ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Reverse breast lift for treatment of congenital symmastia
Lifting reverso do seio mamário para tratamento de simastia congênita
ABSTRACT
INTRODUCTION: Breasts are associated with a feeling of beauty, self-esteem, and female sexuality. Symmastia is a condition, characterized by the confluence of both breasts in the pre-sternal region. The author demonstrates a surgical technique for correction of congenital symmastia.
METHODS: This is the case report of a young patient with previous history of breast hypertrophy and symmastia. She had previously undergone two mammoplasties and one liposuction of the breast, without correction of the symmastia . The author performed resection of the excess tissue in the breast and a reverse lifting of this region, with an upper abdominal advancement flap.
RESULTS: There was complete resolution of the symmastia.
CONCLUSION: The treatment performed by the author is a safe surgical alternative for the treatment of symmastia.
Keywords:
Breast; Mammoplasty; Breast implantation; Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A mama está diretamente relacionada com a beleza, autoestima e sexualidade feminina. A simastia é uma alteração inestética mamária, caracterizada pela união das duas mamas na região pré-esternal. O autor demonstra uma técnica cirúrgica para correção de simastia congênita.
MÉTODOS: O trabalho relata o caso de uma paciente jovem com história prévia de hipertrofia mamária e simastia, que realizara previamente duas mamoplastias e uma lipoaspiração no seio mamário, sem correção da simastia. O autor realizou a ressecção do excesso de tecido no seio mamário e um lifting reverso dessa região, associado com um retalho em avanço do abdome superior.
RESULTADOS: Houve completa resolução da simastia com o tratamento proposto.
CONCLUSÃO: O tratamento realizado pelo autor demonstrou ser mais uma alternativa cirúrgica segura no tratamento da simastia.
Palavras-chave:
Mama; Mamoplastia; Implante mamário; Procedimentos cirúrgicos reconstrutivos.
INTRODUCTION
Breasts are directly associated with a feeling of beauty, self-esteem and female sexuality1. Symmastia is an unaesthetic breast condition, characterized by the confluence of both breasts in the pre-sternal region. First described by Spence et al.2, in 1984, symmastia may be classified as congenital, or acquired, the latter caused by trauma, burns and infection, or following breast augmentation3.
The etiology of congenital symmastia is unknown. On physical examination, a bridge joining the two breasts in the pre-sternal region is observed, caused by accumulation of the skin, fat, and gland, associated with tissue laxity in this region. Acquired symmastia after breast augmentation is classified as monocapsular, when there is a connection between the capsules in the pre-sternal region, and bicapsular, when there is no communication between the capsules4,5.
OBJECTIVE
The author reports the treatment of a case of congenital symmastia, in which resection of the loose intermammary tissue, and a reverse lifting of the area was performed with an upper abdominal advancement flap. This provided a better anchor to the breasts and maintained the scar in the intermammary sulcus.
METHODS
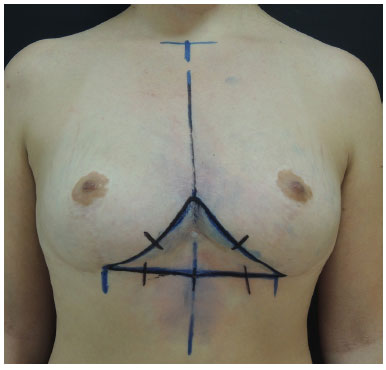
A female patient, aged 28 years, without co morbidities, presented with a history of breast hypertrophy associated with symmastia. She underwent two previous mammoplasties, at 18 and 23 years of age, and was satisfied with the volume of her breasts, but not with the persistent symmastia (Figures 1 and 2). She underwent a liposuction with breast enlargement at 24 years, but the symmastia persisted.
 Figure 1.
Figure 1. Pre-operative view.
 Figure 2.
Figure 2. Pre-operative period - left oblique view.
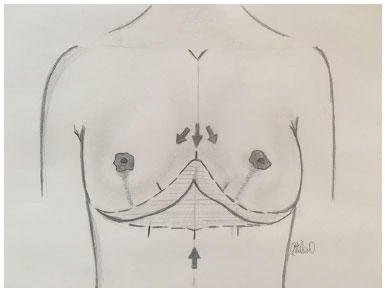
We resected the excess tissue within the breasts, followed by a reverse lifting of the area, bringing the structures downwards, in an inferior lateral vectorial direction (Figures 3 to 5), thus lateralizing the mammary cone. We fixed the new breast at three points, with the fascia fixed to the sternal periosteum. A flap of the upper abdomen with a triangular marking was advanced, which could be modified to a lozenge if there was greater abdominal flaccidity.
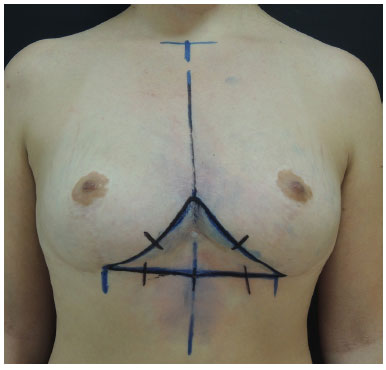 Figure 3.
Figure 3. Marking of resection.
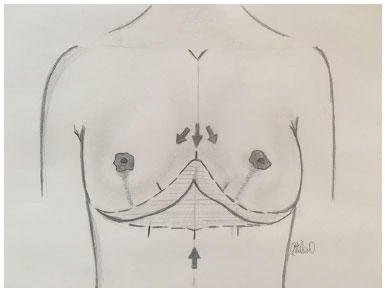 Figure 4.
Figure 4. Traction of the breast in the inferolateral direction.
 Figure 5.
Figure 5. Extended resection of the marking for better compensation.
We did not change the shape of the areolas as desired by the patient. We did not use any type of breast pocket or breast brace to deviate the breasts, except the conventional postoperative bra. The surgery was performed by the author in the Beneficent Association - University Hospital in Marília, SP, in 2016.
RESULTS
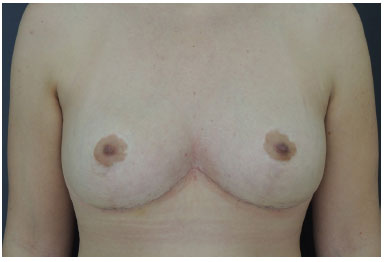
There were no complications in the postoperative period. The shape of the breasts was aesthetic and satisfactory, with resolution of symmastia (Figures 6 and 7).
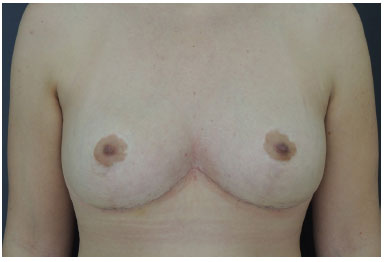 Figure 6.
Figure 6. 3 months post-operative period, frontal view.
 Figure 7.
Figure 7. Post-operative period - left oblique view.
DISCUSSION
The treatment of congenital symmastia is poorly described in the literature and the condition is difficult to treat, as described by Spence in 19842, who used a "V-Y" flap. Mc Kissock6 described an M-shaped flap, in contrast with Salgado and Mardini7 who, in 2014, treated a case using a periareolar approach, associated with liposuction. On the other hand, the treatment of acquired symmastia after breast implantation has been demonstrated to be simpler by Spear et al.8 and Parsa et al.4,5.
The reverse lifting of the breast with an upper abdominal advancement flap is another surgical option for the treatment of this difficult aesthetic breast condition. It is easy to execute, is safe, and preserves the scar in the intermammary sulcus. We believe in its effectiveness both when used alone, without the need to reduce the breast volume, and in association with reduction mammoplasties.
CONCLUSION
The treatment proposed by the author is just a first step and another safe therapeutic option for mammoplasties.
COLLABORATIONS
GDJ Conception and design of the study; writing the manuscript or critical review of its contents; final approval of the manuscript.
FCD Critical review of its contents; completion of surgeries and/or experiments.
REFERENCES
1. Guimarães PAMP, Sabino Neto M, Abla LEF, Veiga DF, Lage FC, Ferreira LM. Sexualidade após mamoplastia de aumento. Rev Bras Cir Plást. 2015;30(4):552-9.
2. Spence RJ, Feldman JJ, Ryan JJ. Symmastia: the problem of medial confluence of the breasts. Plast Reconstr Surg. 1984;73(2):261-6. DOI: http://dx.doi.org/10.1097/00006534-198402000-00020
3. Sillesen NH, Hölmich LR, Siersen HE, Bonde C. Congenital symmastia revisited. J Plast Reconstr Aesthet Surg. 2012;65(12):1607-13. PMID: 23026472 DOI: http://dx.doi.org/10.1016/j.bjps.2012.08.008
4. Parsa FD, Koehler SD, Parsa AA, Murariu D, Daher P. Symmastia after breast augmentation. Plast Reconstr Surg. 2011;127(3):63e-65e. PMID: 21364388 DOI: http://dx.doi.org/10.1097/PRS.0b013e31820635b5
5. Parsa FD, Parsa AA, Koehler SM, Daniel M. Surgical correction of symmastia. Plast Reconstr Surg. 2010;125(5):1577-9. PMID: 20440189 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181d513f0
6. McKissock PK. Symmastia: The problem of confluence of the breast [Discussion]. Plast Reconst Surg. 1984;73(2):267. DOI: http://dx.doi.org/10.1097/00006534-198402000-00021
7. Salgado CJ, Mardini S. Periareolar approach for the correction of congenital symmastia. Plast Reconstr Surg. 2004;113(3):992-4. PMID: 15108896 DOI: http://dx.doi.org/10.1097/01.PRS.0000105072.14373.0E
8. Spear SL, Dayan JH, Bogue D, Clemens MW, Newman M, Teitelbaum S, et al. The "neosubpectoral" pocket for the correction of symmastia. Plast Reconstr Surg. 2009;124(3):695-703. PMID: 19363454 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181a8c89d
1. Hospital Niterói D'or, Niterói, RJ, Brazil
2. Associação Beneficente - Hospital Universitário de Marília, SP, Brazil
3. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital Niterói D'or, Niterói, RJ, Brazil.
Corresponding author:
Getúlio Duarte Junior
Rua Sete de Setembro, 119 - Boa Vista
Marília, SP, Brazil Zip Code 17501-560
E-mail: drgetulioduarte@hotmail.com
Article received: February 2, 2017.
Article accepted: April 23, 2017.
Conflicts of interest: none.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license