

Articles - Year 2000 - Volume 15 -
The Use of Osteointegrated Implants Craniofacial Deformities
Aplicação de Implantes Osteointegrados nas Deformidades Craniofaciais
ABSTRACT
Craniofacial deformities are a challenge for multidisciplinary teams. The treatment requires complex surgeries, performed by stages. The cosmetic results are limited due to the innumerous details of the face. A new and interesting alternative for the treatment of craniofacial defonnities consists in using osteointegrated implants as anchoring elements for prosthesis. This article deals with the conditions and results of osteointegrated implants and prosthesis carried out at Hospital A. C. Camargo - Fundação Antônio Prudente (SP) from 1995 to 1999, totaling 33 osteointegrated implants in 12 patients.
Keywords: Craniofacial implants; osteointegration; rehabilitation; craniofacial deformities
RESUMO
As deformidades craniofaciais são um desafio para as equipes multidisciplinares. O tratamento requer cirurgias complexas e realizadas em etapas. Os resultados estéticos são limitados perante a riqueza de detalhes que as regiões da face exigem. Uma nova e interessante alternativa de tratamento das deformidades craniofaciais é a aplicação de implantes osteointegrados como elementos de sustentação para próteses. Este trabalho discorre sobre as condições e os resultados dos implantes osteointegrados e próteses feitos no Hospital A. C. Camargo - Fundação Antônio Prudente (SP), no período de 1995 a 1999, com um total de 33 implantes osteointegrados em 12 pacientes.
Palavras-chave: Implantes craniofaciais; osteointegração; reabilitação; deformidades craniofaciais
Nowadays, oncologic patients need to be socially reintegrated as part of the multidisciplinary treatment of cancer. Old age, extension of the surgical resection, radiotherapy and the details inherent to craniofacial deformities (CD) make the reconstruction very elaborated. We can repair a wound, but we can not restore the original characteristics of a region.
Regarding the congenital CDs, the plastic surgeon's work is also very hard due to the cosmetic demands, the changes in growing segments and the participation of multidisciplinary teams.
In traumatic CDs, the situation is almost the same, aggravated by the patient's conception of his/her appearance before the trauma.
Whether the cause is congenital or acquired, CD treatment is complicated by one or more circumstances: old age, and physical or mental restrictions. In such cases, the patient is not fit to undergoing multiple surgeries, may not understand the limitations of results, may not accept the donor areas or may not resign himself/herself to partially or totally unsuccessful reconstruction attempts.
The plastic surgeon has to ponder and decide which is the best reconstruction method for each case. The use of a prosthesis may be a simpler option, producing faster rehabilitation with less risks, better cosmetic results and lower costs.
Regarding the prosthesis, two aspects should be considered: the cosmetic result provided by the selected material and the prosthesis retention. In our country, many prosthesis are still made of acrylic resin. This material presents some difficulties for cosmetic characterization and margin adaptations. Glasses and adhesives are some of the accessories used for prosthesis retention, but they are not comfortable and may cause: 1) dermatitis and allergies; 2) prosthesis material deterioration; 3) apprehension concerning the prosthesis fixation, which is aggravated by perspiration and tissue movements; 4) improper positioning of the prosthesis.
The advent of the osteointegration concept(1-4) and improvements in prosthesis materials provided good retention and refined cosmetic definitions.
Osteointegration is the direct contact of the bone with the prosthesis, that is, the absence of connective tissue between bone and metal. Over 1 million Branernark implants (Nobelpharma AB, Gothenburg, Sweden) have been inserted all over the world. Due to its success in oral rehabilitation, the osteointegration concept, introduced by Prof. Anders Tjellström(2)(University of Gothenburg, Sweden) in 1977, has extended to the craniofacial region as a consequence.
Since 1994, the Hospital A. C. Camargo has been developing a project for the creation of a craniofacial rehabilitation sector, supported by the Hospital of the University of Gothenburg (Sweden), Otorhinolaryngology Department, and the Prof. P.I. Branemark's Applied Technology Institute.
The purpose of this article is to present a proposal for the use of osteointegrated implants (OI) in the treatment of craniofacial deformities.
CASUISTICS AND METHODS
The study was developed at the Hospital A. C. Camargo - Fundação Antônio Prudente (SP), from 1995 to 1999.
The Hospital A. C. Camargo received technical support from the Hospital of the University of Gothenburg (Sweden), Otorhinolaryngology Department, and the Prof. P.I. Branemark's Applied Technology Institute.
A multidisciplinary team involving specialists in Head and Neck Surgery, Ophthalmology, Radiotherapy, Pediatrics and Clinical Oncology for cancer staging and treatment examined the patients. The surgeries were carried out by Plastic Surgery and Maxillofacial Surgery specialists, in order to treat the deformities resulting from the oncologic treatment.
• 12 patients were admitted into the osteointegration rehabilitation programo
• 33 OIs have been inserted:
√ 17 OIs of 3 mm in length x 3,75 mm in diameter
√ 16 OIs of 4 mm in length x 3,75 mm in diameter
The implants were made of titaniurn, according to the Branemark System Technique (Nobelpharma AB, Gothenburg, Sweden), with the collaboration of Anders Tjellströrn (Gothenburg, Sweden). After a period of approximately six months, the OIs were connected to the prosthesis.
The steps, from the OI number planning to the prosthesis elaboration, were the following:
1st step - Implant insertion, under general anesthesia. The implants remained totally covered by soft parts for a 6-month rest. Note: An extra OI (besides the expected one) was inserted in case one OI failed.
2nd step - Abutment installation, under general anesthesia, with implant exposition and soft part regularization around the implants, as required.
3rd step - Bed molding for the prosthesis elaboration with silver-palladium metallic frame and gold cylinders to be anchored to the implant abutments. In this step, the general anesthesia was not necessary.
Prior to surgery, the patients were examined by an oncologist, being considered fit to go on reconstruction by the multidisciplinary team of Hospital A. C. Camargo.
The imaging investigation was carried out by means of conventional radiology and tomography. (Note: the patients with implants could not undergo Magnetic Resonance due to the metal interference in the image).
During the surgery, patients received prophylactic therapy with antibiotics - cephalexin 1g each 4 hours or clindamycin 0.6 g each 6 hours.
The prosthesis molding was carried out with alginate and the model was made of plaster of Paris, wax or acrylic resin. The definite prosthesis were made of silicone, from the model, and the proper color was obtained by intrinsic and extrinsic means.
The patients were clinically and radiologically followed after surgery; they were also instructed on how to clean the skin around the OI: brushing it with water and antiseptic agents.
RESULTS
Among the 12 patients of the OI program there were 9 males and 3 females.
Their age ranged from 3 to 77 years.
There were no anesthetic complications in the first and second steps.
The patients did not have bone pain related to the implants. They reported only slight pain in surgical incision areas when the soft parts adjacent to the irnplants had to be resected in the second step.
The deformities were the following:
• Absence of the eye and lids resulting from orbital exenterations in 8 patients, who received 24 OIs;
• Partial or complete absence of the pinna in 3 patients, who received 7 OIs;
• Partial absence of the nose in 1 patient, who received 2 OIs.
Only 2 of the 33 OIs did not integrate to the bone, according to the clinical and radiological monitoring, and had to be removed. The OI lack of firmness was associated to radiotherapy. The 2 removed OIs did not show osteomyelitis and the bone was totally repaired after the OI removal. In both cases, the OI removal did not prevent the prosthesis use beca use the remaining OIs were strong enough to bear the prosthesis load. There was only an extra OI (besides the expected one).
Details on the patients in the OI program are shown in Table I below.
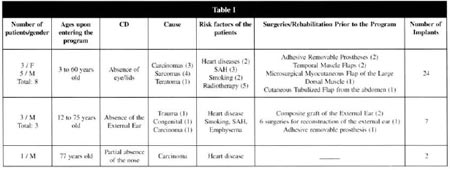
By analyzing the patient data, one can note that:
1) The most frequent cause of CD was the basal cell carcinoma and prickle cell carcinoma.
2) The risk factors were those related to systemic arterial hypertension, heart disease, smoking, and mainly radiotherapy.
3) In the group of patients with CD due to absence of the eyeball and lids, seven patients had looked for some kind of rehabilitation, whether by means of reconstructive plastic surgery or adhesive prosthesis. With time, the adhesive prosthesis caused dermatitis and superficial ulcerative injuries in skin. These skin alterations hindered the use of the removable adhesive prosthesis for some weeks, affecting the patient social life. The myocutaneous flap of the temporal muscle and microsurgical flap of the latissimus dorsi, applied in this group of patients before their admission into the OI program, were meant to give protection against injuries. They were not meant to redefine the orbital structures. Figures 1-5 show an example of CD by absence of the eyeballs and lids after surgery to remove prickle cell carcinoma, as well as the implants being inserted, the prosthesis being positioned and the final result of the prosthesis in place.
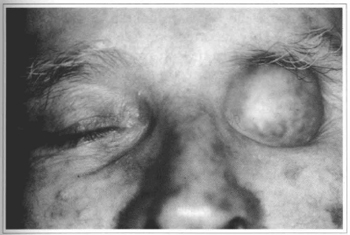
Fig. 1 - A 63-year-old patient with orbital deformity resulting from prickle cell carcinoma resection.

Fig. 2 - Three osseointegrated implants being inserted in the upper orbital margin (1st step).
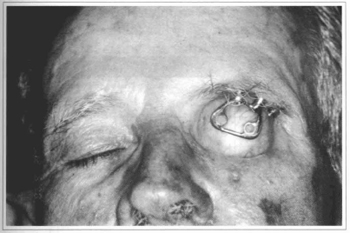
Fig. 3 - Metallic frame for prosthesis retention.

Fig. 4 - Orbital prosthesis with defined intrinsic and extrinsic coloring.
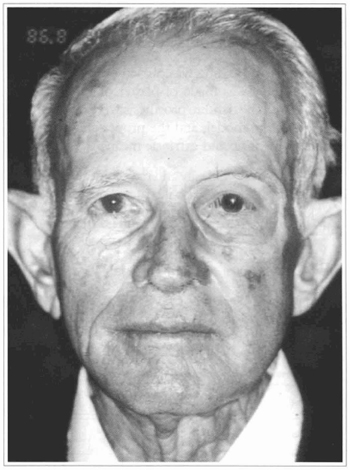
Fig. 5 - Final appearance of the prosthesis in place.
4) In the group of patients with CD by absence of the pinna, one of them had suffered traumatic ablation of the pinna and received a pinna graft, with total loss. The non-acceptance of donor areas was the main reason why this patient entered the OI program. Another patient with microtia, before ente ring the OI program, had undergone six surgeries to reconstruct the pinna. In the last one, the surgeon had implanted a silicone prosthesis. Silicone was banished from the OI program because of the serious fibrosis in that region and poor cosmetic definition.
Figures 6-10 show an example of CD by absence of the ear resulting from trauma, as well as the implant being inserted in the mastoid, the fixing bar with magnets, the prosthesis detail and the final result.

Fig. 6 - A 12-year-old patient with traumatic auricular deformity.

Fig. 7 - Three osseointegrated implants being inserted in the mastoid.
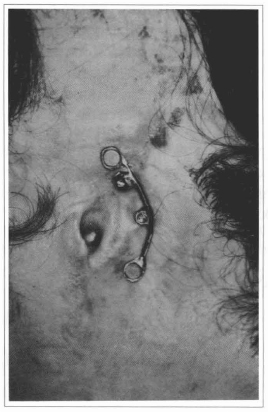
Fig. 8 - Metallic bar that supports the auricular prosthesis.
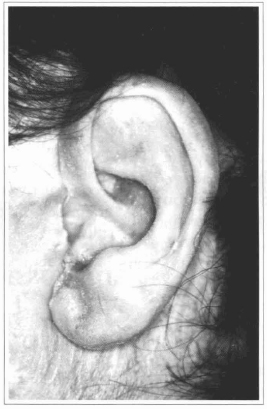
Fig. 9 - Detail of the auricular prosthesis.
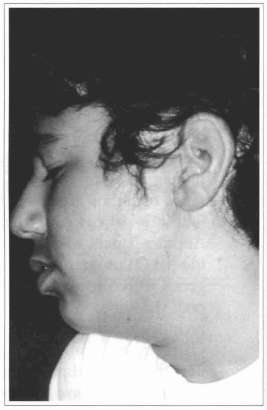
Fig. 10 - Final appearance of the prosthesis in place.
5) Only one patient in the group of CDs by partial absence of the nos e entered the OI program due to the difficulty in inserting OIs in this region and the current practice of conventional nasal reconstruction surgeries. This patient was admitted into the OI program because the donor areas for nasal reconstruction were deformed in consequence of previous surgeries.
On entering the OI program, the patients were anxious and dissatisfied with the adhesive prosthesis and cosmetic results of previous reconstructive surgeries, with their complications and limitations.
However, the silicone prosthesis connected to the OIs produced good cosmetic results and deep satisfaction. This was because such prosthesis are easy to put and clean, and have a wide range of colors and shapes. After a period of approximately one year, only one ear prosthesis with OI required minar corrections in painting (extrinsic coloring).
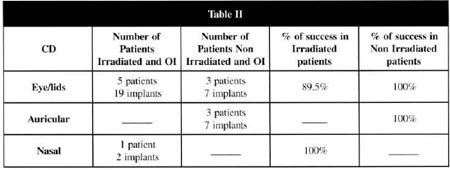
Table II shows the rate of success related to the CDs and me associated radiotherapy.
About 10% of me patients presented some kind of tissue reaction around the abutments, but no removal was necessary. With proper cleanness around me implant, me tissue reaction subsided or even disappeared.
The patients cooperated with the regular follow-up after surgery and neither show the fears related to other reconstructive surgeries performed before me OI program, nor the troubles with donor areas and bad results.
DISCUSSION
The osteointegrated implanting has been performed in several institutions for more than 10 years(1,3). However, in Brazil, few institutions have employed this rehabilitation method because of the material costs and specific knowledge required.
For 30 years, since the first experiences with osteointegration (1,3), two conditions were found essential for the success. The first, which consists in the correct bone perforation technique methodology, was associated to the metal (titanium) quality, part models, accuracy of perforation and the necessary rest time until the implant is ready to bear the load (prasthesis weight). The second condition involves the bone quality, mainly in function of the cortex thickness. Thicker bones are better. As important as bone thickness were the surgical accessibility of the region for OI insertion and the proper implant hygiene by the patient.
According to other publications(1,3), the mastoid region was the safest for OI use, with 100% success at Hospital A. C. Camargo. These fine results were due to the great amount of cortical bone, easy surgical accessibility and easy hygiene instructions.
According to statistics from other publications(1,3), the orbital region had 70 to 85% success with the OIs. This rate was lower than that of the mastoid region because of the lower orbit thickness (whether in the upper margin or in the lower margin), depending on the face sinus extension. Despite our modest casuistics, the success rate at Hospital A C. Camargo was 89.5% for these CDs.
The nasal region had the worst success rates with the OIs, 60 to 75%, as observed in other institutions(1,3). These rates can be explained by: thin cortex of the maxilla, difficult surgical access, difficult hygiene and the presence of teeth. At the Hospital A. C. Camargo, the only patient with this kind of CD was successfully treated.
It was found that the quality of the skin layer around the implants was better, with lower incidence of phlogosis, when the hypodermis was thin and the dermis was poor in hair follicles. In such case, a skin graft over the bone in the OI region met these conditions.
The materials used in prosthesis have showed a significant improvement in the last 10 years. Silicone was the most common material because it is easy to handle, have good resistance to traumas as well as good coloring and characterizing properties.
Regarding the CDs resulting from oncologic ablative treatments, special attention was given to those that underwent adjuvant radiotherapy. According to literature(4), the irradiated area to be rehabilitated had higher complication rates: necroses, infections and implant losses. In these cases, the treatment with hyperbaric therapy impraves the OI success rates in irradiated areas.
CONCLUSIONS
The OIs and prosthesis should be part of the CD rehabilitation options. The OIs are safe prosthesis supports for the face.
For the patient who needs ablative oncologic treatment, the multidisciplinary approach can allow the OI planning without affecting the surgery extension and effectiveness.
MESSAGE FROM THE AUTHORS
Even in a country with severe social distortions like Brazil, it is important that the most advanced treatments reach the population. The right to a good quality of life should be universal. With information and good direction, people gain confidence, overcoming the fears of a cancer diagnosis, facilitating the early identification and avoiding big mutilations.
REFERENCES
1. TJELLSTRÖM A, GRANSTRÖM G. Long-term follow-up with the bone-anchored hearing aid: a review of the first 100 patients between 1977 and 1985. Ear Nose Throat J. 1994;73(2):112-4.
2. PAREL SM, TJELLSTRÖM A. The United States and Swedish experience with osteointegration and facial prosthesis. Int. J. Oral Maxillofac. Implants. 1991;6(4):75-9.
3. BRÄNEMARK PI, DIB LL, CURI MM, GRANSTRÖM G, PIRAS JA, SEIGNEMARTIN CP. Reabilitação das deformidades craniofaciais com o uso de implantes osteointegrados. Revista da APCD. 1998;52:227-231.
4. GRANSTRÖM G, JACOBSSON M, TJELLSTRÖM A. Titanium implants in irradiated tissue: benefits from hyperbaric oxygen. Int. J. Oral Maxillofac. Implants. 1992;7(1):15-25.
I - Titular Member of the Brazilian Society of Plastic Surgery. Titular Member of the Reconstructive Plastic Surgery Department, Hospital do Câncer, Fundação Antônio Prudente, in São Paulo.
II - Dentist. Head of the Stomatology Department, Hospital do Câncer, Fundação Antônio Prudente, in São Paulo.
III - Dentist. Titular Member of the Stomatology Department, Hospital do Câncer, Fundação Antônio Prudente, in São Paulo.
IV - Dentist. Head of the Rehabilitation Division, Fundação Oncocentro, in São Paulo.
Address for correspondence:
Alexandre Katalinic Dutra, MD
R. Professor Antônio Prudente, 211
01509-900 - São Paulo - SP Brazil
Phone: (55 11) 3272-5000/5135
Hospital do Câncer Departamento de Cirurgia Plástica Reparadora


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter