ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Superior Orbitary Fissure Syndrome by Face Trauma Without Medial Third Fracture - Case Report
Síndrome da Fissura Orbitária Superior por Trauma de Face sem Fratura de Terço Médio - Relato de Caso
Case Reports -
Year2000 -
Volume15 -
Issue
2
Antônio Albuquerque BritoI, Rodolfo ValdemarinII, Renato Tatagiba GarciaII, Carlos Eduardo Guimarães LeãoIII
ABSTRACT
The aim of this work is to present a clinical case of the Superior Orbitary Fissure Syndrome in a patient with face trauma without medial third fracture and to establish a correlation of this injury with the orbitary commitment, suggesting that its ethiology is due to the impact force transmission throughout the pillars of the face's reticulated sheleton up to the orbit. The necessity of the knowledge of this ethiopathological mechanism is stressed and the diagnostic and therapeutical of this syndrome are the discussed aspects.
Keywords:
Superior orbital fissure syndrome; ophthalmoplegia; facial trauma; palpebral ptosis; mydriasis
RESUMO
O objetivo do presente trabalho é apresentar um caso clínico de síndrome da fissura orbitária superior numa paciente com trauma de face sem fraturas do terço médio e estabelecer uma correlação dessa injúria com o acometimento orbitário, sugerindo que sua etiologia seja a transmissão da força do impacto através dos pilares do esqueleto reticular da face, até a órbita.
Enfatizamos a necessidade do conhecimento desse mecanismo etiopatológico e discutimos aspectos diagnósticos e terapêuticos da referida síndrome.
Palavras-chave:
Síndrome da fissura orbital superior; oftalmoplegia; trauma facial; ptose palpebral; midríase
INTRODUCTION
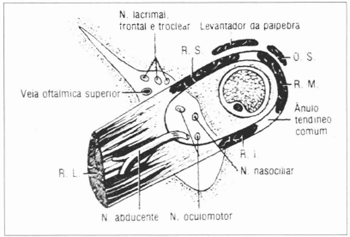
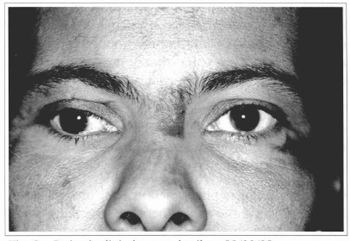
The Superior Orbitary Fissure Syndrome (SOFS) was described by Hirchfield in 1858(1), and was characterized by ophthalmoplegia, superior palpebral ptosis, eye proptosis, mydriasis and frontal region and superior eyelid anesthesia due to the concurrent or not lesion of the III, IV and VI cranial pairs, first division of the V cranial pair and autonomic innervation of the eye globe and its extrinsic muscular(1,2)(Fig. 1). This nosological entity's ethiology varies: medial segment fractures of the facial bones, neoplasias, retrobulbar hematomas and sinus carvernosus, meninges or central nervous system infections(2).
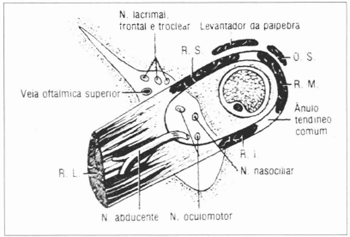
Fig. 1 - Anatomical structures of the orbit apex, according to Gardner.
This work's purpose is to report a SOFS clinical case in a patient with face trauma without medial third fractures and without clinical and tomographic evidences of sphenoidal fracture or evident pathologies at the orbit apex, such as retrobulbar hematoma, and correlate the entiry's ethiopathology to the impact force transmission throughout the superficial medium third of the facial skeleton towards the endocranium, as presented by Sturla(3).
CASE REPORT (MATERIAL AND METHODS/ RESULT)
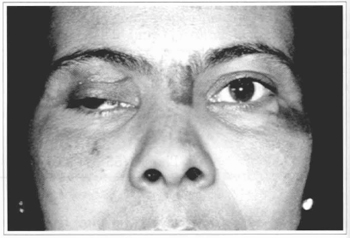
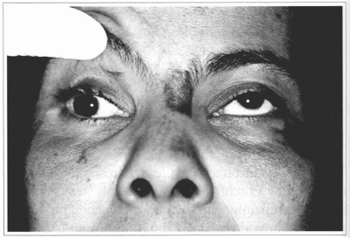
31 years old female patient was hit by a car. She reports trauma at the right hemiface and diplopia. During the physical examination, she presented proptosis, excessive infero-lateral abduction and rotation of the eye, palpebral ptosis, unilateral mydriasis to the right, and divergent strabismus. Denied frontal region parestesia (Figs. 2 and 3). She also presented buccal opening limitation, occlusal dystopia and edema to the right of the mandible.
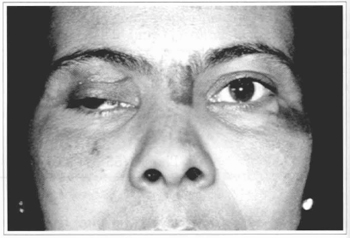
Fig. 2 - Patient's clinical aspect; note the palpebral ptosis and divergent strabismus to the right.
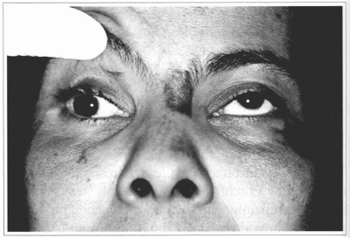
Fig. 3 - Detail of the ophtalmoplegia to the right (superior view).
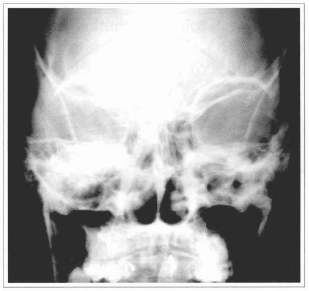
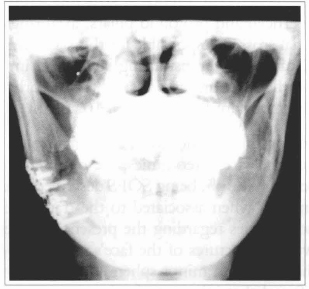
The radiological examination revealed fracture of the body of the mandible to the right, and no fractures at the medial third or endocranium, only a discrete velamentum of the right maxillar sinus was observed (Fig.4).
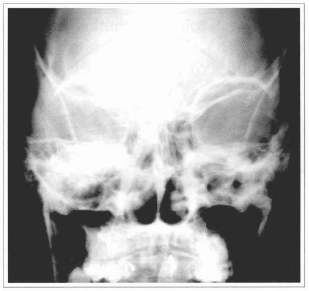
Fig. 4 - Radiographic aspect; note the innominated line integriry to the right and the absence of fracture signals at the medial third.
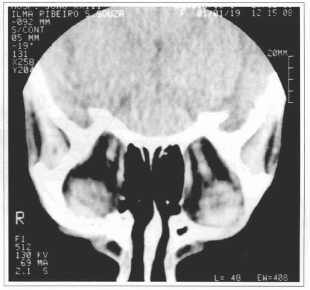
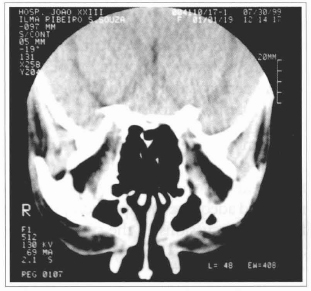
The tomographies didn't show cranial or orbital fractures, as well as orbitary cone's soft tissue alterations, except by a density increase at the extrinsic musculature of the eye globe. There were no signals of orbitary apex compression (Figs. 5 and 6).
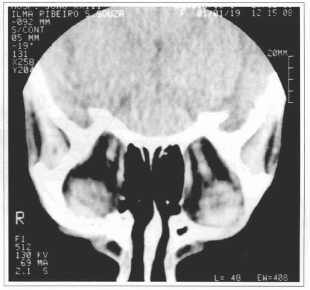
Fig. 5 - Coronal cut tomography, note the orbit apex integrity.
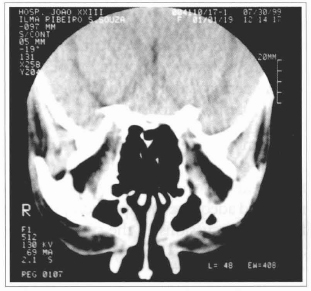
Fig.6 - Caronal cut tomography; note the absence of right compression signals of the orbitary apex.
The mandible's body fracture to the right and SOFS were diagnosed.
The patient underwent the mandible's fracture reduction on 07/21/99, with a rigid fixation, without intermaxillar block (Fig. 7). The SOFS conservative treatment was chosen, together with the sequential ophtalmological follow-up and prednisone administration.
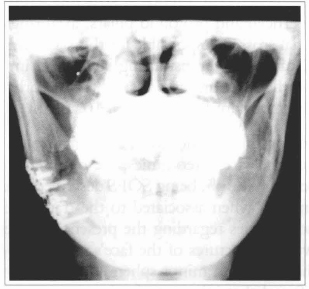
Fig. 7 - Radiographic aspect of the mandible's fracture treatment.
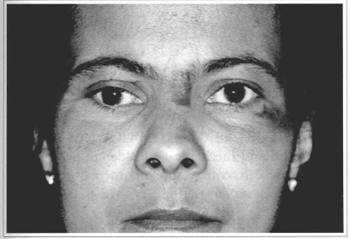
At the last assessment performed on 08/30/99, a partial improvement of the SOFS' signals and symptoms was evidenced (Figs. 8 and 9).
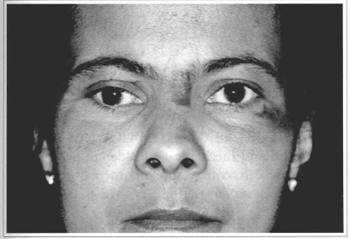
Fig. 8 - Patient's clinical aspect on 08/30/99. Note the improvement of the palpebral ptosis and mydriasis to the right.
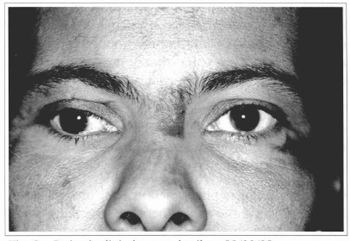
Fig. 9 - Patient's clinical aspect detail on 08/30/99.
DISCUSSION
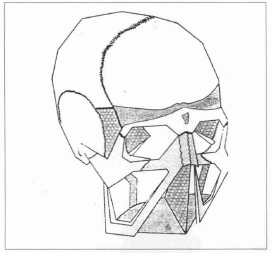
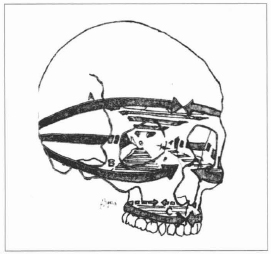
With the purpose of providing an adequate assessment of the craniofacial traumas, STURLA (1980), supported by the 1901 works(4) of René Le Fort, developed an experimental study in which he presented the face's fixed skeleton as a reticular structure, comprised of superficial and profound pillars, axial rings and craniofacial crosses, responsible for this skeleton's support and capable of transmitting superficial impact forces to the profound regions, where the orbit is particularly important for us(3) (Figs. 10 and 11).
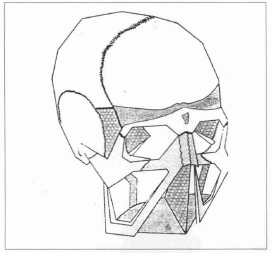
Fig. 10 - Reticular structure of the facial skeleton, according to Sturla.
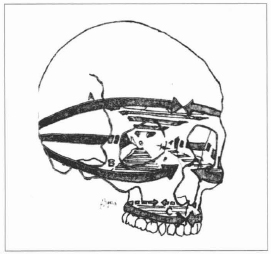
Fig. 11 - Craniofacial rings, according to Sturla.
The ophtalmological complications, associated to the facial traumas and face osteotomies, are reported in the literature(1,2,5,6,7,8,9,10), being SOFS described as a rare entiry, mainly when associated to the trauma(2). There are no statistics regarding the presence of the syndrome without fractures of the face's medial segment and the major and minor sphenoid wings. For that, it is inferred that injury mechanism is indirect, as suggested by Lanigan(6,10), and that takes us back to Sturla (3)previously cited observations, and is illustrated by the clinical case herein presented. The facial trauma can have its impact force transmitted throughout the face's medial skeleton pillars, affecting the orbitary apex and promoting this topography's neurovascular structures compression, even without evidences or fractures or retrorbitary hematomas.
This pathology diagnosis is clinical, and a cranial and orbit tomographic study must be requested in order to observe the orbitary apex fractures or other evident signals of compression(6,7,10,11).
Once that vascular phenomenons can progressively appear, affecting the orbit's nervous structures, a sequential ophthalmological assessment must be installed.
The SOFS treatment in case of trauma is conservative in the majority of the cases, and steroids can be used with the clinical improvement in a variable period of time (3 weeks to 4 months). The orbit decompression is performed in a endocranial or transfacial way in the rarest situations(1,2,8,10).
The clinical case presented stresses the necessity of knowing the impact conduction mechanisms of the face traumas, orientated as to perform an early diagnosis and adequate therapeutical procedure of the profound repercussions of the superficial injuries.
REFERENCES
1. ZANINI SA, MOCCELIN JV, SCHIEFFERDECKER S, MIGOWSKI Jr W. Síndrome da fissura orbitária superior. Rev. Soc. Bras. Cir. Plást. 1985;0:73-75.
2. ZACHARIADES N,VAIRAKTTARIS E, PAPAVASSILIOU D, PAPADEMETRIOU I, MEZITIS M, TRIANTAFYLLOU D. The superior orbital fissure syndrome. J. Maxillofac. Surg. 1985;13:125-128.
3. STURLA F, ADSI D, BUQUET J. Anatomical and mechanical considerations of craniofacial fractures: an experimental study. Plast. Reconstr. Surg. 1980;66:815-820.
4. LE FORT R. Estudo experimental sobre fraturas do maxilar. Rev. Fac. Odont. P. A. 1961;3:137-199.
5. CRUZ RJL. Fraturas do ápice da órbita, in Cirurgia Craniomaxilofacial: Osteotomias Estéticas da Face. 1987; p.599-606 - Ed. Medsi.
6. LANIGAN DT, ROMANCHUK K, OLSON CK. Ophtalmic complications associated with orthognathic surgery. J. Oral Maxillofac. Surg. 1993;51:480-494.
7. MANFREDI SJ, RAJI MR, SPRINKLE PM, WEINSTEIN GW, MINARDI LM, SWANSON TJ. Computerized tomographic scan findings in facial fractures associated with blindness. Plast. Reconstr. Surg. 1981;68:479-490.
8. ORD RA, EL ATTAR A. Acute retrobulbar hemorrhage complicating a malar fracture. J. Oral Maxillofac. Surg. 1982;40:234-236.
9. POGREL MA. The superior orbital fissure syndrome: report of case. J. Oral Surg. 1980;38:215-217.
10. SEIF SR, BERGER MS, GUYON J, PITTS LH. Computed tomographic evaluation of the optic canal in sudden traumatic blindness. Am. J. Ophthalmol. 1984;98:751-755.
11. MARCIANI RD. Management of midface fractures: fifty years later. J. Oral Maxillofac. Surg. 1993;51:960-968.
I - Physician/Surgeon-Dentist - Buccomaxillofacial Surgery Unit Coordinator of Fundação Hospitalar do Estado de Minas Gerais - FHEMIG.
II - Resident doctors at the Plastic Surgery Service of FHEMIG.
III - Head of the Plastic Surgery Service of FHEMIG.
Address for correspondence:
Av. Contorno, 8000 sl. 507
30110-120 - Belo Horizonte - MG Brazil
Phone: (55 31) 335-4679
Fax: (55 31) 335-4679
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license