ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Cleft Patients Treatment Profile in Brazil
Perfil do Tratamento de Fissurados no Brasil
Articles -
Year2000 -
Volume15 -
Issue
3
Diogo FrancoI, Luiz Fernando GonçalvesI, Talita FrancoII
ABSTRACT
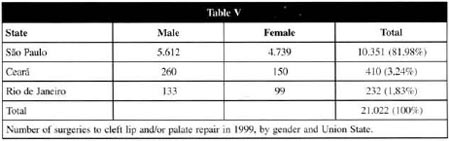
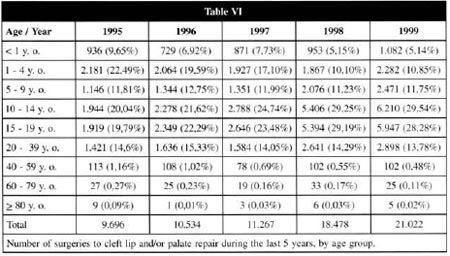
The purpose of this paper is to highlight the importance of multidisciplinary assistance to treat patients with cleft lip and/or palate, to evaluate the treatment protocols used by the main centers in Brazil, and to compare them to the ones used by the main centers in other countries. The medical literature regarding congenital malformation was reviewed. A treatment protocol questionnaire was elaborated and sent to all plastic surgery centers in Brazil that are recognized by the Brazilian Plastic Surgery Society and to other centers known as active in the treatment of cleft lip and/or palate. The data about cleft lip and/or palate surgeries peiformed in the last 5 years were obtained from the Brazilian Health Ministry files. Different treatment protocols have been used in the various centers. There is a consensus about the most applied surgical techniques, the best age group to perform the sugeries)and the necessity of a multidisciplinary team. The number of surgeries increased from 9,696 in 1995 to 21,022 in 1999. Eighty-three percent of the surgeries performcd in 1999 were made in the State of São Paulo. There is no consensus about treatment protocols for cleft patients in Brazil. However, the best results came from centers that adopt a treatment protocol, have well-trained surgeons and perform long-term follow-up.
Keywords:
Cleft lip; rehabilitation; cleft palate ; rehabilitation; patient assistance team
RESUMO
Este trabalho foi elaborado com o propósito de ressaltar a importância do atendimento multidisciplinar ao portador de fenda labiopalatal e avaliar os protocolos empregados no Brasil e em grandes centros de outros países.
Realizou-se a revisão da literatura médica referente ao tratamento desta malformação congênita. Elaborou-se um questionário, relativo aos protocolos de atendimento, que foi enviado a todos os Serviços de Cirurgia Plástica do Brasil vinculados à Sociedade Brasileira de Cirurgia Plástica e também a outras Unidades indicadas como atuantes no tratamento deste tipo de paciente. Analisaram-se os dados oficiais de cirurgias por fendas labiais e/ou palatais realizadas nos últimos 5 anos, fornecidos pelo Ministério da Saúde do Brasil.
Identificou-se grande variedade nos protocolos de atendimento. Houve controvérsias em diversas áreas, contudo, observou-se consenso nas técnicas cirúrgicas mais utilizadas, na faixa etária indicada para as cirurgias, além de unanimidade na indicação de acompanhamento multidisciplinar. O número de cirurgias realizadas subiu de 9.696 no ano de 1995 para 21.022 no ano de 1999, sendo o Estado de São Paulo responsável por 83,9% dos procedimentos realizados no último ano.
Ainda não há total consenso com relação aos protocolos de atendimento ao portador de fenda labiopalatal no Brasil. Entretanto, observa-se que os melhores resultados são obtidos em instituições que trabalham com protocolos definidos, cirurgiões experientes e acompanhamento a longo prazo.
Palavras-chave:
Lábio fissurado; reabilitação; fissura palatina; reabilitação; equipe de assistência ao paciente
INTRODUCTION
The purpose of this study is to highlight me importance of a health multidisciplinary team to treat congenital cleft malformation. The treatment protocols used in Brazil were evaluated and compared to those proposed in me medical literature. Government data regarding hospital admissions for cleft lip and/or palate surgeries were also presented and discussed.
MATERIAL AND METHODS
LITERATURE REVIEW
The literature review allowed us to evaluate me treatment protocols for cleft patients used in different parts of me world and to compare them to me Brazilian centers' resources and results.
NATIONAL RESEARCH
A cleft lip and/or palate treatment protocol questionnaire was elaborated and sent to all centers recognized by me Brazilian Plastic Surgery Society. It was also sent to fifteen non-recognized centers, but active in assisting cleft patients. The purpose of these questionnaires was to evaluate me assistance pravided by me centers, me prafessionals that compose me teams, me preferred surgical technigues, and me treatment plan for cleft patients in Brazil.
HEALTH MINISTRY DATA
The data were obtained from me Health Ministry hospital admission and surgery files and analyzed according to diseases and States between 1995 and 1999.
RESULTS
NATIONAL RESEARCH
Among the 73 contacted centers, 45 (61.6%) returned the form.
The main conclusions about me plastic surgery centers in Brazil are:
1. 89% assist patients with cleft lips and/or palate.
2. In 75% at least three other specialties assist cleft patients, including dentistry and speech therapist.
3. In 80% the plastic surgery team coordinate me treatment.
4. 62.5% make less than 5 primary surgeries per month.
5. 25% make more than 10 primary surgeries per month.
6. Most of me surgeries in Brazil are performed in me age groups recommended by the main reference centers in me world.
7. Surgical techniques are uniform among me centers, except for cleft lip bilateral correction.
HEALTH MINISTRY DATA
The statistic data in Brazil regarding me incidence of cleft lip and/or palate are not precise. The incidence of cleft lip associated or not with cleft palate in me Caucasian population is 1 out of 1.000 born alive (between 0.7 and 1.3). Considering the data from the last 2 years, there are approximately 3,100,000 liveborn infants per year in Brazil. It means approximately 3,100 new cleft lip cases per year.
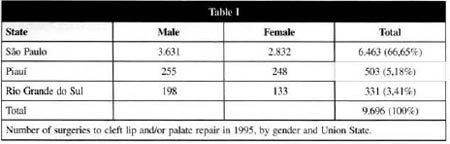
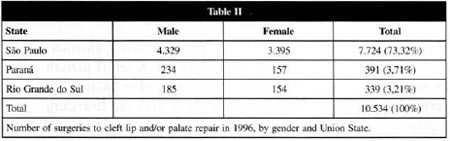
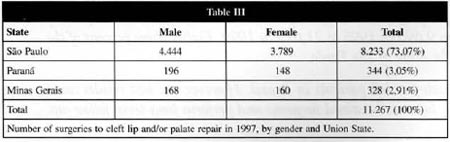
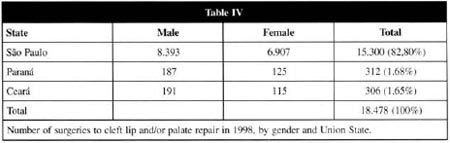
The Health Ministry data from the last 5 years provided the number of surgeries made for cleft lip and or palate, the patient gender, the age group, and the State where the procedures were performed (Tables I to VI).
DISCUSSION
The multidisciplinary assistance to cleft patients intends to provide easy access to the specialties involved in the treatment. It also provides information to the patient's relatives, thus, they can participate in the treatment. The main specialties are: plastic surgery, dentistry, and speech therapy. Other important specialties involved in the treatment of cleft patients are: pediatrics, maxilofacial surgery, psychology, genetics, otorhinolaryngology, social center, and nursing. The participation of any other specialties might also be necessary. The patient should always be assisted by the same professionals, in order to make the treatment consistent. Even when a highlyintegrated team performs the treatment, it may need complementation (1,2,3).
The most used surgical technigue nowadays for unilateral cleft lip correction was proposed by Millard, in 1955. There have been variations in this technigue so as to overcome difficulties, but the basic technigue still is to make two flaps, advance one, and rotate the other one.
Millard technigue is also the choice for bilateral cleft lip correction. It can be made in one ar two surgeries. However, among the plastic surgery centers in Brasil, the most used technigue was described by Spina (1963).
There is no consensus about the best age group and technigue to perform the palatoplasty. It is believed that the sooner the surgery is performed the better the speech is, but early surgeries compromise facial development. On the other hand, the longer the surgery is delayed the lesser facial development abnormalities occur, but late surgeries compromise the speech(5,6,7,8).
Part of the treatment protocols in the reference centers is to evaluate the need for complementary procedures to correct velopharyngeal insufficiency. The most used surgical technigues to correct velopharyngeal insufficiency are: secondary palatoplasty, with maximum muscular retroposition; pharyngoplasty, to enlarge the pharynx posterior wall; and pharyngeal flaps to unite the pharynx posterior wall to the soft palate. There is no consensus about the best technigue. In Brazil, Lessa (1996) recommends pharyngoplasty associated or not with secondary palatoplasty, Zanini (1997) makes secondary palatoplasty using Furlow technigue in cases of velopharyngeal occlusion failure of up to 1.5 cm, and Collares (1999) prefers surgical revision by the Veau or Wardill-Kilner technigue associated with intravelar veloplasty.
Treatment protocols for orthodontics and maxillary growth are very conflicting. The exact mechanism that affects maxillary growth on the cleft side has not been identified yet(12,13,14,15). Differences between the two sides can be visualized during the examination or by tests. Several factors have already been considered responsible for this difference: palatal detachment(16); lip surgery without palatoplasty(17); lip surgery associated with palate surgery(18); primary bone grafting(19); and preoperative orthodontic treatment(20). Interestingly, it was also observed that non-treated cleft patients usually have a normal maxillary growth(21,22).
The information apprehended from the questionnaires shows that 89% of the plastic surgery centers in Brazil assist patients with cleft lip and/or palate. In 75% of these centers, at least three other specialties can assist cleft patients, including dentistry and speech therapy. In conclusion, cleft patients can be assisted by multidisciplinary team with specialized professionals in most of the centers evaluated.
Approximately 62% of the centers evaluated perform less than 5 primary surgeries per month and 55% execute less than 5 secondary surgeries. Only 25% perform more than 10 primary surgeries per month and 10% make more than 10 secondary surgeries. These data show that cleft patients can be assisted throughout the country, but 25% of the centers that perform a high number of surgeries per month are in the following States: São Paulo, Rio de Janeiro, Rio Grande do Sul, Paraná, Minas Gerais, Bahia, Goiás, Pernambuco and Piauí. At least 80% of the surgeries are executed in the State of São Paulo, whose area comprises approximately 3% of the national territory.
Sixty-two percent of the centers perform less than 5 surgeries per month and do not receive any special funds to assist cleft patients. Consequently, surgeons may not be highly trained and treatment protocols may not exist. According to the abovementioned, 60% of the centers consider their team incomplete to assist cleft patients and 75% would like to have some other specialty working together. This demonstrates that these centers are interested in improving their assistance.
Most of the centers that perform a high number of surgeries do not belong to the Brazilian Plastic Surgery Society. The reason for this may be that cleft patients treatment is a subspecialty, and most of the recognized centers are school hospitals that have to train surgeons and treat different diseases.
Most of the surgeries in Brazil are performed in the age groups recommended by the main reference centers in the world: cleft lip - from 3 months old; cleft palate - around 18 months old; alveolar bone grafting - after 8 years old. The best age group to perform surgeries has not been defined by the medical literature. Chiloplasty and/or palatoplasty have been described as early as the first week of life and as late as 12 months old for chiloplasty and 2 years old for palatoplasty. Secondary surgeries are more frequent after the age of 15, but can be done after the age of 2.
Millard's technique is the most used for unilateral cleft lip. For bilateral cleft lip, Spina's or Millard's techniques are equally used. Veau's, von Langenbeck's, Wardill-Kilner's or Furlow's techniques are applied to perform palatoplasty in Brazil and in other countries. Sixty-five percent choose a technique for palatoplasty according to the cleft feature.
Questions related to bone grafting and velopharyingeal insufficiency were not answered by several centers. There are many possible reasons for that: the techniques were not familiar, the indication and results were not known, the auxiliary tests were not performed, there were difficulties in contacting the specialist that would make the procedure, and others. Velopharyngeal insufficiency was reported in less than 20% of the cases in the centers that answered the questions, the same percentage reported by Witt et al. (1998). In addition, the techniques utilized to correct this abnormality are the same as applied worldwide, such as pharyngeal flaps and pharyngoplasty.
Patients admission lasted less than 3 days in most of the centers. This is a positive fact, because short admissions mean reduced costs. A large number of centers assist patients from other States, and usually do not offer the patient and his companion any facilities, such as transportation or lodging.
According to the Health Ministry data, the number of hospital admissions for cleft lip and/or palate impressively increased in the last 5 years. There were 9,696 admissions in 1995 and 21,022 in 1999. This difference basically reflects the variation in the admissions in the State of São Paulo, that were 6,463 in 1995 and 17,636 in 1999.
There was also an increased number of primary treatment performed in patients older than the recommended age group, and secondary treatment performed between the age of 10 and 19. The first may reflect a delay in beginning the treatment, and the latter an increased search for good functional and esthetic results due to social and cultural pressures. In addition, technological developments allow different surgical techniques and complex procedures, with less risks. Consequently, there are more surgeries for refinement, bone grafting, maxillary expansion, pharyngeal flaps, etc.
The data also suggest that there has been an improvement in deft patients treatment performed in Brazil, and a higher number of patients have been assisted. This happened mainly in the State of São Paulo, because its large reference centers attract funds. Nevertheless, several other cities throughout the country with competent professionals and a good volume of patients should also receive equivalent funds from government. This would result in a better assistance to deft lip and/or palate patients in the whole country.
Concentrating the centers in one region makes the treatment very expensive or even impracticable in a large country. It would be better to have the regional centers developed, well equipped, and relying on a multidisciplinary team. This could also improve campaigns and facilitate low-income population access to treatment. In order to achieve this, it would be necessary to overcome initial difticulties and local interests, but the results would be saving money, improving treatment quality, and assisting more patients. The whole treatment for deft patients can last for decades and it is better done in a center dose to where they tive.
Campaigns to treat deft patients take the professionais to the patients. The health care providers give information about the disease, and perform significant number of surgeries. The surgeries can improve the function and esthetic in patients who otherwise would never receive any treatment. But, campaigns can also be considered palliative and far from the ideal treatment provided by a multidisciplinary team.
CONCLUSIONS
1) Being assisted by a multidisciplinary team is fundamental for deft lip and/or palate treatment.
2) There is no consensus about treatment protocols.
3) The best results are obtained by centers that adopt a protocol, have a well-trained surgical team, and perform long-term follow-up.
4) There are several centers that could provide a multidisciplinary assistance to cleft patients.
5) There is an evident concentration of centers in São Paulo.
REFERENCES
1. BARDACH J, MORRIS HL, OLIN WH, GRAY SD, JONES DL, KELLY KM, SHAW WC, SEMB G. Results of multidisciplinary management of bilateral cleft lip and palate at the Iowa Cleft Palate Center. Plast. Reconstr. Surg. 1992;89(3):419-35.
2. NOAR JH. A questionnaire survey of attitudes and concerns of the three professional groups involved in the cleft palate team. Cleft Palate-Craniofac. J. 1992;29(1):92-5.
3. SHAW WC, DAHL E, ASHER-McDADE C, BRATTSTRÖM V, MARS M, McWILLIAM J, MOLSTED K, PLINT DA, PRAHL-ANDERSEN B, ROBERTS C, SEMB G, THE RPS. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 5. General discussion and conclusions. Cleft Palate-Craniofac. J. 1992;29(5):413-8.
4. SPINA V. Bilateral harelip surgery. A new concept. In: Owens, N., ed. Transactions of the 3rd International Congress of Plastic Surgery, Washington, D.C. 1963, Amsterdam Excerpta Medica Foundation, 1964;314-23.
5. ROHRICH RJ, ROWSELL AR, JOHNS DF, DRURY MA, GRIEG G, WATSON DJ, GODFREY AM, POOLE MD. Timing of hard palatal closure: a critical long-term analysis. Plast. Reconstr. Surg. 1996;98(2):236-46.
6. McWILLIAMS BJ, RANDALL P, LAROSSA D, COHEN S, YU J, COHEN M, SOLOT C. Speech characteristics associated with the Furlow palatoplasty as compared with other surgical techniques. Plast. Reconstr. Surg. 1996;98(4):610-21.
7. BROTHERS DB, DALTSON RW, PETERSON HD, LAWRENCE T. Comparison of the Furlow double-opposing Z-palatoplasty with the Wardill-Kilner procedure for isolated clefts of the soft palate. Plast. Reconstr. Surg. 1995;95(6):969-77.
8. WITT PD, WAHLEN JC, MARSH JL, GRAMES LM, PILGRAM TK. The effect of surgeon experience on velopharyngeal functional outcome following palatoplasty: is there a learning curve? Plast. Reconstr. Surg. 1998;102(5):1375-84.
9. LESSA S. Insuficiência velofaringeana. In: Carreirão S, Lessa S, Zanini SA eds. Tratamento das fissuras labiopalatinas. 2a ed., Rio de Janeiro, Editora Revinter, 1996: 237-51.
10. ZANINI LS. Avaliação do uso da técnica de Furlow para tratamento da insuficiência velofaríngea. Monografia apresentada para ascensão à categoria de Membro Titular da Sociedade Brasileira de Cirurgia Plástica, 1997.
11. COLLARES MVM. Comunicação Pessoal. Chefe do Departamento de Cirurgia Maxilofacial do Hospital de Clínicas de Porto Alegre, RS, 1999.
12. MOLSTED K, DAHL E, SKOVGAARD LT, ASHER-McDADE C, BRATTSTRÖM V, McCANCE A, PRAHL-ANDERSEN B, SEMB G, SHAW B, THE R. A multicentre comparison of treatment regimens for unilateral cleft lip and palate using a multiple regression model. Scand. J. Plast. Reconstr. Hand Surg. 1993;27:277-84.
13. ROBERTS-HARRY D, SEMB G, HATHORN I, KILLINGBACK N. Facial growth in patients with unilateral clefts of the lip and palate: a two-center study. Cleft Palate Craniofac. J. 1996;33(6):489-93.
14. SEMB G. A study of facial growth in patients with bilateral cleft lip and palate treated by the Oslo team. Cleft Palate Craniofac. J. 1991;28(1):22-39.
15. SEMB G. A study of facial growth in patients with unilateral cleft lip and palate treated by the Oslo team. Cleft Palate Craniofac. J. 1991;28(1):1-21.
16. MOLINA F, MONASTERIO FO, AGUILAR MP, BARRERA J. Maxillary distraction: aesthetic and functional benefits in cleft lip-palate and prognathic patients during mixed dentition. Plast. Reconstr. Surg. 1998;101(4):951-63.
17. KAPUCU MR, GÜRSU KG, ENACAR A, ARAS S. The effect of cleft lip repair on maxillary morphology in patients with unilateral complete cleft lip and palate. Plast. Reconstr. Surg. 1996;97(7):1371-8.
18. FREITAS JAS, MAZZOTTINI R, CAPELOZZA Fº L, FREITAS PZ. Avaliação das alterações do arco dentário superior em indivíduos portadores de fissura transforame incisivo unila-teral. Ortodontia. 1995;28(1):18-26.
19. SILVA Fº OG, FERRARI JR. FM, CAPELOZZA Fº, ALBUQUERQUE MVP. Enxerto ósseo alveolar em pacientes fissurados: realidade e perspectiva. Ortodontia. 1995;28(1):34-45.
20. SHAW WC, DAHL E, ASHER-McDADE C, BRATTSTRÖM V, MARS M, McWILLIAM J, MOLSTED K, PLINT DA, PRAHL-ANDERSEN B, ROBERTS C, SEMB G, THE RPS. A six-center international study of treatment outcome in patients with clefts of the lip and palate: part 5. General discussion and conclusions. Cleft Palate-Craniofac. J. 1992;29(5):413-8.
21. PITANGUY I, FRANCO T. Nonoperated facial fissures in adults. Plast. Reconstr. Surg. 1967;39(6):569-577.
22. BUSCHANG PH, SCHROEDER JN, GENECOV E, SALYER KE. Growth status of children treated for unilateral cleft lip and palate. Plast. Reconstr. Surg. 1991;88(3):413-419.
I - TCBC, TSBCP, Master degree in Plastic Surgery by the Univeridade Federal do Rio de Janeiro, Ph.D in course in the Surgery Department of the Universidade Federal do Rio de Janeiro.
II - TCBC, TSBCP, F.I.C.S., F.A.C.S., Member of the National Medicine Academy, Head in Chief of the Plastic Surgery Center at the Hospital Universitário da Universidade Federal do Rio de Janeiro (UFRJ).
Address for correspondence:
Diogo Franco, MD
Praia de Botafogo, 528 apto. 1304-A
22250-040 - Rio de Janeiro - RJ Brazil
Fax: (55 21) 542-7119
e-mail: diogo@openlink.com.br
Study performed in the Plastic Surgery Center of the Hospital Universitário Clementino Fraga Filho at the UFRJ.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license