ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Digital computerized analysis of auricle measures in otoplasties
Avaliação computadorizada digital das medidas auriculares em otoplastias
ABSTRACT
INTRODUCTION: Recently a number of studies have been published on quantitative measures mainly for the prominence of digital imaging processing, which is a non-invasive and precisely procedure. This study assessed measures in anterior view before and after surgery of patients who underwent otoplasty using computer analysis of digital images.
METHODS: A retrospective study was performed on a consecutive series from February 2014 to April 2015. Measures were done in the upper third, middle and bottom of the ears.
RESULTS: Of 103 patients, 47 were men and 56 women. We used the technique of weakening the cartilage by making multiple posterior islands associated with non-absorbable suture in 56 patients, an isolated conchal cartilage resection in 1 patient and combination of all techniques in 47 patients. The result of auricle measure in frontal viewing at previous measured points performed using computer analysis showed a significant mean reduction in the third month after surgery.
CONCLUSION: Digital image assessment can estimate auricle measure with high repeatability, corroborating with the use of digital images in noninvasive procedures as less expensive and highly available option in clinical practice. The computed anthropometric analysis of digital images in direct frontal view using images taken before and after surgery is an alternative method for traditional measurements to evaluate results in otoplasties.
Keywords:
Ear; Otoplasty; Proeminent ear; Mesuraments.
RESUMO
INTRODUÇÃO: Nos últimos anos, a literatura vem se enriquecendo de medidas quantitativas, principalmente pelo advento do processamento digital de imagens, procedimento não invasivo e bastante preciso. O objetivo do presente estudo é avaliar as medidas em visão anterior no pré e pós-operatório de pacientes submetidos à otoplastia através de análise computadorizada de fotografias digitais.
MÉTODOS: O estudo retrospectivo foi realizado numa série consecutiva de casos no período de fevereiro de 2014 a abril de 2015. Foram realizadas medidas no terço superior, médio e inferior das orelhas.
RESULTADOS: Do total de 103 pacientes, 47 eram do sexo masculino e 56 do sexo feminino. A técnica de enfraquecimento do pavilhão, pela confecção de ilhas cartilaginosas múltiplas, associada à sutura com fio inabsorvível incolor, foi utilizada em 56 pacientes; a ressecção de cartilagem conchal isolada em um paciente e a combinação das técnicas anteriormente descritas em 47. O resultado da medida auricular em visão frontal nos pontos previamente descritos, realizada através da análise computadorizada, demonstrou uma redução média importante no terceiro mês de pós-operatório.
CONCLUSÃO: No presente estudo, demonstrou-se que a avaliação fotográfica digital pode estimar medidas da orelha com alta reprodutibilidade, corroborando o emprego da fotografia digital na estimativa não invasiva dessas variáveis, como opção de custo reduzido e alta disponibilidade na prática clínica. Em conclusão, a análise antropométrica computadorizada em visão frontal, utilizando fotografias digitais pré e pós-operatórias é uma alternativa aos métodos de medidas tradicionais utilizados para avaliação de resultados em otoplastias.
Palavras-chave:
Orelha; Otoplastia; Orelha proeminente; Medidas.
INTRODUCTION
The external ear exists only in mammals and its function is to direct vibrations to the middle and inner ear. In this study the term external ear will be use to simplify the term ear. Some of the structures, such as the external ear muscles remain trace in humans, but they are active in many other animals.
Normal ear anatomy is widely known in previous studies of anthropometry. The largest ear width is 63.5 mm in men and 59 mm in women, the average ear width is 35.5 mm in men and 32.5 mm in women1.
Another important parameter is the relationship between helix and antihelix. The helix should project 2 to 5 mm more laterally than the antihelix1,2 in frontal view (Figure 1).
 Figure 1.
Figure 1. Clinically normal ear, and protuberante helix many milimeters to more than antihelix and superior crus.
The measurement of ear projection from the scalp allows a proper evaluation of results, and it is key in the diagnosis, planning and implementation of corrective otoplasty. Despite the minor variations, on average, the upper third of the helix distance 1 to 1.2 cm from the scalp, the middle third, 1.6 to 1.8 cm, and the lobe are located 2.2 cm 2 the region from the mastoid region1-2.
The external ear has some parameters considered ideally aesthetically. The auriculocephalic angle formed by the intersection of a line parallel and tangent to the temporal bone and the ear must be 25 to 30 degrees. In prominent ear that angle exceeds 40-45 degrees. The concha-scaphoid angle formed by the intersection of a line parallel to escafa and another parallel to the rear surface of the ear shell, is ideal when close to 90 degrees. When absent or weak (> 90 degrees), the escaphoconchal angle contributes to the formation of prominent ear2.
The ear reaches 85% of development at 3 years and it is fully developed at 7-8 years of age. As we get older, more rigid and calcified is the auricular cartilage. This evolution can affect the technique to be used in otoplasties3.
Prominent ear is the most common congenital deformity in the head and neck region. The estimated incidence in white population is 5%. In about 60% of cases it can be diagnosed at birth. The remaining cases will be diagnosed in early childhood4.
The exact etiology of ear prominence is unclear, and it may be related to postural attitudes of newborns, muscular hypotonia frames, structural collagen changes, genetic diseases and familial incidence with genetic pattern5.
It can be inherited in an autosomal dominant manner through the combination of two faults; or less frequent, with only one of them: 1) underdevelopment or absence of scaphoid- conchal angle; 2) ear shell cartilage hypertrophy6.
Strong feelings about this deformity are rooted in different cultures. In the east, protruding ears means luck and its correction is not a very popular procedure. However, in the West, prominent ears can have pejorative connotation and it may cause embarrassing and social isolation7. In this context, otoplasty is purely aesthetic, and indicate widely accepted in children, adolescents and adults5.
The first description of otoplasty was performed by Dieffenbach in 1845 with excision of skin and conchal-mastoid fixation, joining the shell at the perichondrium Galea, in a case of ear trauma8. Over 150 techniques have been described in the last 100 years to correct protruding ears6. Since then, otoplasty has undergone several changes and additions techniques, with different tactical variations. Patient satisfaction is emphasized with frequency, regardless of the technique used9,10,11.
Most studies on ear projection is quantitative, through direct later measured using rules or compass1,4,5.
In recent years, the literature has been enriched quantitative measures, mainly by the advent of digital imaging, non-invasive procedure and fairly accurate12,13, 14. This technique enables refined quantitative analysis of parameters that may have surgical importance12.
However, this type of research has not been carried out, and only few studies exist related to blepharoplasty and cleft lip and palate, therefore motivating this research13,14.
OBJECTIVE
This study assessed the measures in anterior view in the pre- and postoperative patients undergoing otoplasty through computer analysis of digital photographs.
METHODS
The retrospective study was performed on a consecutive series of cases from February 2014 to April 2015, complying with all the principles of the Helsinki declaration.
Patients included in the study were all those undergoing otoplasty, unilateral or bilateral, who were under sedation and received local anesthesia. The initial approach was common skin through posterior incision spindle. The technical option used was the weakening of upper third by making multiple cartilaginous islands, with or without resection of the ear cartilage15. This resection, when necessary, was made by marking with needle and dye, to the way Mustardé held in antihelix. All patients underwent surgery and they were followed-up by the same plastic surgeon.
Directed healing in all patients with crepe bandages, sterile gauze and cotton for 4 days. The use of ear brace was directed for 30 days for a minimum of 12 hours. The returns were performed at 7, 30, 60 and 90 days postoperatively.
The pictures were taken using a single digital camera (Samsung note 3, 13 megapixel resolution of 4128 x 3096 with digital stabilization), with standard distance and parallel millimeter ruler ear (Figure 2).
 Figure 2.
Figure 2. We performed measures in the superior, medium and inferior third of ears. The superior point goes over the triangle fossa, the medium, superior limit of the tragus and inferior over the antitragus.
Patients were evaluated and obtained their photographic record before surgery and at least 3 months postoperatively.
Measurements were performed in the upper third, middle and bottom of the ears. The top spot goes on the triangular fossa, between the apex of the propeller and the propeller branch; the middle, upper limit of the tragus and antitragus on the bottom (Figure 2).
Bilateral anthropometric ear measured at three points was performed using the described linear measurement software ImageJ software 1.37v®.
Age, sex, technique used, and complications were recorded.
The following postoperative parameters were evaluated: pain, paresthesias, hematoma, skin necrosis, wound dehiscence, hypertrophic scars and need for surgical revision (correction of secondary deformities or asymmetries in the subsequent 3-6 months).
RESULTS
Of the total 103 patients, 47 were male and 56 female.
The mean age was 25 years (7-71 years).
Bilateral otoplasty was performed in 101 and unilateral in 2 patients.
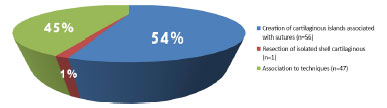
The pavilion weakening technique for the production of multiple cartilaginous islands accompanied by colorless suture with nonabsorbable suture was used in 56 patients, resection of isolated ear cartilage in 1 patient and the combination of the techniques described above in 47 (Figure 3).
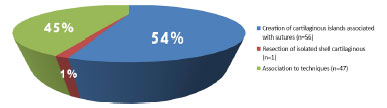 Figure 3.
Figure 3. Cartilage weaking technique of ear pavilion to create multiple cartilaginous islands followed by suture with uncolored unabsorbable wires were used in 56 patients, the resection of isolated shell cartilage in 1 patient and combination of techniques early described in 47 patients
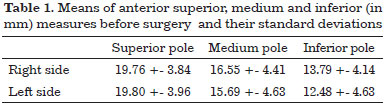
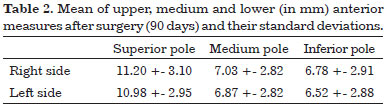
The result of previous ear measured in points described previously performed by computer analysis demonstrated a mean significant reduction in the third month postoperatively (Figure 4 and 5 and Tables 1 and 2). The reduction in upper, middle and lower measures were in the order of 44%, 57% and 50% respectively when compared to preoperative measurements.
Greater asymmetry than 3 mm preoperatively were found in 37% (n = 38) of patients, and reduced postoperative for 16% (n = 17). Of these, only 4 underwent surgical revision by their request and/or request own surgeon and patient consent. The average asymmetries in upper, middle and lower preoperative were respectively 2.84 mm, 3.17 mm and 2.75 mm. In the third month after surgery these measures were respectively 1.68 mm, 1.69 mm and 1.66 mm.
In the immediate postoperative period was reported by most discrete paresthesia (n = 90) and moderate to severe pain in a minority (n = 13) of patients.
Complications were recorded in 20 (19%) patients. Hematoma in shell removal site occurred in 1 patient and it was handled by puncturing with caliber needle and pressure dressing immediate after surgery. Skin necrosis minor was observed in 5 patients (4.8%) treated conservatively with dressings and satisfactory settlement in 2-3 weeks. Partial dehiscence of suture occurred in 8 (7.7%) patients without intervention. Hypertrophic scarring was observed in 2 (1.9%) patients. A total of 4 patients (3.88%) underwent new surgery approach to improve the aesthetic result and symmetry.
DISCUSSION
The otoplasty goals were well described by McDowell16: 1) Full Correction protrusion of the upper third of the ear; 2) the visibility of the helix beyond the antihelix in anteroposterior view; 3) outline the soft propeller and regular 4) prevention of distortion or decrease the depth of the retroauricular groove; 5) positioning the ear at the correct distance from the scalp and not too close; 6) bilateral symmetry, i.e., difference in the helix-mastoid distance between the two sides should not exceed 3mm.
Differently from Pitanguy and Rebello17, who described in 1961 the production of a single island of cartilage for the reconstruction of antihelix, parallel incisions in the cartilage, which formed islands that lie at the poles, and facilitate modeling and provide a bending point rounded, and more harmonious way. The technique we report applies the same principles of Barsky (1938) and McEvitt (1947)18-19. These islands can be made only in the upper third, if the deletion of antihelix is confined to the pavilion apex15. The sutures are a form of security and maintenance of the result20-21.
Resection of the ear cartilage allows for better accommodation of the shell mastoid without the need for any fixing, differently from Mustardé (1963) and Furnas (1968)20-21.
Several studies showed that the helix-mastoid distance is significantly reduced in the immediate postoperative period, followed by a slight increase in the first months of this measure, with a trend towards stabilization between 3-6 months4.
The popularization of digital photography also affects medical practice, promoting the documentation of cases, their evolution and use in scientific research. When digital images are obtained in the presence of a millimeter ruler, evaluation of parameters of interest becomes more objective, allowing measurements to be made which can be directly incorporated into the metric system14.
The distance between the pixels that make up a digital image can be easily estimated from image editors. This procedure known as first linear order as is widely used in research and clinical practice, for example, in radiological images12-14.
There are studies suggesting that digital photography system with computerized analysis is comparable and offers advantages compared to traditional measurement methods. This system provides a simple, standardized and quick method of evaluation of patients with important applications in electronic records, audit and investigation12.
Although traditional or posterior auricular measure is the most widely used in the researched articles, the method requires more time to collect measures in addition to not allow the surgeon or researcher perform measurements without the presence of the patient. In addition to anteroposterior view of the face and ear contour provides additional information regarding facial harmony as the ear is a defining feature of this unit.
A highlight is the low cost of digital photography, storage facility, possibility of reproduction, sending without loss of quality and direct analysis without the need for printing photos12-14.
In the present study, it was shown that digital photographic assessment can estimate pinna parameters with high reproducibility, corroborating with the use of digital photography in the noninvasive estimate of such variables, such as reduced cost and high availability option in clinical practice.
CONCLUSION
Computed anthropometric analysis in anterior view digital photos using pre and post-operative is an alternative method to replace traditional measures used to evaluate results in otoplasties.
COLLABORATIONS
GAMS Analysis and interpretation of the data; statistical analyses; final approval of the manuscript; planning and study design; completion of surgeries and/or experiments; writing the manuscript or critical review of its contents.
JCRRA Critical review of its contents.
REFERENCES
1. Bozkir MG, Karakaş P, Yavuz M, Dere F. Morphometry of the external ear in our adult population. Aesthetic Plast Surg. 2006;30(1):81-5. DOI: http://dx.doi.org/10.1007/s00266-005-6095-1
2. Hornos A. Correção de orelha de abano por técnica combinada: análise de resultados e alteração da qualidade de vida. Rev Bras Cir Plást. 2013;28(3):406-15
3. Ha RY, Trovato MJ. Plastic Surgery of the Ear. Sel Read Plast Surg. 2011;11(R3):1-52.
4. Secco LG, Ogata DY, Pagnoncelli BH, Ribeiro RD, Paccanaro RC, De Miranda RE, et al. Medida do grau de correção das orelhas proeminentes utilizando algoritmo de tratamento padronizado. Rev Bras Cir Plást. 2013;28(4):571-7.
5. Ungarelli LF. Eficácia do retalho adipofascial retroauricular em otoplastia. Rev Bras Cir Plást. 2012;27(2):249-59. DOI: http://dx.doi.org/10.1590/S1983-51752012000200014
6. Spira M. Otoplasty: what I do now--a 30-year perspective. Plast Reconstr Surg. 1999;104(3):834-40. DOI: http://dx.doi.org/10.1097/00006534-199909010-00038
7. Tan KH. Long-term survey of prominent ear surgery: a comparison of two methods. Br J Plast Surg. 1986;39(2):270-3. PMID: 3697576 DOI: http://dx.doi.org/10.1016/0007-1226(86)90100-1
8. Dieffenbach JE. Die Ohrbildung Otoplastik. In: Die Operative Chirurgie. Leipzig: F.A. Brockhause; 1848. p. 395-7.
9. Kelley P, Hollier L, Stal S. Otoplasty: evaluation, technique, and review. J Craniofac Surg. 2003;14(5):643-53. DOI: http://dx.doi.org/10.1097/00001665-200309000-00008
10. Janis JE, Rohrich RJ, Gutowski KA. Otoplasty. Plast Reconstr Surg. 2005;115(4):60e-72e. PMID: 15793433 DOI: http://dx.doi.org/10.1097/01.PRS.0000156218.93855.C9
11. Limandjaja GC, Breugem CC, Mink van der Molen AB, Kon M. Complications of otoplasty: a literature review. J Plast Reconstr Aesthet Surg. 2009;62(1):19-27. PMID: 18952516 DOI: http://dx.doi.org/10.1016/j.bjps.2008.06.043
12. Coombes AG, Sethi CS, Kirkpatrick WN, Waterhouse N, Kelly MH, Joshi N. A standardized digital photography system with computerized eyelid measurement analysis. Plast Reconstr Surg. 2007;120(3):647-56. DOI: http://dx.doi.org/10.1097/01.prs.0000270315.53241.10
13. Sabitha S, Veerabahu M, Vikraman B. Esthetic evaluation of the treated unilateral cleft lip using photographs and image analysis software: a retrospective study. J Maxillofac Oral Surg. 2011;10(3):225-9. DOI: http://dx.doi.org/10.1007/s12663-011-0238-5
14. Miot HA, Pivotto DR, Jorge EM, Mazeto GMFS. Avaliação de parâmetros métricos oculares pela fotografia digital da face: uso do diâmetro da íris como unidade de referência. Arq Bras Oftalmol. 2008;71(5):679-83. DOI: http://dx.doi.org/10.1590/S0004-27492008000500013
15. Schettino A, Mayor DS, Soto A, Franco D, Franco T. Tratamento de orelhas em abano sem sutura cartilaginosa: associação de técnicas. Rev Bras Cir Craniomaxilofac. 2010;13(1):18-22
16. McDowell AJ. Goals in otoplasty for protruding ears. Plast Reconstr Surg. 1968;41(1):17-27. PMID: 5639206 DOI: http://dx.doi.org/10.1097/00006534-196801000-00004
17. Pitanguy I, Rebello C. Orelhas em abano: considerações em torno do problema e sugestão de técnica pessoal. Rev Bras Cir. 1961;42(6):267-77.
18. Barsky AJ. Plastic Surgery. Philadelphia: WB Saunders; 1938. p. 178.
19. McEvitt WG. The problem of the protruding ear. Plast Reconstr Surg (1946). 1947;2(5):481-96. DOI: http://dx.doi.org/10.1097/00006534-194709000-00011
20. Mustardé JC. The correction of prominent ears using simple mattress sutures. Br J Plast Surg. 1963;16:170-8. PMID: 13936895 DOI: http://dx.doi.org/10.1016/S0007-1226(63)80100-9
21. Furnas DW. Otoplasty for prominent ears. Clin Plast Surg. 2002;29(2):273-88. DOI: http://dx.doi.org/10.1016/S0094-1298(01)00014-1
1. Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
2. Hospital Unimed, Belo Horizonte e Betim, MG, Brazil
3. Hospital Vera Cruz, Belo Horizonte, MG, Brazil
4. Instituto de Mastologia, Odontologia e Cirurgia Plástica, Belo Horizonte, MG, Brazil
5. Universidade Federal de Minas Gerais, Belo Horizonte, MG, Brazil
6. Faculdade de Medicina da Universidade de Itaúna, MG, Brazil
7. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
8. Instituto de Cirurgia Plástica Avançada, Belo Horizonte, MG, Brazil
Institution: Clínica privada, Belo Horizonte, MG, Brazil.
Corresponding author:
Gustavo Augusto Matos Saliba
Rua Esmeralda, 1705, apt. 603 - Prado
Belo Horizonte, MG, Brazil Zip Code 30411-191
E-mail: salibagustavo@yahoo.com.br
Article received: September 6, 2015.
Article accepted: January 4, 2017.
Conflicts of interest: none.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license