

Case Report - Year 2021 - Volume 36 - Issue 1
Pulmonary thromboembolism due to superficial venous thrombophlebitis in upper limbs after cosmetic breast plastic surgery: report of 3 cases
Tromboembolismo pulmonar decorrente de tromboflebites venosas superficiais em membros superiores pós-cirurgia plástica mamária estética: relato de 3 casos
ABSTRACT
Superficial thrombosis and thrombophlebitis of the upper limbs are frequent and often underestimated diseases. We report three patients in the postoperative cosmetic breast plastic surgery period who presented thrombophlebitis in the upper limbs and who evolved with pulmonary thromboembolism. All patients had a typical clinical picture, with Doppler ultrasound evidence of thrombosis/superficial phlebitis of the upper limbs and absence of lesions in the lower limbs and an increase in D-dimer and evidence of pulmonary embolism by computed tomography or pulmonary scintigraphy. The three cases evolved with improvement after anticoagulation and without sequelae.
Keywords: Thrombophlebitis; Thrombosis; Pulmonary embolism; Augmentation mammoplasty; Postoperative complications; Thromboembolism; Venous thromboembolism
RESUMO
Tromboses e tromboflebites superficiais de membros superiores são doenças frequentes e muitas vezes pouco valorizadas. Relatamos três pacientes no pós-operatório de cirurgias plásticas mamárias estéticas que apresentaram tromboflebite em membros superiores e que evoluíram com tromboembolismo pulmonar. Todas as pacientes apresentaram quadro clínico típico, com comprovação pelo Doppler ultrassonografia de trombose/flebite superficial de membros superiores e ausência de lesões em membros inferiores, bem como aumento de dímero-D e comprovação da embolia pulmonar por tomografia computadorizada ou cintilografia pulmonar. Os três casos evoluíram com melhora após anticoagulação e sem sequelas.
Palavras-chave: Tromboflebite; Trombose; Embolia pulmonar; Mamoplastia de aumento; Complicações pós-operatórias; Tromboembolia; Tromboembolia venosa
INTRODUCTION
Thromboembolic phenomena can result from thrombosis and/or superficial venous thrombophlebitis (SVT) of the upper limbs1. Most superficial thromboses also compete with phlebitis, in contrast to deep vein thrombosis (DVT), where phlebitis may be absent2. Pulmonary thromboembolism (PTE) can rarely be related to lower limb SVT (lower limbs)1. There are few upper limb SVT reports (upper limbs) leading to PTE3-7, and there are no reported cases related to cosmetic surgery.
In this article, we report 3 cases of patients who underwent cosmetic breast plastic surgery who had confirmed upper limb SVT and evolved with PTE.
CASE REPORT
Check Chart 1.
| Type | Case 1 | Case 2 | Case 3 | |
|---|---|---|---|---|
| Surgery performed | Retromuscular augmentation mastopexy (dual plane) and abdominoplasty | Retro augmentation mammoplasty Muscular (dual plane) |
Retro Muscular Augmentation Mammoplasty (dual plane) | |
| Date surgery | 19/12/2013 | 16/02/2016 | Day 09/8/2017 | |
| Site of surgery | Hospital Metropolitano de Sarndi (PR) - Private | Hospital do Câncer - Maringá (PR) - Private | Hospital do Câncer - Maringá (PR) - Private | |
| Duration of surgery | Five hours and 30 minutes. | 1h20 min | 1 hour | |
| Type and Duration of anesthesia | Epidural and General 6h30min h | General 1 h 50 min. | General 1 h 30 min. | |
| Use of BCP | Suspended for 1 month pre-Operative and after surgery | Suspended only after Surgery | Didn't use | |
| Chemo prophylaxis | Made heparin intraoperatively and maintained for 4 days postoperatively | not performed | not performed | |
| Venous puncture site | RIGHT upper member | RIGHT upper member | LEFT upper limb | |
| Ultrasound of upper limbs | thrombophlebitis of basilica and brachial veins BILATERALLY | left basilica thrombophlebitis at elbow level | presence of imaging suggestive of occlusive thrombotic residues in the median vein of the right elbow | |
| Ultrasound of lower limbs | absence of thrombi in deep and superficial vessels | absence of lesions in superficial and deep veins | absence of lesions in superficial and deep veins | |
| D-dmin *ref. positive = or > 500 ng/ml) *FEU equivalent fibrinogenic units) |
2110.00 ng/ml | 810.0 ng/ml | 4110 ng/ml | |
| Pulmonary tomography | Signs of pulmonary thromboembolism in the distal third of the left pulmonary artery. Possible small clots embolizing the posterior segment of the lower lobe to the right | Discrete bilateral basal opacities, which may correspond to the opacity of decubitus | SIGNS of PTE in the right lower lobe posterior segment | |
| Pulmonary scintigraphy | Not performed | Presence of focal areas, with decreased blood perfusion, of a subsegmental pattern dispersed in the posterior segment of the right upper lobe, superior of the right lower lobe, lateral of the middle lobe and lateral of the left lower lobe, of a subsegmentary pattern, disagreeing with the inhalation pattern. High probability of pulmonary thromboembolism. | Not performed | |
| 2. Presence of focal areas of radiotracer hypocaptation located in the most basal portions of the right lung, suggesting a parenchymal process (atelectasis?) | ||||
| Investigation for thrombophilia | Negative | POSITIVE, diagnosed with antiphospholipid antibody syndrome (point mutation C677T: Heterozygous mutated), IgM Cardiolipin antibodies 64.0 MPL-U and after 6 months 57.0 MPL-U (Positive higher than 40) | Negative | |
| Other exams | Normal echocardiogram | |||
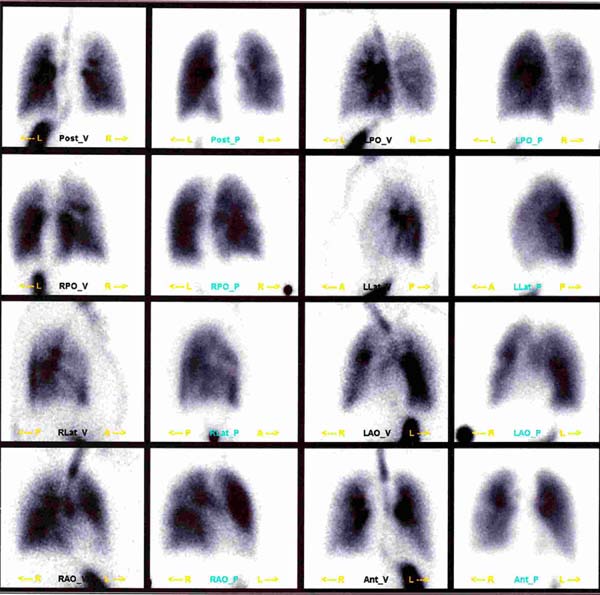
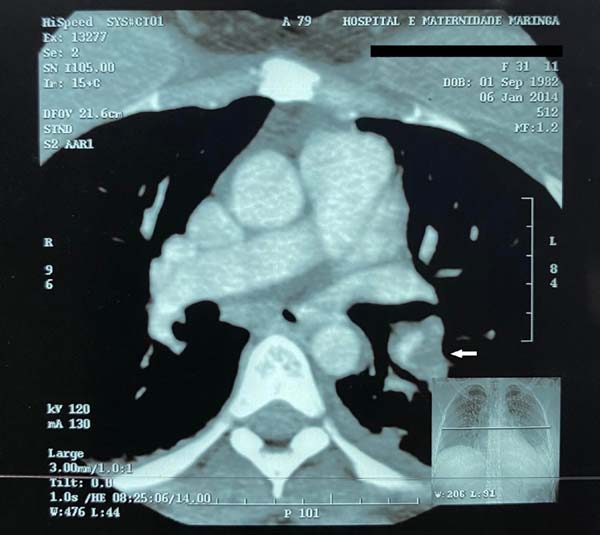
Case 1. A 31-year-old female patient without comorbidities who underwent a mastopexy of retromuscular augmentation and abdominoplasty without liposuction. She wore elastic stockings during the procedure and for one more week, an anti-thrombosis device for 24 hours, subcutaneous heparinization in the intra and postoperative periods for four days (heparin from 10 to 15 thousand U/day), and contraception suspended for 30 days before surgery. After 15 days, she had pain in her upper limbs, and on the 18th day, she had sudden dyspnea diagnosed with PTE (Figures 1 and 2). She was hospitalized for 7 days, 5 of them in an intensive care unit, oxygen supplementation (without orotracheal intubation), observation, and anticoagulation. It evolved without sequelae.
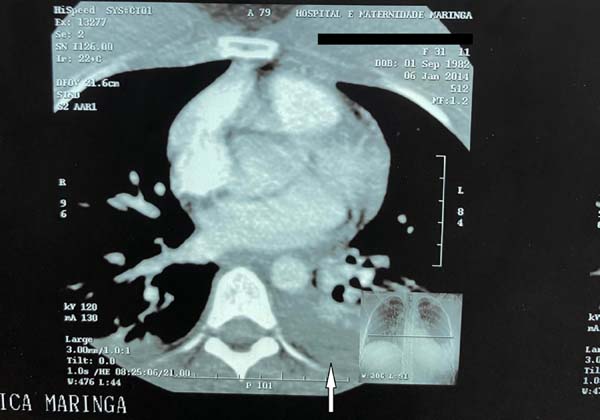
Case 2. A 35-year-old female patient with no comorbidities who underwent breast augmentation. She developed a sudden dyspneic condition with no complaints until the 10th postoperative day, confirming PTE (Figure 3). She was admitted for three days for observation, oxygen supplementation (without orotracheal intubation), and anticoagulation. It evolved without sequelae. Contraceptive suspension (BCP) only after surgery.
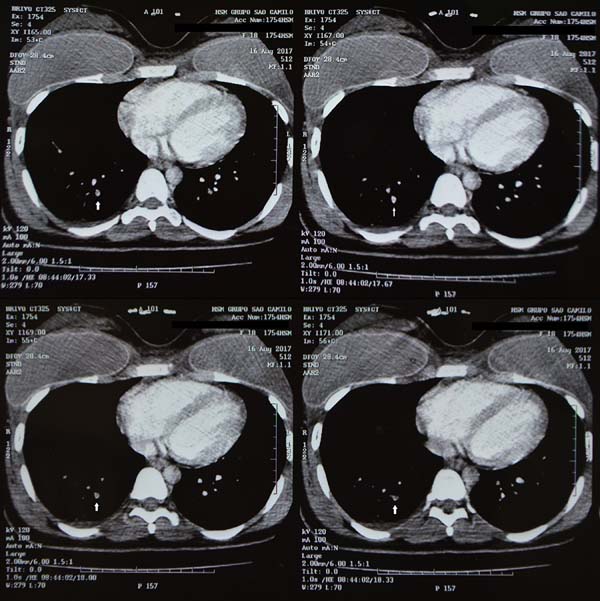
Case 3. A 17-year-old female patient without comorbidities who underwent a breast augmentation. There were no complaints until the 6th postoperative day, when she developed sudden dyspnea, confirming PTE (Figure 4). She was hospitalized for five days, two in an intensive care unit, for observation, oxygen supplementation (without orotracheal intubation), and anticoagulation. It evolved without sequelae. Family history of postoperative embolism in grandfather and uncle.
DISCUSSION
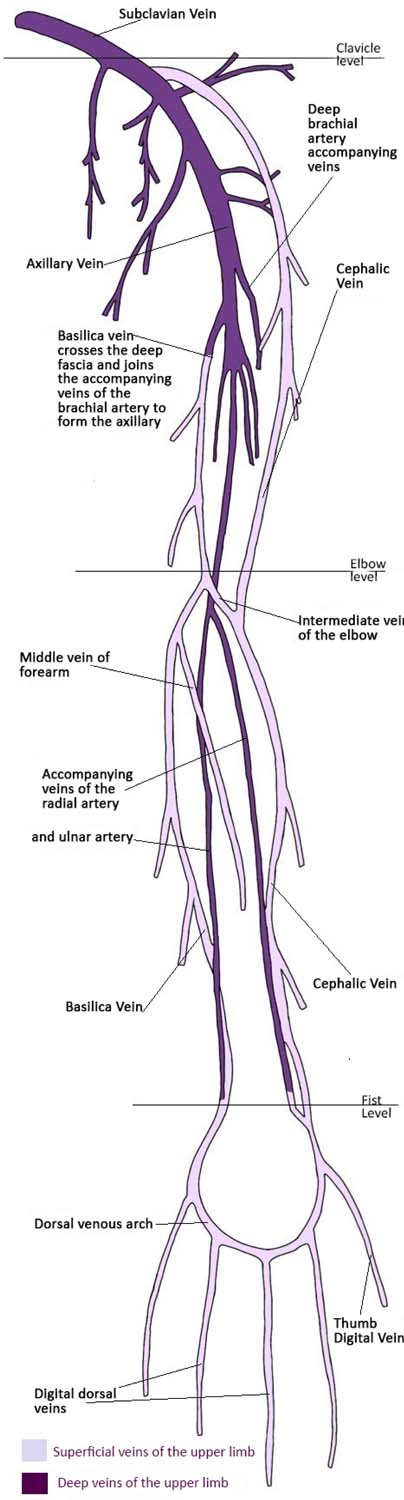
PTE is especially feared after cosmetic surgery. In the cases described, it is surprising that the embolic source is from upper limbs (Figure 5).
SVT is a common disease, usually identifying a palpable cord (best sign with positive predictive value), hyperemic, painful, and hot in the course of the superficial vein1. In more severe cases of the upper limb, it can extend to axillary veins. In case 1, thrombosis reached brachial veins.
PTE secondary to SVT of the upper limbs is rare in the absence of DVT4. SVT is probably little detected and is at least 2 to 3 times more frequent than deep. It usually resolves spontaneously. In lower limbs, SVT evolves in 20 to 33% for asymptomatic PTE and 2 to 13% for symptomatic. There is no data for upper limbs.
In cases 1 and 3, computed tomography (CT) was compatible, and in case 2, pulmonary scintigraphy confirmed the diagnosis of PTE (inconclusive CT). Doppler ultrasonography of the upper limb was associated with the absence of thrombi in the lower limbs. Therefore, PTEs resulting from SVT of the upper limb (compatible clinic, positive D-dimer, and CT or pulmonary scintigraphy proving PTE) were confirmed8. Besides, patients improved after anticoagulation.
As a cause of upper limbs thromboembolic phenomena, the use of central venous catheters (chemotherapy, prolonged antibiotic therapy, or parenteral nutrition) is found, as well as peripheral venous catheters (often “trivialized” in conventional medicine)9. In cases 2 and 3, it is noteworthy that the SVT was contralateral to the punctured limb, and in case 1, bilateral.
Several studies suggest a predictive score for safety parameters in plastic surgery10,11. However, only in case 1 did the surgery last for more than 4 hours, and in the others, it was close to 1 hour. Despite preventive measures for thromboembolism, patient 1 presented bilateral upper limbs SVT that extended to deep, probably due to prolonged immobilization and delay in diagnosis.
The research for preoperative thrombophilia is questionable (rarity of these situations and high cost). It should only be performed in the case of unexplained thromboembolic phenomena9,12.
Hereditary thrombophilia (Chart 2) and oral contraceptives have a higher risk of thromboembolism, about 2 to 20 times12. Case 2 presented acquired thrombophilia (without a previous diagnosis) and use of oral contraception.
| Classification of thrombophilias13 |
|---|
| Hereditary |
| Antithrombin deficiency protein deficiency
C Protein Deficiency Protein S Protein Deficiency Z resistance APC (APCR) Factor V Leiden mutation (R506Q) Prothrombin G20210A gene Mutation MTHFR mutation (variants 677C>T and 1298A>C) PAI-1 675G>A mutation (4G/5G) and 844A>G Dysfibrinogenemias High Factor IX High Factor XI |
| Acquired |
| Antiphospholipid antibody syndrome (APLS) |
| Mixed/combined |
| Hyperhomocysteinemia high factor VIII activity increased fibrinogen |
| Other thrombophilias |
| ACE Ins/del fibrinogen (455G>A) factor XIII (Val34Leu) APOE (Cys112Arg and Arg158Cys) EPCR (4678G/C) |
There is a case description of PTE in the literature due to SVT in a patient using hormone therapy only4. Hormone therapy or oral contraception increases the chance of thromboembolism by up to four times. Thus, the importance of hormonal suspension, even in cases of lower risk10.
The most important chemoprophylaxis in venous thrombosis would be with fibrinolytic agents (heparin or low molecular weight heparin), while in arterial, it is based on the use of antiplatelet agents10.
Mechanical prophylaxis (elastic stockings, intermittent pneumatic devices) reduces venous stasis and distension. The pneumatic device has little fibrinolytic activity10. It is recommended to start it 30 minutes before anesthetic induction until the patient’s discharge, in surgeries longer than one hour10.
There are no reports of post-plastic surgery PTE from upper limb SVT. Several factors could explain this fact, such as:
the inadequate position of the upper limbs during the intraoperative
period;
postoperative immobilization, especially in cases of retromuscular
breast implant (postoperative usually more painful);
exaggerated immobilization of the limbs and/or inappropriate flexing
of the limbs, for example, due to the excessive time of electronic
devices (cell phones or computers), leading to an inadequate posture
for drainage and consequent local stasis. In these cases, an elastic
band (for non-displacement) above the prostheses was used.
CONCLUSION
Cosmetic breast augmentation surgery with implants, although usually not long, can also lead to non-local complications. Superficial thrombophlebitis, triggered by excessive rest and/or venipuncture, is often overlooked and can progress to thrombosis of larger vessels or even PTE.
Preoperatively, it is suggested to follow the prophylaxis protocols for thromboembolism. In the intraoperative period, it is recommended that the arms’ position be constantly monitored and the use of elastic stockings, pneumatic apparatus in the lower limbs, and chemoprophylaxis. Postoperative surveillance of the upper limbs is also suggested to avoid excessive edema, and active research for thrombophlebitis.
REFERENCES
1. Sobreira ML. Complicações e tratamento da tromboflebite. J Vasc Bras. 2015 Jan/Mar;14(1):1-3.
2. Nagarsheth KH. Superficial thrombophebitis: overview. Medscape. 2019.
3. Cascella M, Viscardi D, Bifulco F, Cuomo A. Postoperative massive pulmonary embolism due to superficial vein thrombosis of the upper limb. J Clin Med Res. 2016 Abr;8(4):338-41.
4. Manzana BJ, Tan RG, Tuason JP, Onf N. A case of pulmonary embolism from superficial venous thrombosis with an upper extremity source in a 35-years-old female on orla contraceptive pills. Respirology. 2018;23(Supl 2):90-334.
5. Sassu GP, Chisholm CD, Howell JM, Huang E. A rare etiology for pulmonary embolism: basilic vein thrombosis. J Emerg Med. 1990 Dez;8(1):45-9.
6. Barros FS, Sandri JL, Prezotti BB, Nofa DP, Cunha SXS, Barros SD. Pulmonary embolism in a rare association to a floating thrombus detected by ultrasound in the basilic vein at the distal arm. Rev Bras Ecocardiogr Imagem Cardiovasc. 2011;24(4):89-92.
7. Clement DL. Superficial vein thrombosis: more dangerous than anticipated. Phlebolymphology. 2013;20(4):188.
8. Rivera-Lebron B, McDaniel M, Ahrar K, Alrifai A, Dudzinski DM, Fanola C, et al. Diagnosis, treatment and follow up of acute pulmonary embolism: consensus practice from the PERT Consortium. Clin Appl Thromb Hemost. 2019 Jan;25:1076029619853037.
9. Drouin L, Pistorius MA, Lafforgue A, N’Gohou C, Richard A, Connault J, et al. Épidémiologie des thromboses veineuses des membres supérieurs: étude rétrospective de 160 thromboses aiguës. Rev Med Interne. 2019 Jan;40(1):9-15.
10. Iorio ML, Venturi ML, Davison SP. Practical guidelines for venous thromboembolism chemoprophylaxis in elective plastic surgery. Plast Reconstr Surg. 2015 Fev;135(2):413-23.
11. Saldanha OR, Salles AG, Llaverias F, Saldanha Filho OR, Saldanha BC. Fatores preditivos de complicações em procedimentos da cirurgia plástica - sugestão de escore de segurança. Rev Bras Cir Plást. 2014 Jan/Mar;29(1):105-13.
12. Lima J, Borges A. Rastreio de trombofilias. Bol SPHM. 2012 Dez;27(4):5-11.
1. Clínica Dra. Márcia Balbina L. Hoyos,
Plastic Surgery, Maringá, PR, Brazil.
MBLH Aprovação final do manuscrito, Coleta de Dados, Conceitualização, Concepção e desenho do estudo, Gerenciamento do Projeto, Investigação, Metodologia, Realização das operações e/ou experimentos, Redação - Preparação do original, Redação - Revisão e Edição, Software, Supervisão, Validação, Visualização
Corresponding author: Márcia Balbina Lorenzo Hoyos, Avenida Doutor Luiz Teixeira Mendes, 2418, Zona 05, Maringá, PR, Brazil. Zip Code: 87015-001. E-mail: mblhoyos@gmail.com
Article received: November 20, 2019.
Article accepted: July 15, 2020.
Conflicts of interest: none










 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter