

Original Article - Year 2018 - Volume 33 - Issue 2
Surgical treatment of moderate and severe ptosis: analysis of results
Tratamento cirúrgico da ptose palpebral moderada e grave: análise de resultados
ABSTRACT
Introduction: Eyelid ptosis is a common condition in clinical practice for which a complete
evaluation is mandatory. Ptosis is defined when the eyelid margin is 2 mm
below the corneoscleral junction and can be classified as mild, moderate,
and severe. There are numerous repair techniques, and the choice will depend
on the classification of the function of the levator muscle.
Methods: We evaluated prospectively, from March 2013 to May 2015, 14 patients who
underwent surgical treatment of moderate and severe ptosis (n = 21). Several
factors were studied, such as degree of ptosis and function of the eyelid
levator muscle, type of repair technique, and immediate and late
complications.
Results: Fourteen patients (21 eyelids) underwent operation. The etiology was acquired
in 85% of the cases and congenital in 15%. With respect to the degree of
ptosis, 64.3% (n = 9) of the cases were moderate and 35.7% (n = 5) were
severe. With respect to the muscle function of the levator, good, moderate,
and poor functions were observed in 28.5% (n = 4), 28.5% (n = 4), and 43% (n
= 6) of the cases, respectively. With regard to complications, 2 cases of
conjunctival hyperemia and one case of edema were observed. We obtained a
high satisfaction rate of 85.7% (n = 12), with low complication rates.
Conclusion: Eyelid ptosis is a common presentation in clinical practice and requires on
the part of the surgeon a detailed anatomical knowledge of the delicate
structure of the eyelid and its pathophysiology. A complete evaluation of
these patients is mandatory for the employment of the most appropriate
treatment.
Keywords: Blepharoptosis; Blepharophimosis; Myasthenia gravis; Fascia lata; Eyelid diseases
RESUMO
Introdução: A ptose palpebral é uma afecção comum na prática clínica na qual uma perfeita
avaliação torna-se mandatória. Definimos ptose quando a margem palpebral
encontra-se abaixo de 2 mm da junção corneoescleral e pode ser classificada
em leve, moderada e grave. Existem inúmeras técnicas de reparo e a escolha
dependerá da classificação da função do músculo levantador.
Métodos: Foram analisados de forma prospectiva, no período de março de 2013 a maio de
2015, quatorze (n = 14) pacientes submetidos ao tratamento cirúrgico de
ptose palpebral moderada e grave (n = 21). Inúmeros fatores foram estudados,
tais como grau de ptose e função do músculo elevador da pálpebra, tipo de
técnica de reparo, complicações imediatas e tardias, etc.
Resultados: Quatorze pacientes foram opera-dos, totalizando 21 pálpebras, sendo que, 85%
foram de etiologia adquirida e 15% congênita. Com relação ao grau de ptose,
64,3% (n = 9) foram moderadas e 35,7% (n = 5) graves. No que tange à função
do músculo levantador, encontramos função boa 28,5% (n = 4), moderada 28,5%
(n = 4) e pobre 43% (n = 6). Em relação às com-plicações, 2 casos de
hiperemia conjutival e um caso de edema. Obtivemos um alto índice de
satisfação com 85,7% (n = 12), com baixas taxas de complicações.
Conclusão: A ptose palpebral é uma enfer-midade comum na prática clínica e exige por
parte do cirurgião um perfeito conhecimento anatômico da delicada estrutura
palpebral e também de sua fisiopatologia. Uma perfeita avaliação desse
paciente torna-se mandatória para o emprego do tratamento mais adequado.
Palavras-chave: Blefaroptose; Blefarofimose; Miastenia gravis; Fascia lata; Doenças palpebrais
INTRODUCTION
The upper eyelids have a peculiar anatomical structure divided into three lamellae as follows: the anterior lamella, consisting of skin and orbicularis oculi muscle; the middle lamella consisting of the orbital septum, tarsus, orbital fat pad, and lifting musculature (levator and Müller’s muscles); and the composite posterior lamella composed of the mucosa1. They protect the eyeball and aid in the lacrimal pump for lubrication. The correct position and anatomy of the upper eyelid margin are comprised of half the distance between the pupil and the corneoscleral junction in the corneal limbus; when it is positioned outside this limit, ptosis or palpebral retraction may occur2.
Eyelid ptosis occurs when the eyelid edge exceeds the upper limbus of the iris by 2 mm and may even cover the pupil in more severe cases. Palpebral ptosis is classified as mild, moderate, and severe when the eyelid edge is 2-4, 4-6, and >6 mm from the upper limbus of the iris, respectively (Table 1).
| Mild | 2-4 mm |
|---|---|
| Moderate | 4-6 mm |
| Severe | > 6 mm |
The function of the eyelid levator muscle is evaluated as excellent at ≥13 mm, good between 8 and 12 mm, weak at 5-7 mm, and poor or severe at <4 mm from the levator excursion (Table 2).
| Function | Measurement of the excursion of the upper eyelid margin (mm) |
|---|---|
| Excellent | ≥13 mm |
| Good | 8-12 mm |
| Poor | 5-7 mm |
| Severe | ≤4 |
The 10% phenylephrine test is another fundamental test in the evaluation of patients with eyelid ptosis. A drop is instilled at the bottom of the cul-de-sac of each eye, and the resolution of ptosis is observed after 10 minutes. If the eyelid returns to its anatomical position, surgical procedure on the Müller muscle is indicated.
Eyelid ptosis can also be classified according to etiology, which may be acquired or congenital. Acquired ptosis can be subdivided into neurogenic, myogenic, and aponeurotic origins. Lesions of the III cranial pair and Horner’s syndrome are of neurogenic origin. Myasthenia gravis, a motor plaque disorder, is classified as of myogenic origin3. Direct trauma to the eyes4, ophthalmologic surgeries in which retractors are used to injure or disengage the aponeurosis5, craniofacial surgeries, and those of involutional or senile origin6 are of aponeurotic causes.
With regard to those with congenital etiology, which shows muscular atrophy due to failure in the embryological development of the striated fibers of the eyelid levator muscle, such as blepharophimosis syndrome2, which evolves with palpebral ptosis, epicanthus, and decrease of the palpebral fissure, and the synkinesis phenomenon of the Marcus-Gunn syndrome7.
However, another entity simulates ptosis, pseudoptosis. As the name indicates, this is not a true ptosis and occurs in situations of enophthalmos, hypertrophy of the ocular globe with fragility of the upper rectus muscle, severe dermatochalasis, and tumors of the upper eyelid. In all cases, the upper eyelid droops beyond the upper limbus of the cornea, mimicking a true ptosis.
Several techniques can be used to correct palpebral ptosis, and the choice of technique depends on the etiology, degree of ptosis, and function of the levator muscle. In mild ptosis with positive phenylephrine test, tarsoconjunctival müllerectomy, described by Fasanella and Servat in 19618, can be performed. In cases of moderate ptosis, plication or reinsertion with or without shortening of the levator muscle aponeurosis may be indicated, and in cases of severe ptosis with poor levator function, frontalis suspension is formally indicated. Therefore, the diagnostic definition of the degree of ptosis and the function of the levator muscle will define the choice of the best technique for surgical treatment.
OBJECTIVE
The aim of the present study was to prospectively analyze the results of ptosis correction, including aesthetic and functional results, in patients with moderate and severe eyelid ptosis of various etiologies operated by the author using various repair techniques.
METHODS
This was a prospective study conducted from March 2013 to May 2015, in accordance with the ethical principles of the Declaration of Helsinki. The study sample was composed of 14 patients who underwent surgical treatment for moderate and severe unilateral or bilateral ptoses. The total number of eyelids surgically treated was 21. Cases of mild ptosis were excluded and, therefore, not included in the 10% phenylephrine test.
The factors studied were etiological demographics, degree of ptosis and function of the eyelid levator muscle, type of repair technique used, immediate and late complications, reoperation rate, analysis of results, and index of patient satisfaction. All the patients underwent a photographic study before and after the surgery. The work was conducted at Barata Ribeiro Municipal Hospital and in a private clinic in Rio de Janeiro, RJ.
RESULTS
Of the 14 patients, 42.8% (n = 6) were male and 57.2% (n = 8) were female. The age ranged from 12 to 74 years, with a mean of 51 years. Regarding comorbidities, systemic arterial hypertension and diabetes mellitus were predominant, with 5 and 4 cases, respectively. Alcoholism and smoking were found in 4 cases, and only 1 case of myasthenia gravis was observed.
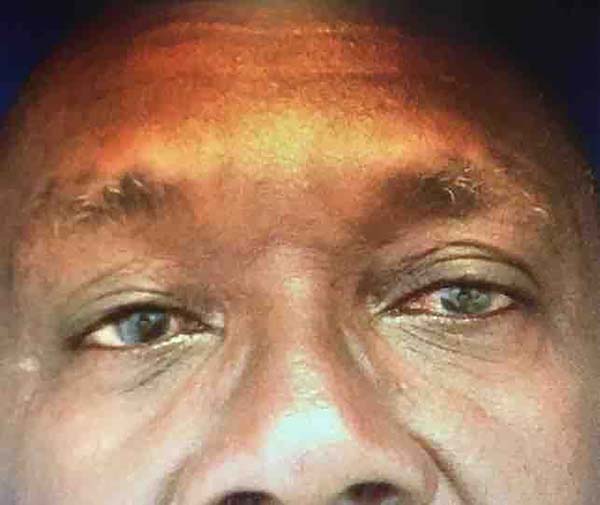
Of the 21 eyelids surgically treated, 85% had acquired ptosis and 15% had congenital ptosis (Figures 1 and 2). Among the acquired cases, involutional ptoses after ophthalmic surgeries were the most common, with 4 cases in 8 patients. Other etiologies were direct blunt trauma on the orbit (3 cases) and myasthenia gravis (only 1 case).
With respect to the degree of ptosis, 64.3% of the cases were classified as moderate; and 35.7%, as severe (Figures 3 to 5). Regarding the function of the eyelid levator muscle, 28.5% (n = 4) of the cases presented good function; 28.5% (n = 4) moderate function; and 43% (n = 6), poor function. Only one case of severe ptosis was associated with moderate levator muscle function.
The surgical technique most commonly used was the frontalis suspension surgery (9 eyelids), followed by reintegration of the aponeurosis in the tarsal plate (6 eyelids), shortening followed by reinsertion of the aponeurosis in 5 (Figures 6 and 7), and plication of the aponeurosis (1 case). In all the cases of shortening and plication, a proportion of 4:1 was used. Local anesthesia was used in all the cases, which enabled the positioning of the patient’s upper eyelid in the most anatomical position possible.
In relation to complications, 2 cases of conjunctival hyperemia of unknown etiology were treated conservatively with corticosteroids (Maxtrol®) and one case of large edema that lasted for more than a week was treated conservatively. Although common after palpebral ptosis correction surgery, eyelid asymmetries of >2 mm were considered late complications. For the cases with complications, surgical revision was indicated only in one case because the patient was a 17-year-old girl in whom asymmetry caused aesthetic impairment. We also observed a patient with mild eyelid retraction who was treated conservatively with massage.
The study results were analyzed in two ways. First, a critical analysis was performed by the author, in which the correct positioning and anatomy of the eyelids, presence or absence of significant asymmetries (those >2 mm), eyelid retraction, eyelid function, and improved aesthetics were observed. Thus, 50% (n = 7) of the cases were classified as optimal, 42.8% (n = 6) showed good results, and only one case was considered poor.
Second, the patients were asked about their opinion of the outcome. A high index of satisfaction (85.7%, n = 12) was indicated by all the patients, except two who reported that they were poorly satisfied with the outcome of the surgery.
DISCUSSION
Currently, a myriad of techniques are available for repair of palpebral ptosis. The choice of technique depends on the type, degree of ptosis, and levator muscle function. For mild ptoses, that is, those with the eyelid edge 2-4 mm from the corneal limbus, the Fasanella-Servat8 technique can be used, as cited previously but not assessed in this study.
For moderate ptosis with the eyelid edge 4-6 mm from the corneal limbus and good levator muscle function, according to etiology, we indicate reinsertion, plication, or shortening of the aponeurosis of the muscle. In 2010, Saito et al.9 published a study that analyzed two different types of approaches to the aponeurosis of the levator muscle, performing plication with a mean shortening of 9.78 mm and resection with reinsertion with a mean shortening of 14 mm, with good results in both techniques.
Alves10, in 2014, described a technique of continuous suture on the aponeurosis, with an average shortening of 12 mm with plication at a proportion of 4:1 mm, which attained good results in 92.3% of the cases.
With regard to severe ptosis with the eyelid edge >6 mm from the corneal limbus and with poor levator muscle function (Figures 8 and 9), the frontalis suspension is formally indicated. The use of the fascia lata in the form of small bundles of 2 mm in width is the most commonly used technique, as described by Crawford in 195611. As this is a fascial graft, an autologous inert tissue, the immediate complication and recurrence rates are. Several studies12-16 showed the safety of the procedure, with a low complication rate and good results in the short and long terms, even in children aged <3 years15,16.
In our sample, the fascia lata was used in 100% of the cases with severe ptosis and poor levator muscle function (Figures 10 and 11). We used small bands of 2 × 60 mm in W formation in a plane below the orbicularis muscle, harvested from the lateral aspect of the non-dominant thigh through 2-minute incisions of 2 cm, equidistant by 7 cm. The bands were sutured with 5-0 mononylon sutures in the tarsal plate and frontalis muscle, with the patient awake; the most adequate and anatomical position was evaluated.
Other techniques using suture wires with mononylon, polypropylene yarns17,18, deep temporal fascia19, and orbicularis muscle in the form of a wing, as described by Freitas and Sperli in 200920, were also described. Friedhofer et al.21 published in 2012 a large-scale study with 112 patients with severe ptosis who were treated with a silicone device, known as an eyelid implant suspensor. This apparatus consists of two rods connected to a plate with equally spaced holes to pass the attachment sutures.
They obtained an excellent result in 68.75% of the cases and good result in 26.79%. However, despite the high success rates, some complications related to the implant, such as cutaneous ulcerations, partial extrusion, and infection, occurred. Another study published by the same group22 showed the effectiveness of the implant suspensor in patients with blepharophimosis syndrome, both in adults and children, with minimal morbidity and optimal results.
Ramirez and Peña, in 200423, described a series of cases of severe congenital ptosis treated with transposition of a flap of the innervated frontalis muscle with good functional and cosmetic results and low complication rate. This technique was initially described by Fergus in 190124, followed by Song and Song in 198225, and Zhou and Chang in 198826.
Other authors described the effectiveness of this technique27,28 with minimal morbidity and good results. Zou et al.29 published in 2013 a histological analysis of the frontalis muscle flap in experimental models of pigs. They observed under scanning electron microscopy the viability of the muscle flap 6 and 12 months after its preparation and showed that this technique was applicable in severe cases.
CONCLUSION
Palpebral ptosis is a disease commonly found in clinical practice and requires the surgeon to have a comprehensive anatomic and functional knowledge of the delicate structure of the eyelid. In this study, 14 patients (21 eyelids) underwent surgery. The acquired form is the most common in Brazil, with the involutional form being the most common, as the study showed. This type of ptosis, typical of elderly patients, is caused by disinsertion of the aponeurosis of the tarsal plaque or its weakening.
With respect to the repair technique applied, frontalis suspension was performed in 9 eyelids; reinsertion of the aponeurosis in the tarsal plate, in 6 eyelids; shortening with reintegration in the tarsal plate, in 5 eyelids; and plication of the aponeurosis at a ratio of 4:1, in only 1 case. The complication rate was low, with asymmetries being the most difficult to treat.
Therefore, a good evaluation of patients with eyelid ptosis becomes mandatory, as well as the choice of the surgical repair technique to be used to obtain the best aesthetic-functional outcome.
COLLABORATIONS
|
RC |
Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents. |
|
CJB |
Writing the manuscript or critical review of its contents. |
|
FSG |
Statistical analyses. |
REFERENCES
1. Reid RR, Said HK, Yu M, Haines GK 3rd, Few JW. Revisiting upper eyelid anatomy: introduction of septal extension. Plast Reconstr Surg. 2006;117(1):65-70. DOI: http://dx.doi.org/10.1097/01.prs.0000194923.99879.90
2. Katowitz WR, Katowitz JA. Congenital and developmental eyelid abnormalities. Plast Reconstr Surg. 2009;124(1 Suppl):93e-105e. DOI: http://dx.doi.org/10.1097/PRS.0b013e3181aa2a9b
3. Litwin AS, Patel B, McNab AA, McCann JD, Leatherbarrow B, Malhorta R. Blepharoptosis surgery in patients with myasthenia gravis. Br J Ophthalmol. 2015;99(7):899-902. DOI: http://dx.doi.org/10.1136/bjophthalmol-2014-306335
4. Srinath N, Balaji R, Basha MS. Ptosis correction: a challenge following complex orbital injuries. J Maxillofac Oral Surg. 2012;11(2):195-9. DOI: http://dx.doi.org/10.1007/s12663-011-0300-3
5. Parsa DF, Wolff DR, Parsa NN, Elahi aE E. Upper eyelid ptosis repair after cataract extration and importance of Hering's test. Plast Reconstr Surg. 2001;108(6):1527-36. DOI: http://dx.doi.org/10.1097/00006534-200111000-00014
6. Chang S, Lehrman C, Itami K, Rohrich RJ. A systematic review of comparison of upper eyelid involutional ptosis repair techniques: efficacy and complication rates. Plast Reconstr Surg. 2012;129(1):149-57. DOI: http://dx.doi.org/10.1097/PRS.0b013e318230a1c7
7. Rolim JDAL, Rovaris DA, Chia CY. Fenômeno de marcus Gunn recidivado: relato de caso e revisão bibliográfica. Rev Bras Cir Plást. 2014;29(4):578-81.
8. Fasanella RM, Servat J. Levator resction for minimal ptosis: another simplified operation. Arch Ophtalmol. 1961;65:493-6.
9. Saito FL, Gemperli R, Hiraki PY, Ferreira MC. Cirurgia da ptose palpebral: análise de dois tipos de procedimentos cirúrgicos. Rev Bras Cir Plást. 2010;25(1):11-7.
10. Alves DG. Plicatura e reinserção da aponeurose do músculo levantador da pálpebra superior com sutura contínua na correção cirúrgica da ptose palpebral leve e moderada-experiência pessoal. Rev Bras Cir Plást. 2014;29(1):39-43.
11. Crawford JS. Repair of ptosis using frontalis muscle and fascia lata. Trans Am Acad Ophthalmol Otolaryngol. 1956;60(5):672-8.
12. Krohn-Hansen D, Haaskjold E, Nicolaissen B. Suspension surgery with autogenous fascia lata via a less invasive modification of the Crawford method on 85 patients with congenital severe eyelid ptosis. J Plast Surg Hand Surg. 2015;49(4):214-9. DOI: http://dx.doi.org/10.3109/2000656X.2014.1001853
13. Yoon JS, Lee SY. Long-term functional and cosmetic outcomes after frontalis suspension using autogenous fascia lata for pediatric congenital ptosis. Ophthalmology. 2009;116(7):1405-14. DOI: http://dx.doi.org/10.1016/j.ophtha.2009.01.040
14. Batista KT, Araújo HJ. Correção da blefaroptose na oftalmoplegia crônica progressiva. Rev Bras Cir Plást. 2009;24(1):1-5.
15. Bilgin LK, Yeniad B. The Long-Term Results of Frontalis Suspension Using Autogenous Fascia Lata in Children with Congenital Ptosis under 3 Years Old. Plast Surg Int. 2010;2010:609462. PMID: 22567230
16. Leibovitch I, Leibovitch L, Dray JP. Long term results of frontalis suspension using autogenous fascia lata for congenital ptosis in children under 3 years of age. Am J Ophthalmol. 2003;136(5):866-71. PMID: 14597038 DOI: http://dx.doi.org/10.1016/S0002-9394(03)00466-5
17. Cagatay HH, Ekinci M, Apil A, Arslan B, Pamukcu C, Oba ME, et al. The use of polypropylene suture as a frontalis suspension material in all age groups of ptosis patients. J Invest Surg. 2014;27(4):240-4. DOI: http://dx.doi.org/10.3109/08941939.2014.892187
18. Bouazza M, Eibelhadji M, Mchachi A, Benhmidoune L, Amraoui A. Treatment of congenital ptosis by frontalis suspension with monofilament polypropylene suture: results of study of 21 cases. J Fr Ophtalmol. 2014;37(7):520-5. DOI: http://dx.doi.org/10.1016/j.jfo.2014.01.014
19. Tellioglu AT, Saray A, Ergin A. Frontalis sling operation with deep temporal fascial graft in blepharoptosis repair. Plast Reconstr Surg. 2002;109(1):243-8. DOI: http://dx.doi.org/10.1097/00006534-200201000-00038
20. Freitas JOG, Sperli A. Tratamento da ptose palpebral com emprego de retalho em asa do músculo orbicular. Rev Bras Cir Plást. 2009;24(4):552-5.
21. Friedhofer H, Nigro MVAS, Sturtz G, Ferreira MC. Correction of severe ptosis with silicone implant suspensor: 22 years of experience. Plast Reconstr Surg. 2012;129(3):453e-460e. DOI: http://dx.doi.org/10.1097/PRS.0b013e318267d822
22. Friedhofer H, Nigro MV, Filho AC, Ferreira MC. Correction of blefarophimosis with silicone implant suspensor. Plast Reconstr Surg. 2006;117(5):1428-34. DOI: http://dx.doi.org/10.1097/01.prs.0000207472.55066.8d
23. Ramirez OM, Peña G. Frontalis muscle advancement: a dynamics structure for the treatment of severe congenital eyelid ptosis. Plast Reconstr Surg. 2004;113(6):1841-9. DOI: http://dx.doi.org/10.1097/01.PRS.0000117664.07831.48
24. Fergus AF. An Easy Operation for Congenital Ptosis. Br J Med;1901;1(2100):762. DOI: http://dx.doi.org/10.1136/bmj.1.2100.762
25. Song R, Song Y. Treatment of blepharoptosis. Direct transplantation of the frontalis muscle to the upper eyelid. Clin Plast Surg. 1982;9(1):45-8.
26. Zhou LY, Chang TS. Frontalis myofascial flap from eyebrow region for the correction of ptosis of the upper eyelid. Eur J Plast Surg. 1988;11(2):73-8. DOI: http://dx.doi.org/10.1007/BF00299215
27. Medel R, Vasquez L, Wolley Dod C. Early frontalis flap surgery as first option to correct congenital ptosis with poor levator function. Orbit. 2014;33(3):164-8. DOI: http://dx.doi.org/10.3109/01676830.2014.881396
28. Zhong M, Jin R, Li Q, Duan Y, Huang L, Yu D. Frontalis muscle flap advancement for correction of severe ptosis under general anesthesis: modified surgical design with 162 cases in China. Aesthetic Plast Surg. 2014;38(3):503-9. DOI: http://dx.doi.org/10.1007/s00266-014-0297-3
29. Zou C, Wang JQ, Guo X, Yu H, Li XQ, Li WY, et al. Long term histopathologic study of the frontalis muscle flap after frontalis suspension for severe ptosis repair. Ophthal Plast Reconstr Surg. 2013;29(6):486-91. DOI: http://dx.doi.org/10.1097/IOP.0b013e3182a64de7
1. Sociedade Brasileira de Cirurgia Plástica, São
Paulo, SP, Brazil.
2. Hospital Municipal Barata Ribeiro, Rio de
Janeiro, RJ, Brazil.
3. Universidade do Estado do Rio de Janeiro, Rio
de Janeiro, RJ, Brazil.
Corresponding author: Rodolfo Chedid
Avenida Armando Lombardi, 1000, sala 136, bloco 02 - Barra da Tijuca
Rio de
Janeiro, RJ, Brazil Zip Code 22640-000
E-mail: rodolfochedid@gmail.com
Article received: December 04, 2017.
Article accepted: May 17, 2018.
Conflicts of interest: none.

























 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter