, and tendinous intersections
of the rectum muscle. The latter, with slight misalignment to give a non-artificial
appearance, more natural.
Figure 2 - Immediate preoperative marking, male pattern. In blue the areas of liposuction; in
green the projections of the semilunar lines, alba line, and tendinous intersections
of the rectum muscle. The latter, with slight misalignment to give a non-artificial
appearance, more natural.
All patients underwent the procedure under general anesthesia. The incisions were
standardized with two 7mm orifices in the pubic region. Wet infiltration was used,
with infiltrate ratio: 1:2 aspirate, or super wet, with infiltrate ratio: 1:1 aspirate,
with saline solution associated with epinephrine concentration 1:500,000 and lidocaine
at a concentration of 0.05%. The liposuction was obtained with 60ml syringes and latches,
with 4mm diameter cannulas, 5 Mercedes-type orifices, 30 and 35cm in length.
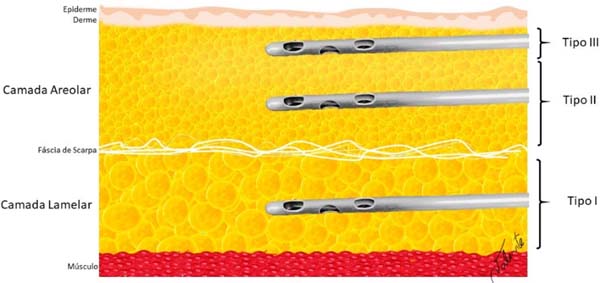
Fat removal was performed using a standardized abdominal liposuction technique, divided
into type I, type II and type III (Figure 3), performed in this order:
Figure 3 - Standardization of liposuction: Lipo type I: removal of fat from the deepest layer
of subcutaneous cellular tissue (SCCT), lamellar layer, below the fascia of Scarpa;
Lipo type II: performed in the areolar layer of the SCCT, above the fascia of Scarpa,
aiming at reducing the volume of this compartment, preserving the most superficial
region of the areolar layer; Lipo type III: it is the liposuction of definition, performed
in the areolar layer even more superficial than the Lipo type II, closer to the deep
dermis, under the alba and semilunar lines.
Figure 3 - Standardization of liposuction: Lipo type I: removal of fat from the deepest layer
of subcutaneous cellular tissue (SCCT), lamellar layer, below the fascia of Scarpa;
Lipo type II: performed in the areolar layer of the SCCT, above the fascia of Scarpa,
aiming at reducing the volume of this compartment, preserving the most superficial
region of the areolar layer; Lipo type III: it is the liposuction of definition, performed
in the areolar layer even more superficial than the Lipo type II, closer to the deep
dermis, under the alba and semilunar lines.
• Lipo type I: removal of fat from the deepest layer of subcutaneous cellular tissue
(SCCT), or lame layer, below the fascia of Scarpa;
• Lipo type II: performed in the areolar layer of the SCCT, above the fascia of Scarpa,
preserving the most superficial region of the areolar layer;
• Lipo type III: it is the definitive liposuction performed in the areolar layer even
more superficial than the Lipo type II, closer to the deep dermis, under the alba
and semilunaris lines (Figure 1). The same surgical material and the same accesses are used, but aiming at the vigorous
removal of fat, with the aid of the contralateral hand to grasp the tissue through
which the cannula slid, alternating with compression and aspiration movements, until
the formation of a visible groove in these places inspected by the surgeon with the
clamping or pinch test maneuver, making sure that the cannula holes are not facing
the dermis. In cases where the patient requested more definition of the tendinous
intersections of the rectus abdominis muscle, 3 incisions were added in the line alba,
of 3mm each, for superficial areolar type III liposuction also with cannulas of 4mm
in diameter, until the formation of a groove in these locations (Figure 2).
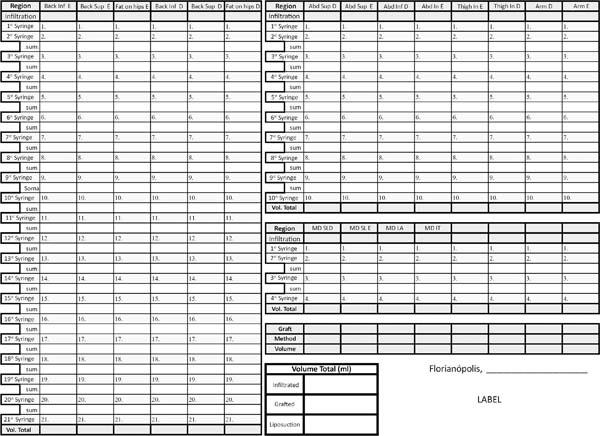
All data referring to the volume withdrawn were recorded by region in milliliters,
possible documentation due to the use of graduated syringes and accounting according
to the document developed by the team (Figure 4).
Figure 4 - Table used in the transoperative period to control the volumes removed (in milliliters)
from the liposuction areas and also from the abdominal definition areas. The use of
liposuction with graduated syringes allows this objective evaluation, helping to water
replacement, more accurate control of the volumes taken from each region, helping
to obtain results closer to the ideal.
Figure 4 - Table used in the transoperative period to control the volumes removed (in milliliters)
from the liposuction areas and also from the abdominal definition areas. The use of
liposuction with graduated syringes allows this objective evaluation, helping to water
replacement, more accurate control of the volumes taken from each region, helping
to obtain results closer to the ideal.
Subsequently, the surgical incisions were closed with continuous polyglecaprone 4.0
(Monocryl®) suture without the use of drains. Then, the dressings were performed as previously
described12, using 7mm diameter hollow malleable silicone tubes (Figure 5), positioned over the sinuous contour of the semilunaris line, as well as rectilinear
positioning of the supraumbilical alba line (Figure 6) and on the tendinous intersections, in the cases in which they were addressed (Figures 7 and 8). Such tubes were fixed vertically with microporous tape, complementing with horizontal
fixations over the entire abdominal extension (Figure 8). Additionally, rectangular foam with cotton lining was used throughout the trunk,
over the silicone tubes, and maintained by the modeling strap.
Figure 5 - Silicone tubes, cylindrical and hollow, to better adapt to the abdominal definition
lines, used for greater skin adhering to aponeurosis.
Figure 5 - Silicone tubes, cylindrical and hollow, to better adapt to the abdominal definition
lines, used for greater skin adhering to aponeurosis.
Figure 6 - On the left, positioning the silicone tube on the semilunar line. On the right, silicone
tubes positioned and fixed with micropore®, female pattern.
Figure 6 - On the left, positioning the silicone tube on the semilunar line. On the right, silicone
tubes positioned and fixed with micropore®, female pattern.
Figure 7 - When defining the tendon intersections, we used the same silicone tubes positioned
on these areas, slightly misaligned to give a more natural aspect.
Figure 7 - When defining the tendon intersections, we used the same silicone tubes positioned
on these areas, slightly misaligned to give a more natural aspect.
Figure 8 - Final aspect of fixed silicone tubes, including tendon intersections. In the end,
microporation was done on the entire abdominal region, performed in all cases
Figure 8 - Final aspect of fixed silicone tubes, including tendon intersections. In the end,
microporation was done on the entire abdominal region, performed in all cases
The patients had their dressings maintained for 5 to 6 days when the silicone tubes
were removed (Figure 9), and the foam was indicated for 15 days and the modeling strap for 30 days.
Figure 9 - Aspect on the first return, with 5 to 6 days. On the left, with tubes and micropore® fixed. In the right, aspect after removal of the dressing, with well-pronounced definition
grooves.
Figure 9 - Aspect on the first return, with 5 to 6 days. On the left, with tubes and micropore® fixed. In the right, aspect after removal of the dressing, with well-pronounced definition
grooves.
The patients had their dressings maintained for 5 to 6 days when the silicone tubes
were removed (Figure 9), and the foam remained indicated for 15 days and the modeling belt for 30 days.
The participants were followed up through consultations before and after the surgery
on the 5th or 6th day, 21st to 28th day, and third and sixth months. The standardized
photographic recording was performed with the Cannon SX30IS model in 4 steps. The
first stage during the preoperative period, the second in the 3rd month and the third
in the 6th month (Figures 10 to 16).
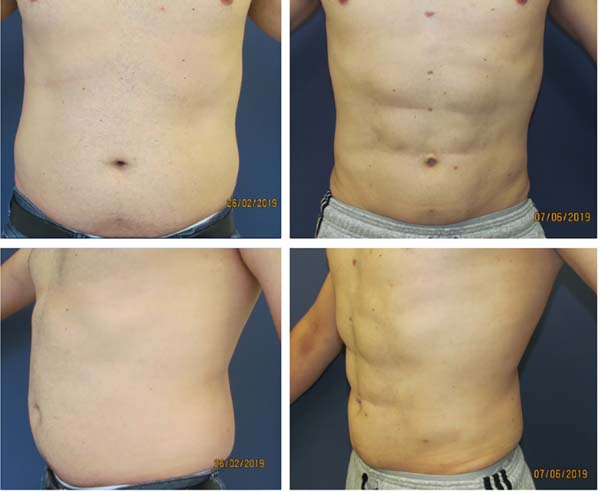
Figure 10 - Male patient, 36 years old, practicing intense physical activity daily. Upper left,
preoperative anterior view. Upper right, postoperative anterior view 6 months. Lower
left, preoperative oblique view. Lower right, postoperative oblique view 6 months.
Figure 10 - Male patient, 36 years old, practicing intense physical activity daily. Upper left,
preoperative anterior view. Upper right, postoperative anterior view 6 months. Lower
left, preoperative oblique view. Lower right, postoperative oblique view 6 months.
Figure 11 - Female patient, 33 years old, practicing moderate physical activity 3 times a week.
Upper left, preoperative anterior view. Upper right, postoperative anterior view 6
months. Lower left, preoperative oblique view. Lower right, postoperative oblique
view 6 months.
Figure 11 - Female patient, 33 years old, practicing moderate physical activity 3 times a week.
Upper left, preoperative anterior view. Upper right, postoperative anterior view 6
months. Lower left, preoperative oblique view. Lower right, postoperative oblique
view 6 months.
Figure 12 - Female patient, 28 years old, sedentary. Upper left, preoperative anterior view. Upper
right, postoperative anterior view 6 months. Lower left, preoperative oblique view.
Lower right, postoperative oblique view 6 months.
Figure 12 - Female patient, 28 years old, sedentary. Upper left, preoperative anterior view. Upper
right, postoperative anterior view 6 months. Lower left, preoperative oblique view.
Lower right, postoperative oblique view 6 months.
Figure 13 - Male patient, 42 years old, sedentary. Upper left, preoperative anterior view. Upper
right, postoperative anterior view 6 months. Lower left, preoperative oblique view.
Lower right, postoperative oblique view 6 months.
Figure 13 - Male patient, 42 years old, sedentary. Upper left, preoperative anterior view. Upper
right, postoperative anterior view 6 months. Lower left, preoperative oblique view.
Lower right, postoperative oblique view 6 months.
Figure 14 - Male patient, 42 years old, practicing moderate physical activities 3 times a week.
Upper left, preoperative anterior view. Upper right, postoperative anterior view 3
months. Lower left, preoperative oblique view. Lower right, postoperative oblique
view 3 months.
Figure 14 - Male patient, 42 years old, practicing moderate physical activities 3 times a week.
Upper left, preoperative anterior view. Upper right, postoperative anterior view 3
months. Lower left, preoperative oblique view. Lower right, postoperative oblique
view 3 months.
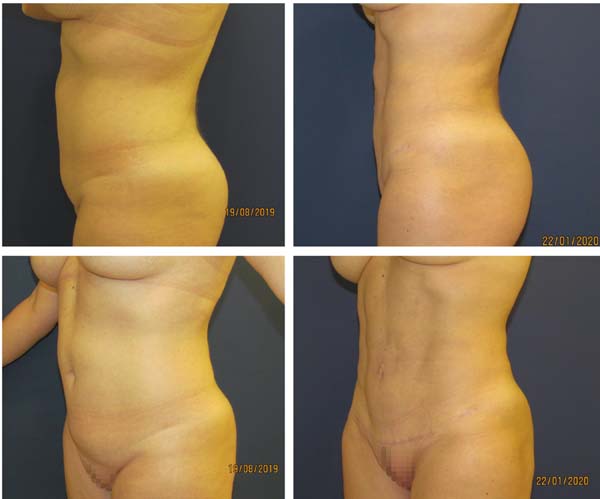
Figure 15 - Female patient, 27 years old, sedentary. Upper left, preoperative oblique view. Upper
right, postoperative oblique view 8 months. Bottom left, preoperative profile view.
Lower right, postoperative profile view 8 months.
Figure 15 - Female patient, 27 years old, sedentary. Upper left, preoperative oblique view. Upper
right, postoperative oblique view 8 months. Bottom left, preoperative profile view.
Lower right, postoperative profile view 8 months.
Figure 16 - Female patient, 44 years old, sedentary. Upper left, preoperative oblique view. Upper
right, postoperative oblique view 6 months. Bottom left, preoperative profile view.
Lower right, postoperative profile view 6 months.
Figure 16 - Female patient, 44 years old, sedentary. Upper left, preoperative oblique view. Upper
right, postoperative oblique view 6 months. Bottom left, preoperative profile view.
Lower right, postoperative profile view 6 months.
The complications investigated through clinical examination were seroma, ischemia,
irregularity, infection, hyperchromia, unaesthetic scarring, late edema and need for
reoperation.
RESULTS
One hundred seven patients were included. All cases were operated on by the same surgeon
from May 2018 to May 2019, with follow-up of at least 6 months. Of these, 22 patients
were excluded due to lack of follow-up after 6 months of surgery, with 85 patients
remaining 10 (8.5%) men and 75 (91.5%) women, between 18-58, with mean, median and
modal age of 37, 35 and 28 years old, respectively.
Of the remaining 85 patients, all underwent MD Lipo with the demarcation of the semilunaris
and alba lines above the umbilical scar. Of these, 10 male patients and 1 female patient
requested the addition of more evident demarcation at the tendinous intersections
of the rectus abdominis muscle through additional incisions. Type III liposuction,
of definition, added an average time of 20 minutes for alba and semilunaris lines
and 30 minutes when also approaching tendinous intersections.
The silicone tubes’ marks were very evident on the first return (Figure 9), being more discreet in the subsequent consultation. There was mild discomfort of
abdominal movement due to the presence of fixed tubes, considered tolerable by the
patients. After 6 months, the results were considered good (Figures 10 to 16) by patients and medical staff by comparing photographs.
There was 1 case of seroma resolved with a puncture on the seventh post-operative
day (5ml) and 2 cases of allergic dermatitis, which started two weeks after the surgery
and ended with topical and systemic use of corticosteroids for one week. There was
a case of unsightly adherence in the left semilunaris line initially treated with
a subcision to release the adherence, but which evolved with seroma, in turn, resolved
after 3 punctures and, later, with lipografting.
Two patients requested reoperation for complementary fat removal with Lipo type II
due to the asymmetry. Both were performed under local anesthesia on an outpatient
regimen, with a male case in a 20ml aspirated right upper abdomen; and a female case
in the left lower abdomen aspirated 30ml.
No color changes, ischemia, unaesthetic scarring, prolonged edema, hematoma or infection
were observed.
DISCUSSION
The contribution of Hoyos et al. (2007, 2014) 10,11 with high-definition liposuction or HD Lipo, opened a new chapter in the history
of liposuction, elevating the artistic concept, shifting to the search for more anatomical
results and more athletic bodies. The concept of high-definition liposuction has recently
been discussed with great interest in the subject and several studies published in
Brazil12,14,17 and the world18-20 and fat graft use within the abdominal rectum sheath21 and classification proposals13-16. As graduating from 0 to 314; in light, only semilunaris lines and alba line, intermediate, associated with “V”
demarcation of the lower abdomen and iliac crest, and high definition added the marking
of the serratile muscle and abdominal metamers15; and low, medium and high definition, based only on photographic examples16.
Evaluating the evolution of aesthetic procedures and the growing search for naturalness,
in our daily practice, we observed since the beginning of 2018 that most patients
request the term HD Lipo, but crave softer reliefs than the requested technique. In
this same sense, it should be remembered that the volumes preserved on the rectus
abdominis muscles between the lines of definition are fatty remnants. Thus, the greater
the difference in the volume of preserved adipose tissue and the regions of aspirated
grooves, causing greater definition, the greater the chances of artificial results
and possible anatomical distortions caused by future variations in body weight. However,
when less adipose tissue is preserved between these grooves, as in MD Lipo, the reliefs
are smoother and physiologically less susceptible to disharmonious changes due to
possible weight fluctuation.
The present MD Lipo technique is guided by the patient’s desire, who mostly seek liposuction
to decrease measures and improve body contour and, secondarily, want abdominal definition.
We understand that liposuction should be done at three levels of depth, from bottom
to top, as described above, as well as we believe that the emptying of the areolar
layer, or Lipo type II, must precede the definition liposuction (Lipo type III), both
for better adapting to the results intended immediately by the patient, as well as
for presenting less chance of future anatomical distortion.
Even though we have been practicing moderately defined liposuction concepts since
2018, the term was first mentioned in an ISAPS Brasil event in April 2019 by Borille13, later published in the same year16. During the event, discussions pointed to the need to separate the intensities of
definition of liposuction, as distinct techniques since MD Lipo aims to promote smoother
and more natural results, as well as to demystify the need to change the liposuction
method used in order to attribute the current aesthetic focus to the surgeon’s technical
ability as the real promoter of the results.
Currently, defining liposuction has been described using a syringe12, liposuction device14,22, vibroliposuction16,18,19 and laser17, as well as third generation ultrasound10,11 and others20. Although many studies have reported the superiority of different technologies for
performing this type of surgery, there is a lack of robust evidence for such statements.
The methodology found in the literature is diverse and incompatible in different aspects
such as inclusion of patients, surgical technique and result evaluation system by
both surgeons and patients, making it impossible to compare them.
Another divergence observed is the need for an additional operative step when there
is the use of high-energy liposuction devices (ultrasound and laser), which require
a greater financial investment and require additional time to prepare the equipment
in the room, in addition to needing to emulsify first the fat and then suck it up.
The present technique took an additional surgical time of 20 to 30 minutes.
As mentioned by Wall Junior et al., in 201823, unlike processes and technologies that use ultrasound, radiofrequency and laser,
traditional liposuction does not apply thermal energy and, therefore, there is no
possibility of burns or related inflammatory response. Studies associated with the
use of Vaser® reported epidermal injury, thermal lesion in the insertion portal and hyperpigmentation18.
About the possible advantages of liposuction performed with high-energy devices, it
is argued that greater skin retraction, reduced recovery period, less ecchymosis and
less post-operative pain. In 201224, a controlled, randomized, blinded clinical trial was published comparing conventional
liposuction with Vaser®, in which it was concluded that there is greater skin retraction and less blood loss
when using the device. It is also reported that there was no difference in the results
between the different methods in relation to pain, edema and final results. However,
such evidence was challenged both by sampling and methodology, financial conflict,
and commercial bias25. In addition, data were published showing the occurrence of seromas, burns in the
access and distance portals, in addition to prolonged edema, unsatisfactory definition,
hyperpigmentation, nodular fibrosis, Mondor syndrome23,26, as well as a high level of technical knowledge of the required device27,28 and high investment in its acquisition. Subsequently, in 2018, Hoyos et al.29, in a series associated with lipoabdominoplasty, made several comments in the need
for better scientific evidence regarding the statements regarding the use of technology.
Pereira-Netto et al., in 201830, in a systematic review, observed that 5 comparative studies between liposuction
associated with laser and traditional liposuction concluded that the association with
technology would be superior in reducing subcutaneous tissue, skin retraction and
patient satisfaction; however, all presented methodological flaws that precede their
conclusions regarding the high level of evidence.
Particularly, we prefer the syringe liposuction technique as it allows an objective
and precise analysis of the volumes removed. Since the measurement in milliliters
of the volumes removed from each region, both in the stage of conventional liposuction
and in the definition liposuction (Figure 4), allows strict control of the volumes aspirated. To increase technical quality and
promote less chance of asymmetries and, therefore, reduce the possibility of new interventions
to improve results. In our experience, the surgical time is equivalent to the other
low-energy methods that we have used previously, such as the liposuction device and
the vibroliposuction device.
We used a dressing with hollow cylindrical silicone tubes (Figure 5), according to previously published observational research12, aiming at better adhesion of the skin to the abdominal aponeurosis and obtaining
more visible grooves on the first return, in order to cause a good initial psychological
impact to the patient. Subsequently, the use of similar tubes was published22; in addition to this material, there are reports of the use of foams (Reston®) 26 and gauze and cotton pads13 to help obtain the definition. However, such materials transmit a straight-line design,
a right angle at the edges (Reston®) and a tendency not to properly preserve the curved anatomy of the semilunaris line,
previously mentioned3. We observed that Reston® has physical characteristics that do not allow adequate adaptation to the curves
of the semilunaris lines and have a right-angled edge, which can negatively interfere
with the liposuction site. We believe that the use of silicone tube dressings requires
a better level of evidence.
Our study observed 3.73% of complications, with dermatitis, adherence, and seroma
occurring with 1.86%, 0.93% and 0.93%, respectively. Two reinterventions were carried
out for complementary withdrawal, as described above. There were no changes in color,
ischemia, unsightly scar, prolonged edema, hematoma or infection. The incidence of
seroma was extremely low even without the use of drains, and there were no cases of
hematoma even with chemical prophylaxis for thrombosis. Contact dermatitis can be
related to the dressing used but was resolved without major commemorations; there
was no pressure injury described by Niddam et al., in 202022, mentioned in a study using similar dressings.
Empirically, we observed greater satisfaction, both for patients and the medical team,
with MD Lipo compared to the traditional technique with no definition previously performed.
Furthermore, as well as Jewell et al. (2002) 27 we believe that just like any form of technology applied to surgery, it is important
to examine whether the new modality is superior to the existing technique in terms
of its efficiency, safety and quality of clinical results, as well as it is important
to compare complications and clinical results found in the literature. From a surgical
perspective, the advances in the devices used must be superior to the existing technology
and provide overwhelming evidence for this before affirming superiority.
Finally, we believe that the definition result, be it HD Lipo or MD Lipo, is dependent
on the plastic surgeon: his aesthetic sensitivity, anatomical knowledge and experience,
regardless of the device of his choice.
CONCLUSION
A medium-definition abdominal liposuction technique or MD Lipo has been described,
using conventional liposuction instruments in the alba and semilunaris lines and the
tendinous intersections of the rectus abdominis muscle.
REFERENCES
1. International Society of Aesthetic Plastic Surgery (ISAPS). International survey on
aesthetic/cosmetic procedures performed in 2018 [Internet]. West Lebanon: ISAPS; 2018;
[acesso em 2020 Ago 08]. Disponível em: https://www.isaps.org/wp-content/uploads/2019/12/ISAPS-Global-Survey-Results-2018-new.pdf
2. Avelar J. Regional distribution and behavior of the subcutaneous tissue concerning
selection and indication for liposuction. Aesthetic Plast Surg. 1989;3(13):155-65.
3. Bozola AR, Psilakis J. Abdominoplasty: a new concept and classification for treatment.
Plast Reconstr Surg. 1988 Dez;82(6):983-93.
4. Gasperoni C, Salgarello M, Emiliozzi P, Gargani G. Subdermal liposuction. Aesthetic
Plast Surg. 1990;14(2):137-42.
5. Gasperoni C, Salgarello M. Rationale of subdermal superficial liposuction related
to the anatomy of subcutaneous fat and the superficial fascial system. Aesthetic Plast
Surg. 1995 Jan/Fev;19(1):13-20.
6. Gasparotti M, Lewis CM, Toledo LS. Superficial liposculpture: manual of technique.
New York: Springuer-Verlag; 1993.
7. Souza EBS, Abdalla PCSP, Moia SMS, Cação EG, Federico R, Chávez RS. Lipomioescultura.
In: Souza EBS, org. Lipomioescultura. Rio de Janeiro: Di Livros Editora Ltda.; 2009.
p. 139-71.
8. Mentz HA, Gilliland MD, Patronella CK. Abdominal etching: differential liposuction
to detail abdominal musculature. Aesthetic Plast Surg. 1993;17(4):287-90.
9. Ersek RA, Salisbury AV. Abdominal etching. Aesthetic Plast Surg. 1997 Set/Out;21(5):328-31.
10. Hoyos AE, Millard JA. VASER-assisted high-definition liposculpture. Aesthet Surg J.
2007 Nov/Dez;27(6):594-604.
11. Hoyos A, Prendergast PM. High definition body sculpting: art and advanced lipoplasty
techniques. Berlin: Springer-Verlag; 2014.
12. Gomes RS, Mattiello CM, Rendon NB, Garcia EB, Gomes HFC, Ferreira LM. Lipoaspiração
abdominal de alta definição e tubos de silicone. Rev Bras Cir Plást. 2018 Out;33(4):567-71.
13. Borille G. Medium definition liposuction. Med Clin Res. 2019;4(12):1-3.
14. Viaro MSS. Lipoaspiração de definição abdominal. Rev Bras Cir Plást. 2019;34(3):336-43.
15. Cucchiaro JV. High definition liposuction classification. Plast Reconstr Surg Glob
Open. 2019 Set;7(9):e2440.
16. Saad A, Combina LN, Altamirano-Arcos C. Abdominal etching. Clin Plast Surg. 2020 Juk;47(3):397-408.
17. Motta RP. Lipoaspiração laser-assistida de alta definição. Rev Bras Cir Plást. 2018;33(1):48-55.
18. Husain TM, Salgado CJ, Mundra LS, Perez C, AlQattan HT, Bustillo E, et al. Abdominal
etching: surgical technique and outcomes. Plast Reconstr Surg. 2019 Abr;143(4):1051-60.
19. Saad AN, Arbelaez JP, Benito J. High definition liposculpture in male patients using
reciprocating power-assisted liposuction technology: techniques and results in a prospective
study. Aesthet Surg J. 2020 Fev;40(3):299-307.
20. Cucchiaro JV. Abdominal etching: surgical technique and outcomes. Plast Reconstr Surg.
2020 Abr;145(4):1051-60.
21. Danilla S. Rectus abdomin fat transfer (RAFT) in lipoabdominoplasty: a new thechinique
to achive fitness body contour in patients tha require tummy tuck. Aesthet Surg J.
2017 Jun;41(6):1389-99.
22. Niddam J, Hersant B, Aboud C, Sawan D, SidAhmed-Mezi M, Meningaud JP. Postoperative
complications and patient satisfaction after abdominal etching: prospective case series
of 25 patients. Aesthetic Plast Surg. 2020;44(3):830-5. DOI: https://doi.org/10.1007/s00266-019-01558-4
23. Wall Junior SH, Claiborne JR. Discussion: a report of 736 high-definition lipoabdominoplasties
performed in conjunction with circumferential VASER liposuction. Plast Reconstr Surg.
2018 Set;142(3):676-8.
24. Nagy MW, Vanek Junior PF. A multicenter, prospective, randomized, single-blind, controlled
clinical trial comparing vaser-assisted lipoplasty and suction-assisted lipoplasty.
Plast Reconstr Surg. 2012 Abr;129(4):681e-9e.
25. Swanson E. Improved sking contraction after VASER-assited lipoplasty: is it a change
we can belive in? Plast Reconstr Surg. 2012 Nov;130(5):754e-6e.
26. Danilla S, Babaitis RA, Jara RP, Quispe DA, Andrades PR, Erazo CA, et al. High- definition
liposculpture: what are the complications and how to manage them?. Aesthetic Plast
Surg. 2020 Abr;44(2):411-8.
27. Jewell ML, Fodor PB, Pinto EBS, Al Shammari MA. Clinical application of VASER-assisted
lipoplasty: a pilot clinical study. Aesthet Surg J. 2002 Mar;22(2):131-46.
28. Pinto EBS, Abdala PCSP, Maciel CM, Santos FPT, Souza RPM. Liposuction and VASER. Clin
Plast Surg. 2006 Jan;33(1):107-15.
29. Hoyos A, Perez ME, Guarin DE, Montenegro A. A report of 736 high-definition lipoabdominoplasties
performed in conjunction with circumferential VASER liposuction. Plast Reconstr Surg.
2018 Ago;142(3):662-75.
30. Pereira-Netto D, Montano-Pedroso JC, Aidar ALS, Marson WL, Ferreira LM. Laser-assisted
liposuction (LAL) versus traditional liposuction: systematic review. Aesthetic Plast
Surg. 2018 Abr;42(2):376-83.
1. Hospital Carlos Corrêa, Plastic Surgery Service, Florianópolis, SC, Brazil.
Corresponding author: Rogerio Schützler Gomes, Avenida Trompowsky, 291, Torre 1, Sala 303, Centro, Florianópolis, SC, Brazil. Zip
Code: 88015-300 E-mail: plasticarogerio@gmail.com
Article received: August 20, 2020.
Article accepted: January 10, 2021.
Conflicts of interest: none
COLLABORATIONS
RSG Analysis and/or data interpretation, Conception and design study, Conceptualization,
Data Curation, Final manuscript approval, Investigation, Methodology, Project Administration,
Realization of operations and/or trials, Supervision, Validation, Visualization, Writing
- Original Draft Preparation, Writing - Review & Editing
GVN Analysis and/or data interpretation, Conception and design study, Final manuscript
approval, Methodology, Project Administration, Validation, Writing - Review & Editing