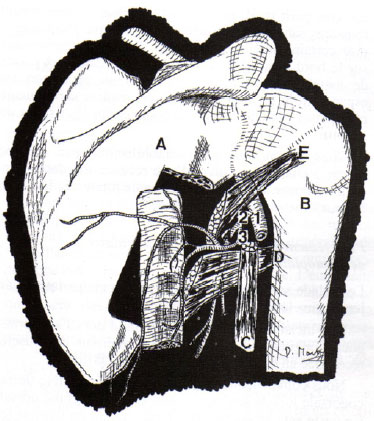
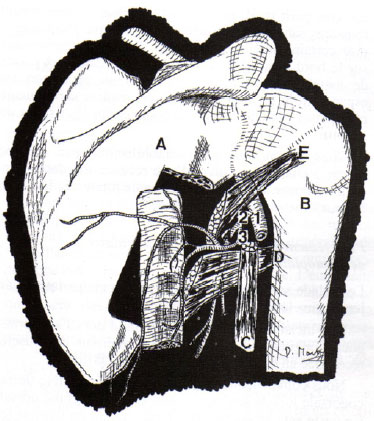
 Figure 2.
Figure 2. Drawing showing the layout of flap elevation and vascularization.
A: Scapula;
B: Humerus;
C: Long head of the triceps;
D: Teres major muscle;
E: Teres minor muscle; 1: Axillary artery; 2: Subscapular artery; 3: Circumflex scapular artery; 4: Thoracodorsal artery.
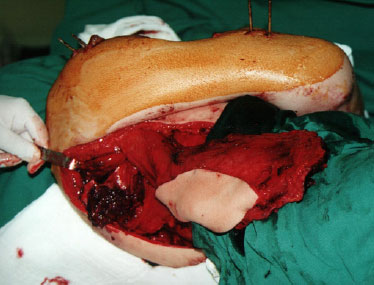
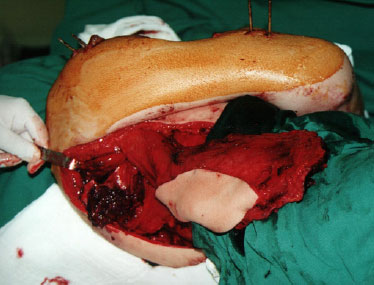 Figure 3.
Figure 3. Intraoperative aspect, patient in left lateral decubitus. Note the lateral border of the right scapula already elevated, along with the latissimus dorsi muscle and overlying skin.
The patient had an excellent postoperative course, and presented at the 2-month follow-up with bone consolidation and initiation of elbow flexion (Figure 4).
 Figure 4.
Figure 4. 2-month postoperative aspect showing the reconstructed area and the patient initiating flexion of the elbow.
A bone flap from the lateral border of the scapula presents great advantages in the reconstruction of the humerus compared to that from other bone sources commonly used for this purpose, such as the iliac flap and the fibular flap:
- Proximity to the receiving area: the flap can be transposed in a pedicled manner, without the need of microsurgical technique;
- Safety: the subscapular system is, without dispute, the most widely used for flap preparation and implementation, with large published studies showing its safety and limited anatomical variation;
- Diversity of possible elevations: no other flap area offers greater diversity of possible flaps, starting from a scapular and parascapular cutaneous flap, through a flap of the serratus anterior muscle and the muscular, musculocutaneous, and osteomyocutaneous flap (with the tenth rib) of the latissimus dorsi, up to the association of these flaps with the lateral scapular border flap;
- Quality of bone transferred: the lateral border of the scapula is a richly vascularized cancellous bone, making its use for reconstruction superior to that of the rib;
- The presence of a long pedicle: this provides a wide arc of rotation to this flap and greater safety and ease for free transfers.
CONCLUSIONConsidering the use of a flap from the lateral scapula border described in this report, together with numerous anatomical and clinical studies already published, we conclude that the osteomyocutaneous scapular flap is an excellent option in cases of large tissue loss in the upper limb. It can safely be raised pedically, as demonstrated, and can also be associated with transposition of the latissimus dorsi and overlying skin. The pedicle is easily dissected and visualized; moreover, in addition to the scapula, the rib can be used as a donor bone source. This bone flap, in addition to a flap from the iliac crest and fibula, is safely and commonly used in bone reconstruction in general, and especially in the upper limb.
COLLABORATIONSHRPF Analysis and/or interpretation of data; statistical analyses; final approval of the manuscript; conception and design of the study; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
JAF Writing the manuscript or critical review of its contents; completion of surgeries and/or experiments.
JAF Completion of surgeries and/or experiments.
GM Completion of surgeries and/or experiments.
REFERENCES1. Téot L, Bosse JP, Moufarrege R, Papillon J, Beauregard G. The scapular crest pedicled bone graft. Int J Microsurg. 1981;3:257-62.
2. dos Santos LF. The vascular anatomy and dissection of the free scapular flap. Plast Reconstr Surg. 1984;73(4):599-604. PMID: 6709742 DOI:
http://dx.doi.org/10.1097/00006534-198404000-000143. Swartz WM, Banis JC, Newton ED, Ramasastry SS, Jones NF, Acland R. The osteocutaneous scapular flap for mandibular and maxillary reconstruction. Plast Reconstr Surg. 1986;77(4):530-45. PMID: 3952209 DOI:
http://dx.doi.org/10.1097/00006534-198604000-000034. Deraemaecker R, Thienen CV, Lejour M, Dor P. The serratus anterior scapular free flap: a new osteomuscular unit for reconstruction after radical head and neck surgery. In Proceedings of the Second International Conference on Head and Neck Cancer; 1988 Jul 31-Aug 5; Boston, MA, USA.
5. Coleman JJ 3rd, Sultan MR. The bipedicled osteocutaneous scapula flap: a new subscapular system free flap. Plast Reconstr Surg. 1991;87(4):682-92. PMID: 2008466 DOI:
http://dx.doi.org/10.1097/00006534-199104000-000136. Frodel JL Jr, Funk GF, Capper DT, Fridrich KL, Blumer JR, Haller JR, et al. Osseointegrated implants: a comparative study of bone thickness in four vascularized bone flaps. Plast Reconstr Surg. 1993;92(3):449-55. DOI:
http://dx.doi.org/10.1097/00006534-199309000-000107. Funk GF. Scapular and parascapular free flaps. Facial Plast Surg. 1996;12(1):57-63. DOI:
http://dx.doi.org/10.1055/s-2008-10644941. Universidade Estadual Paulista Campus de Botucatu, Botucatu, SP, Brazil
2. Faculdade de Medicina de Fernandópolis, Unicastelo, Fernandópolis, SP, Brazil
3. Colégio Brasileiro de Cirurgiões, Rio de Janeiro, RJ, Brazil
4. Hospital das Clínicas de Fernandópolis, Fernandópolis, SP, Brazil
5. Sociedade Brasileira de Ortopedia, São Paulo, SP, Brazil
Institution: Hospital das Clínicas de Fernandópolis, Fernandópolis, SP, Brazil.
*Corresponding author:Humberto Regis de Paula Faleiros
Avenida Amadeu Bizelli, 979
Centro - Fernandópolis, SP, Brazil - Zip Code 15600-000
E-mail:
betofaleiros@yahoo.comArticle received: February 13, 2012.
Article accepted: January 26, 2018.
Conflicts of interest: none.