

Original Article - Year 2016 - Volume 31 -
A review of abdominoplasty technique with reduced dissection and fixation with Baroudi sutures
Revisão da técnica de abdominoplastia com dissecção reduzida e fixação com pontos de Baroudi
ABSTRACT
INTRODUCTION: A retrospective study was carried out on 500 abdominoplasties with lower pubic transverse incision combined with liposuction, performed from 2007 to 2014. In all cases, the dissection of the abdominal skin flap was restricted, with adhesion sutures applied throughout the dissected regions. The use of vacuum suction drains was also evaluated. In 33% of cases, these drains were not used, but no signs of seroma were detected, proving the efficacy of adhesion sutures.
METHODS: In all abdominoplasties, the access route was the lower transverse pubic region extended up to the level of the anterior superior iliac spines bilaterally, combined with liposuction in the adjacent regions. After the dissection, plication of the rectus muscles, and resection of excess skin, adhesion sutures were applied throughout the dissected regions.
RESULTS: The systematic use of adhesion sutures was efficient, without the need to use drains, given the absence of seroma in all cases.
CONCLUSION: In lower pubic transverse abdominoplasty, limited dissection of the cutaneous flap extended up to the xiphoid, combined with adhesion sutures and liposuction, avoided the use of vacuum drains; no seroma developed, and the results were good.
Keywords: Abdominoplasty; Liposuction; Tissue adherence; Suction drainage; Seroma; Surgical flaps.
RESUMO
INTRODUÇÃO: Um estudo retrospectivo foi realizado em 500 abdominoplastias tipo incisão transversal pubiana baixa, combinada com lipoaspiração de 2007 a 2014. Em todas, a dissecção do retalho cutâneo abdominal foi restrita, em que foram aplicados pontos de adesão em toda a extensão das regiões dissecadas. Foi ainda avaliado o uso ou não de drenos de sucção a vácuo. Em 33% dos casos não foram utilizados estes drenos e não foram também detectados sinais de seroma, comprovando a eficácia dos pontos de adesão.
MÉTODOS: Em todas as abdominoplastias a via de acesso foi da região pubiana transversal baixa estendida até o nível das espinhas ilíacas anterossuperiores bilateralmente, associada à lipoaspiração nas regiões dos flancos. Após a dissecção, plicatura dos músculos retos e ressecção dos excessos cutâneos, foram aplicados pontos de adesão em toda a extensão das regiões dissecadas.
RESULTADOS: A conduta com o uso sistemático dos pontos de adesão demonstrou ser eficaz, sem a necessidade do uso de drenos de qualquer natureza dada a inexistência de seroma em todos os casos operados.
CONCLUSÃO: Nas abdominoplastias tipo pubiana transversal baixa, a dissecção limitada do retalho cutâneo estendida até o apêndice xifoide, associada a pontos de adesão e lipoaspiração concomitante, tem dispensado o uso de drenos a vácuo, sem a existência de seroma, além de determinar resultados gratificantes.
Palavras-chave: Abdominoplastia; Lipoaspiração; Aderências teciduais; Drenagem por sucção; Seroma; Retalhos cirúrgicos.
The abdominal region exhibits aesthetic-functional changes throughout life, more commonly in women, due to pregnancy, weight fluctuation, sedentary lifestyle, inadequate nutrition, hormones, etc. Particularly during pregnancy, there is an increase in abdominal girth caused by stretching and flaccidity of the muscles of the pelvis, and of the rectus abdominis and oblique muscles, together with alterations in skin elasticity1.
Abdominoplasty is an effective and specific procedure for the improvement of body contour. The technique has been improved by combining limited dissection of the cutaneous flap, adhesion sutures, and liposuction in the same operation, thereby avoiding suture dehiscence, and complications such as skin necrosis, hematoma, and seroma.
Seroma is still a common problem, and may be difficult to treat without inconvenience to the surgeon and the patient. The appearance of seroma is the result of excess dead space in the dissected area, with accumulation of serosanguinous fluid forming a pocket with a pseudomembrane, despite the use of drains, compressive dressings, and an elastic strap.
This retrospective study was based on 501 abdominoplasties combined with liposuction performed between 2007 and 2014. Adhesion sutures2, limited cutaneous dissection3, and liposuction were combined in a single surgical procedure2-5. The surgical technique and the use or omission of vacuum suction drains for the prevention of seroma are discussed.
OBJECTIVE
The objective of this study was to correlate the use of drains and adhesion sutures with the development of a hematoma or seroma. The criteria for limited dissection of cutaneous abdominal flaps were also evaluated.
METHODS
Female patients predominated, and ages ranged from 24 to 75 years. Abdominoplasty was performed with limited dissection up to the margin of the aponeurosis of the rectus abdominis muscle; the use of adhesion sutures and the use or omission of vacuum suction drains were assessed.
Demographic data, dates of surgeries, postoperative complaints, and presence of seroma diagnosed by ultra-sound examination6,7 were recorded. The patients were distributed into two groups, all with limited cutaneous dissection up to the limits of the rectus muscles: adhesion sutures without drains were used in one group, and the other group used adhesion sutures with drains.
The patients were evaluated after the 4th postoperative day and then weekly. Any drains used were removed when the volume of drainage was less than 30 mL/day.
Surgical Technique
Skin marking was performed with the patient standing and without preanesthetic (Figure 1). With the patient in horizontal ventral decubitus position under general anesthesia with endotracheal intubation, local infiltration of flanks was performed with Ringer's lactate at 38°C with adrenaline 1:500,000 in the demarcated areas. Liposuction was performed with a 3 to 4 mm Mercedes cannula8. Next, the patient was positioned in dorsal decubitus position with prior cutaneous demarcation for lower pubic transverse abdominoplasty, extended up to the anterior superior iliac spines bilaterally.
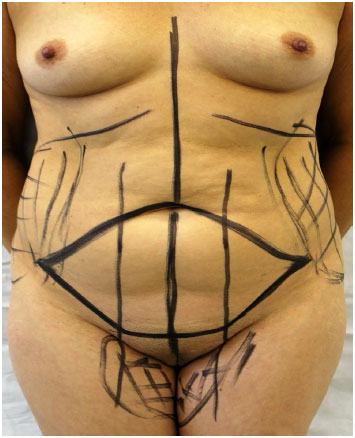
Figure 1. Cutaneous marking in a standing position, without pre-anesthetic.
The dissection of the skin plane from the pubis to the xiphoid was restricted to the area of plication of the aponeurosis along the outer edge of the rectus abdominis muscles, with dissection and release of the umbilical scar. This was followed by demarcation of the xipho-pubic line with methylene blue in the midline and plication of the aponeurosis of the rectus abdominis muscles with mononylon 2-0 (Figures 1 and 2). Suturing was performed in a single plane with isolated sutures.
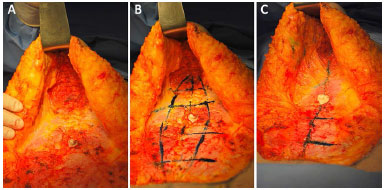
Figure 2. A: Dissection of the skin plane from the pubis to the xiphoid. B: demarcation of the xipho-pubic line. C: Plication with mononylon 2-0.
Then, with the patient in a semiflexed position, caudal traction on the abdominal flap was used to assess adequacy of dissection and whether the umbilicus reached or exceeded the level of the pubic region without skin folds or sagging. Resection of the excess skin and subcutaneous tissue was performed, followed by release and eversion of the cutaneous flap and application of adhesion sutures according to the described technique2-9.
The isolated adhesion sutures were used to secure the cutaneous flap in the aponeurosis of the rectus abdominis muscle with Vicryl 3-0, placed at intervals of 4 cm in lines and columns from the xiphoid to the pubic region bilaterally (Figure 3). Umbilicoplasty was performed according to the star technique10, in which the umbilical cutaneous stump has the form of a triangle and is fixed in the aponeurosis.
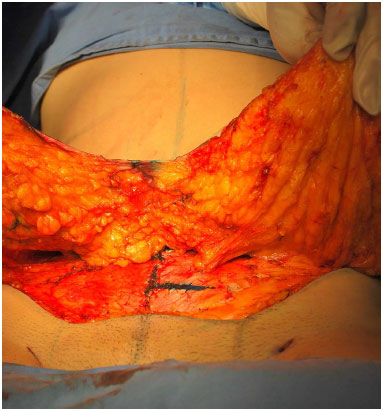
Figure 3. Cutaneous flap in the aponeurosis of the rectus abdominis muscle with Vicryl 3-0 suture placed equidistant at 4 cm intervals.
An incision is then made in the descent skin flap, with fixation in the aponeurosis, allowing the suture to remain in the inner part of the umbilical scar, avoiding its exposure. The central point of the flap is fixed in the midline of the pubis, and excess skin is resected5.
Sutures in planes follow all strata of the skin, including Scarpa's fascia. The vacuum drain, when used, is removed when the volume is less than 30 mL/day (Figure 4). Dressing is performed with porous adhesive on the suture line, and cotton wool and an elastic strap cover the entire area from the xiphoid to the middle third of the thighs.
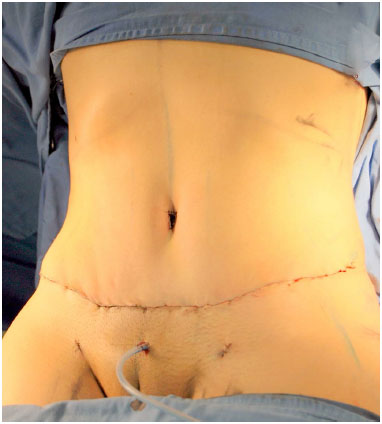
Figure 4. Vacuum drain with volume lower than 30 mL/day.
RESULTS
The patients were grouped by the year in which they underwent surgery, with reduced dissection of the cutaneous flap3, flap attachment2, and liposuction, and with or without the use of drains. All surgeries were performed by the same team at the Hospital Nipo-Brasileiro, in São Paulo, SP (Figures 5 to 8).
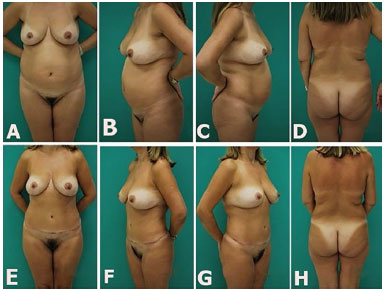
Figure 5. Abdominoplasty - (A, B, C, and D) preoperatively; (E, F, G, and H) postoperatively.
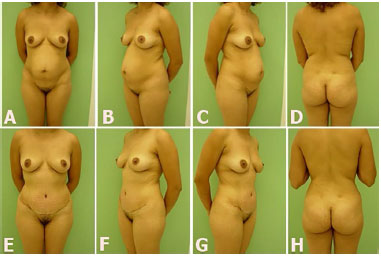
Figure 6. C.L., 30 years old, abdominoplasty and liposuction. (A, B, C, and D) preoperatively; (E, F, G, and H) 14 months postoperatively.
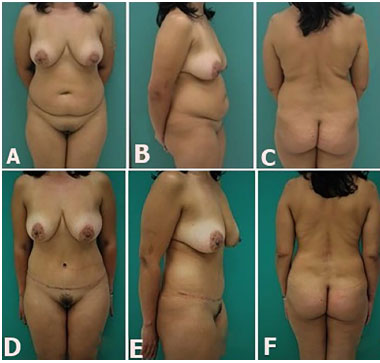
Figure 7. M.S., 38 years old, abdominoplasty and liposuction. (A, B, and C) preoperatively; (D, E, and F) 11 months postoperatively.
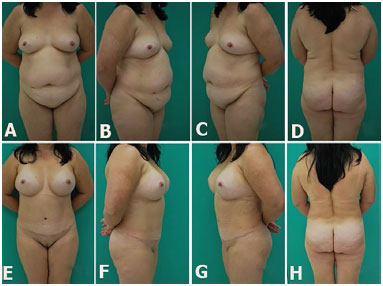
Figure 8. M.L., 40 years old, abdominoplasty and liposuction with concomitant mammoplasty. (A, B, C, and D) preoperatively; (E, F, G, and H) 7 months postoperatively.
2007: 56 patients
Abdominoplasty + liposuction - 56 female patients
Fixation suture used, reduced dissection.
Absence of seroma: 27% with drain, 52% without drain
Presence of seroma: 10% with drain, 11% without drain
2008: 64 patients
Abdominoplasty + liposuction - 63 female and 1 male patients
Fixation suture used, reduced dissection.
Absence of seroma: 17% with drain, 31% without drain
Presence of seroma: 34% with drain, 18% without drain
2009: 60 patients
Abdominoplasty + Liposuction - 58 female and 2 male patients
Fixation suture used, reduced dissection.
Absence of seroma: 43% with drain, 29% without drain.
Presence of seroma: 18% with drain, 10% without drain
2010: 72 patients
Abdominoplasty + liposuction - 72 female patients
Fixation suture used, reduced dissection.
Absence of seroma: 42.2% with drain, 25.9% without drain
Presence of seroma: 21.9% with drain, 10% without drain
2011: 74 patients
Abdominoplasty + liposuction - 73 female and 1 male patients
Fixation suture used, reduced dissection.
Absence of seroma: 34.48% with drain, 49.29% without drain.
Presence of seroma: 16.23% with drain, 0% without drain
2012: 66 patients
Abdominoplasty + liposuction - 66 female patients
Fixation suture used, reduced dissection.
Absence of seroma: 60.60% with drain, 33.33% without drain.
Presence of seroma: 6.07% with drain, 0% without drain
2013: 53 patients
Abdominoplasty+ liposuction - 52 female and 1 male patients
Fixation suture used, reduced dissection.
Absence of seroma: 82% with drain, 15% without drain
Presence of seroma: 3% with drain, 0% without drain
2014: 55 patients
Abdominoplasty+ liposuction- 50 female and 5 male patients
Fixation suture used, reduced dissection.
Absence of seroma: 80% with drain, 20% without drain
Presence of seroma: 0% with drain, 0% without drain
CONCLUSION
Fixation sutures on the flap were effective in the prevention of seroma. The use of aspiration drains did not decrease the incidence of seroma in this study. The combination of abdominoplasty techniques with reduced dissection and liposuction helped in the refinement of the results.
COLLABORATIONS
JAC Design of the project; implementation of research; analysis and/or interpretation of data; completion of operations and/or experiments and approval; writing of the manuscript; final approval of the version to be published.
RB Writing of the manuscript and critical review of its content; final approval of the manuscript.
ACKNOWLEDGEMENTS
Lilian R Nóbrega Marques; Angela Kuninari; Dr. Heitor Yassuda; Dr. Masashi Munechika.
REFERENCES
1. Montenegro CAB, Rezende Filho J. O Mecanismo do parto. In: Montenegro CAB, Rezende Filho J. Obstetrícia Fundamental. 3º Ed. Rio de Janeiro: Guanabara Koogan; 1980. p.183-9.
2. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthetic Surg J. 1998;18(6):439-41.
3. Saldanha OR, De Souza Pinto EB, Mattos WN Jr, Pazetti CE, Lopes Bello EM, Rojas Y, et al. Lipoabdominoplasty with selective and safe undermining. Aesth Plastic Surg. 2003;27(4):322-7. PMID: 15058559
4. Saldanha O. Lipoabdominoplastia. Rio de Janeiro: Di-Livros; 2004.
5. Avelar J. Fat suction versus abdominoplasty. Aesth Plast Surg. 1985;9(4):265-75.
6. Stocchero IN. Ultrasound and seromas. Plastic Reconstr Surg. 1993;91(1):198. PMID: 8416535
7. Nahas FX, Ferreira LM, Ghelfond C. Does quilting suture prevent seroma in abdominoplasty? Plastic Reconstr Surg. 2007;199(3):1060-6.
8. Pollock H, Pollock T, Progressive tension sutures: a technique to reduce local complications in abdominoplasty. Plast Reconstr Surg. 2000;105(7):2583-8.
9. Matarasso A. Liposuction as an adjunct to a full abdominoplasty revisited. Plast Reconstr Surg. 2000;106(5):1203-5.
10. Avelar J. Cicatriz umbilical: da sua importância e da técnica de confecção nas abdominoplastias. Rev Bras Cir. 1979;69(1/2):41-52.
Sociedade Brasileira de Cirurgia Plástica, São Paulo, SP, Brazil
Institution: Hospital Nipo Brasileiro, São Paulo, SP, Brazil.
Corresponding author:
Julio Alberto Soncini
Rua Josefina Mandotti, 340 cj 54 - Jardim Maia-Guarulhos
São Paulo, SP, Brazil Zip Code 07115-080
E-mail: jasoncini@uol.com.br
Article received: June 11, 2012.
Article accepted: April 15, 2016.
Conflicts of interest: none.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter