ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Comparative study between abdominoplasty with suction drainage and without suction drainage but using adhesion stitches
Estudo comparativo de abdominoplastias com drenagem a vácuo e sem drenagem, mas com pontos de adesão
ABSTRACT
INTRODUCTION: Abdominoplasty is one of the most common procedures performed by plastic surgeons. The goal of this study is to evaluate the outcome and the occurrence of complications in patients undergoing abdominoplasty using the en bloc resection technique, and to look for differences in evolution when a drain is used or is replaced with adhesion stitches.
METHODS: A prospective study was conducted on 34 female patients undergoing abdominoplasty. These were alternately placed into 2 groups: in one group suction drains were used, and in the other these were replaced with adhesion stitches.
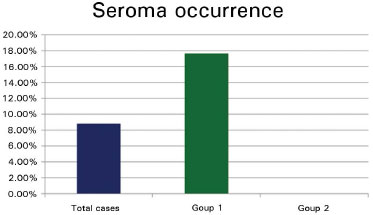
RESULTS: Among all the cases, there was some degree of scar widening in 14.7% of patients. When analyzed by group, those who received drains had a higher incidence (23.53%) comparing to those who received adhesion stitches (5.88%). One patient had superficial vein thrombosis of the lower limbs with a good outcome. Three cases of seroma were diagnosed, all of them in the group using drains. These represent 8.82% of the entire study and 17.64% of the specific group. The aesthetic result was considered good by 94.12% of all patients.
CONCLUSIONS: The en bloc resection abdominoplasty technique proved to be safe, easy to perform, assured good aesthetical results and had similar complication rates when compared to other techniques. The adhesion stitches were effective for preventing complications in this study.
Keywords:
Abdominoplasty; Postoperative Complications; Seroma; Scars.
RESUMO
INTRODUÇÃO: A abdominoplastia é um dos procedimentos mais comumente realizados por cirurgiões plásticos. O objetivo do estudo foi avaliar a evolução e a ocorrência de complicações em pacientes submetidos à abdominoplastia pela técnica de ressecção em bloco, e observar se existe alguma diferença na evolução com a utilização de dreno ou de pontos de adesão.
MÉTODOS: Foi realizado um estudo prospectivo de 34 pacientes do sexo feminino, submetidas à abdominoplastia. Foram divididas em dois grupos alternadamente; em um deles foi utilizado dreno de aspiração a vácuo e no outro não, mas estes últimos receberam pontos de adesão.
RESULTADOS: Do total operado, houve algum grau de alargamento da cicatriz em 14,7% dos casos. Quando avaliado separadamente por grupo, aqueles que foram drenados tiveram incidência maior (23,53%) em comparação com os que receberam pontos de adesão (5,88%). Ocorreu um caso de trombose de veias superficiais de membros inferiores, com boa evolução. Foram diagnosticados três casos de seroma, todos no grupo com dreno. Eles representaram 8,82% do total estudado e 17,64% dos casos deste grupo. O resultado estético foi considerado muito bom por 94,12% das pacientes estudadas.
CONCLUSÕES: A técnica de ressecção em bloco se mostrou segura, de fácil execução, com bons resultados estéticos e índices de complicações semelhantes às outras técnicas descritas na literatura. Os pontos de adesão foram eficazes na prevenção de complicações neste estudo.
Palavras-chave:
Abdominoplastia; Complicações pós-operatórias; Seroma; Cicatriz.
INTRODUCTION
Abdominoplasty is one of the most popular procedures in plastic surgery; it is most commonly sought by women, especially after pregnancy. Although men currently represent a small share of the patients desiring this procedure, they are ever more concerned about their appearance. Additionally, the number of men and women undergoing bariatric surgery is growing, and are a group which often need abdominoplasty. Usual complaints are: skin laxity, excess skin, stretch marks, abdominal bulging, excess amounts of abdominal fat, previous scarring in the lower abdomen (especially from c-sections or gynecological surgeries), irregularities of the abdominal surface, and umbilical hernia. The physical examination often reveals diastasis recti. Plication of these muscles is done alongside abdominoplasty and has become a routine addition to this procedure, because not only does it correct the diastasis but also guarantees a stiffening of the abdominal wall and decreases waist circumference.
As with all surgeries, there can be complications in abdominoplasty. Seroma is the most common complication in this procedure1. Some factors that increase its incidence are overweight, obesity, patients with significant weight loss, and existence of previous supra-umbilical incisions2. Another important risk factor is the presence of dead space between the muscle aponeurosis and the dermo-adipose flap after the surgery. Seromas should be treated with percutaneous aspiration, compression, and rigorous follow-up, because seroma may relapse and require several aspirations. If a seroma is not noted and remains untouched for a long period, a capsule will form around it. This capsule may undergo scar contraction and lead to secondary deformities with visible and palpable distortions in the abdominal wall3. When this occurs, extensive reconstructive surgery may be required. In 1998, Baroudi & Ferreira4 reported a technique using adhesion stitches between the abdominal flap and the muscle aponeurosis during abdominoplasty to prevent seroma formation. Other authors have adopted this technique with good results5-8.
Other complications which have been described are: hematoma, infection, pathological scar formation (keloids or hypertrophic scarring), wound dehiscence, umbilical stenosis or enlargement, umbilical necrosis, deep venous thrombosis, pulmonary embolism, death, respiratory distress due to the plication, and abdominal skin necrosis.
OBJECTIVE
To the evolution and incidence of complications in two groups of patients after abdominoplasty using the en bloc resection technique described and standardized by Ronaldo Pontes9; one group received suction drainage and the other received adhesion stitches without any kind of drainage.
METHODS
A prospective study was conducted from February 2008 to November 2012. All 34 patients who underwent abdominoplasty were divided into two groups in an alternating sequence according to the order in which their surgery was performed. All the surgeries were performed by the author of this study, using the en bloc resection abdominoplasty technique9. All patients received liposuction of the superior abdomen and flanks. The surgery in Group 1 followed the original technique as well as suction drainage, while Group 2 received adhesion stitches and no drain. All patients were female. The youngest patient was 23 years old and the two oldest patients were 67 years old. The average age was 40.05 years and the median age was 42 years. All of them had at least one previous pregnancy and diastasis recti.
Operative Technique
All patients underwent en bloc resection abdominoplasty. This technique was developed by Prof. Ronaldo Pontes in the early 1960s and was first reported in 1964 in the III Jornada da Regional in Petrópolis no Colégio Internacional de Cirurgiões and was latter formalized in 1971 in the VIII Congresso Brasileiro de Cirurgia Plástica. It is described in detail in a book dedicated entirely to this method9.
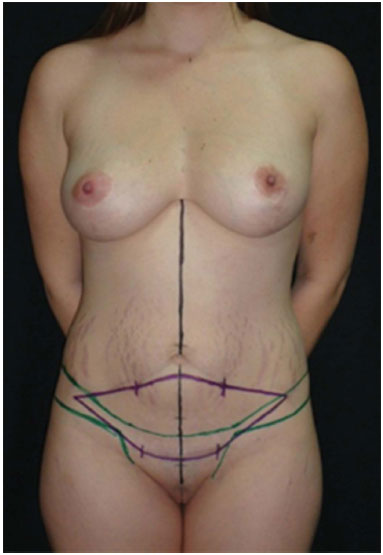
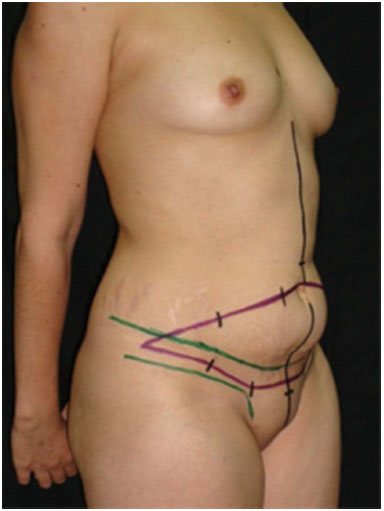
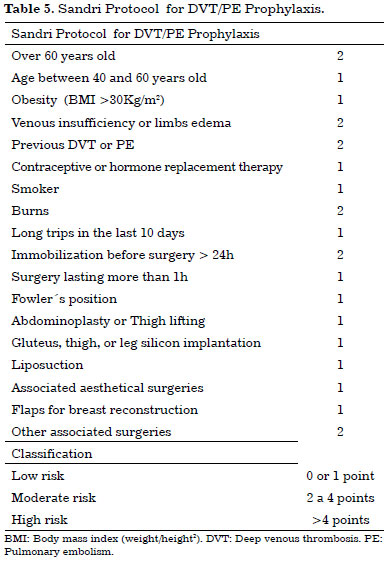
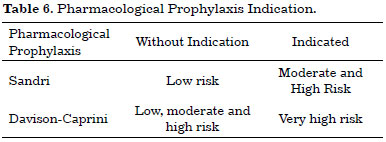
A description of the technique: excess skin and adipose tissue is marked prior to the surgery; the patient is asked to bring a bikini or underwear to this consultation. The marking is done with a waterproof marker so that the markings will not be washed off during pre-surgical preparation. First, the edges of the bikini or underwear are drawn. This will serve as a guide for the height of the central part of the incision and also the angle of the lateral segments. This process guarantees that the scar can be easily hidden by clothing, allowing the patient to go to the beach or swimming pools without any concerns related to visible scarring.
Next, an ellipse containing the excess tissue that needs to be removed is marked on the lower abdomen (Figures 1 and 2). This excess is assessed by a manual pinch maneuver and should occur with the patient standing, sitting, and laying down. This must be done in a careful and unhurried manner in a suitable environment, with the patient relaxed and unclothed, and the surgeon take care to check as many times as needed to avoid excessive tension after resection. The advantages of this technique are: resection is facilitated, no need to hold a heavy and long flap during the dissection, better symmetry and positioning of the resulting scar, easier to control bleeding during dissection, reduced operative time, stimulates preoperative planning, and since the marking is generally done the day prior to the procedure or in the infirmary, it also reduces the time spent in the operating room, the time under anesthesia, and the total procedure time.
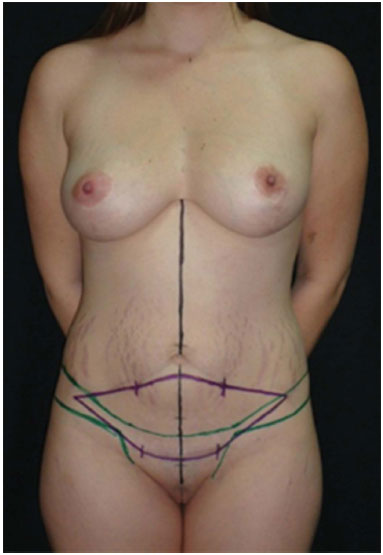
Figure 1. Typical marking for bloc resection technique. Black line marks the medium line. Green line marks the waistline contouring. Purple line marks the excessive skin to be resected en bloc.
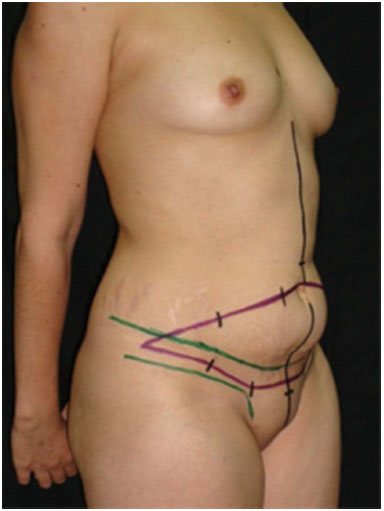
Figure 2. Typical marking for bloc resection technique in another patient in semiprofile position. Black line marks the medium line. Green lines mark the waistline contouring. Purple line marks the excessive skin to be resected en bloc.
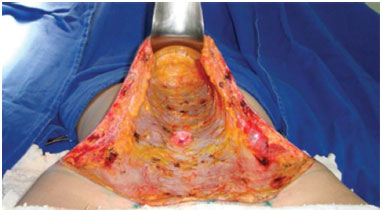
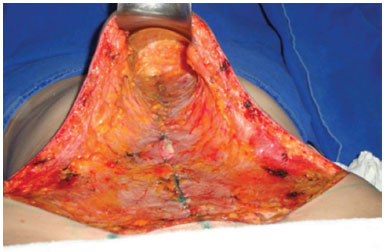
The surgery begins by checking the marks with a ruler and caliper. The area to be operated is infiltrated with a saline solution with adrenaline at a concentration of 1:500.000. Liposuction is performed where necessary in previously-marked areas. The liposuction accesses can be made anywhere within the previously-marked ellipse and a 3 or 4mm cannula is used. The umbilicus is removed, and en bloc resection of the previously-marked ellipse is performed in the skin and subcutaneous tissue until the muscular aponeurosis is reached (Figures 3 and 4).

Figure 3. Skin incision with scalpel until the fatty tissue of the previous marked area.

Figure 4. En bloc resection of previous marked area. Dissection plan was the muscular aponeurosi.
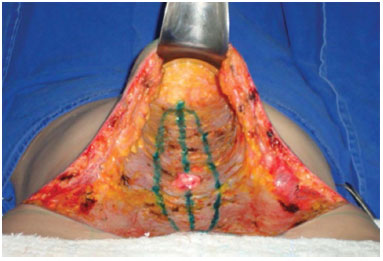
A supra-umbilical tunnel is created on the plane just above the aponeurosis toward the level of the xiphoid appendix; this tunnel should be as small as narrow as possible to allow muscle plication and correction of diastasis recti (Figure 5). The skin is incised with a scalpel and the undermining is done with the electric scalpel. Hemostasis is performed. The diastasis is then marked and an ellipse centered on the midline is marked for the plication. The plication is conducted on two planes, the first one with separated double stitches using Monocryl 2-0 line, and the second a running suture with Prolene 0 (Figures 6 and 7). The umbilicus is attached to the aponeurosis by four stitches of nylon 4-0 line. The flap is pulled taut and the umbilical projection is marked on the skin. This point is incised and the fat under it is removed to allow transposition of the umbilicus.
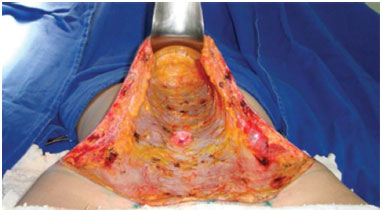
Figure 5. Supra-umbilical tunnel dissected toward the level of the xiphoid appendix.
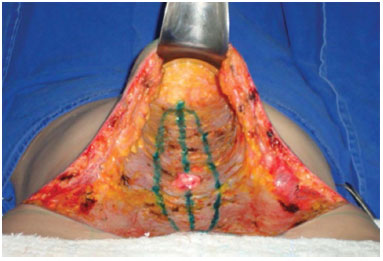
Figure 6. Medium line marking and ellipse where the plication was made.
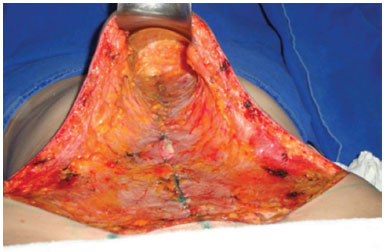
Figure 7. The appearance after plication.
At this point, treatment of the two groups diverges. In Group 1, two suction drains are inserted: one is directed towards the supra-umbilical tunnel and the other is placed within the lower abdomen. The flap is definitively pulled down and sutured in at least 3 layers according to the thickness of the adipose panicle. The deeper plane is sutured using simple Monocryl 3-0 sutures, the intermediate plane follows with inverted and separated Monocryl 3-0 sutures, and the most superficial plane is closed with intradermal running Monocryl 4-0 sutures.
Group 2 received adhesion stitches, as described by Baroudi & Ferreira4. These are simple separated stitches using Vicryl 1 line to join the fat from the flap to the muscle aponeurosis, fixing the flap in various areas to reduce dead space, alleviate scar tension, and immobilize the flap. A large number of stitches (30 to 40 stitches) are advocated by Baroudi, Ferreira and other authors; in this study fewer stitches were used according to evaluation during the procedure (20 to 25 stitches). The patients in Group 2 did not receive any kind of drain4,7. After the adhesion stitches were placed, the procedures follow the same steps as in Group 1 (Figures 8 to 10).

Figure 8. Placement of adhesion stitches. Here, the flap stitch can be observed.

Figure 9. Placement of adhesion stitches. Aponeurosis stitc can be observed.

Figure 10. Final appearance of the surgery. No drains were placed.
All patients received occlusive cotton dressings and were placed in Fowler position.
Postoperative
The surgeries were all performed in hospitals and the patients remained in the hospital for 24 hours. Dressings were replaced with compression wrappings on the following day, and these were used 24 hours/day during the first month and 12 hours/day in the second month. Patients were encouraged to walk as soon as possible, but were directed to maintain their backs curved while standing for 21 days to avoid excessive tension on the scar; they were also told to stay in Fowler position when laying down for this same period.
The patients were seen by the surgeon every week for 1 month, every 15 days in the second month, and returned at 3, 6, and 12 months after surgery.
In Group 1, the drain balance was noted daily, and the drains were only removed when drainage was less than 40ml in 24 hours. The maximum time until drain removal was 5 days.
RESULTS
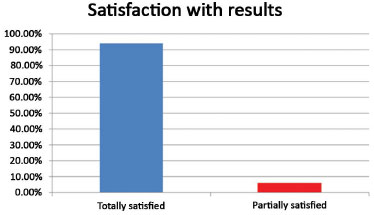
Of all the operated patients, only 2 (5.88%) were not completely satisfied with the aesthetic result. They complained that a bulge remained in the upper abdomen. This was the result of a large amount of intra-abdominal fat that precluded the achievement of a completely flat abdomen, although those patients did obtain a significant improvement in the appearance. Both patients had BMI over 30 Kg/m2 (obesity). The other 32 patients (94.12%) were completely satisfied with the aesthetical result. (Table 1 and Figure 11).

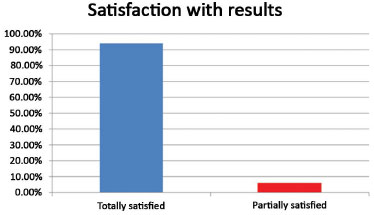
Figure 11. Total satisfaction with aesthetical results.
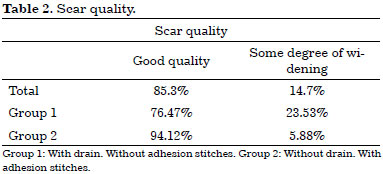
Scar quality was considered good by the surgeon and the patient in 29 cases (85.3%), but some degree of widening did occur, especially in the central area of the scar, in 5 cases (14.7%). Four of these occurred in Group 1 (23.53% of the cases in this group). Only one of these cases occurred in Group 2 (5.88% of this group). (Table 2 and Figure 12).
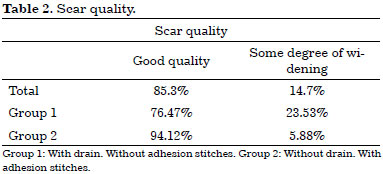

Figure 12. A: Scar quality in Group 1, i.e., with drain and without adhesion stitches. B: Scar quality in Group 2, i.e., without drain and with adhesion stitches.
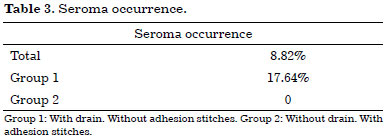
Three cases of seroma were diagnosed, all in Group 1. They represented 8.82% of the total number of patients studied and 17.64% of the patients in Group 1. After seroma was diagnosed, the patients were seen by the surgeon every 4 days. One of these patients had spontaneous drainage through the scar on the 10th postoperative day but no subsequent drainage. The other 2 patients were diagnosed on the 7th day and were treated with needle aspiration. One patient had 80 ml aspirated and exhibited no relapse. The other patient had initial drainage of 120 ml, relapsed with 100 ml on the 11th day, and additional drainage of 60 ml on the 15th day, after which no more drainage occurred. (Table 3 and Figure 13).
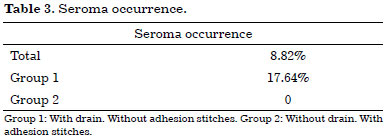
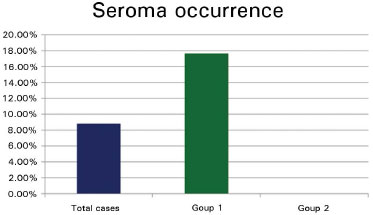
Figure13. Seroma occurrence. Group 1: with drain. Without adhesion stitches. Group 2: Without drain. With adhesion stitches.
There was one diagnosis of superficial vein thrombosis in the lower limb of a patient in Group 1 on the 7th day after surgery. The patient was 37 years old and had a BMI of 28.19 Kg/m2 (overweight). The diagnosis was made based after clinical examination that revealed pain upon lower limb compression, positive Homans' sign, and swelling, and was confirmed by Doppler ultrasound. Even though the thrombosis was superficial, the vascular surgeon consulted in this case opted to hospitalize the patient and use low molecular weight heparin (enoxaparin) subcutaneously along with oral warfarin until adequate levels were reached. After 5 days the patient was discharged and continued use of warfarin for 3 months, and had a good outcome.
No patients had hematoma, scar dehiscence, infection, necrosis, or keloid formation. These complications are often reported in medical literature related to abdominoplasty.
DISCUSSION
Patient dissatisfaction is considered by many surgeons to be one of the worst and most difficult complications, since it involves not only objective but mainly subjective criteria. Sometimes patients are unhappy with clearly poor results, but often while the result is quite positive, it is not what the patient had in mind. In some cases, the patient's desired outcome is not possible, whether because of technical impossibilities or physical characteristics that are difficult if not impossible to alter. In other cases, the patient has some type of body dysmorphism or other psychological disorder.
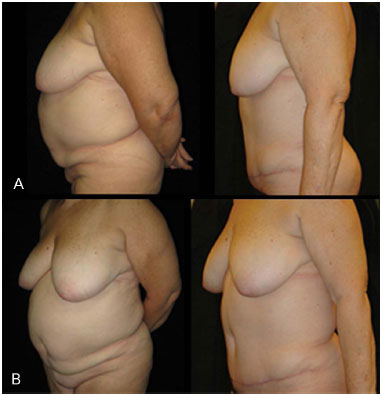
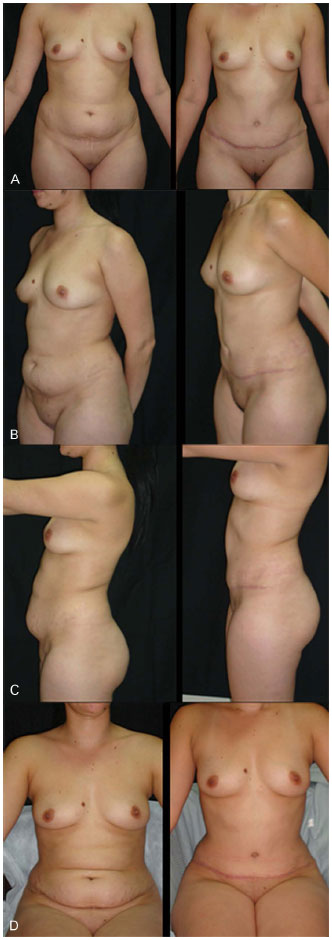
In this study, two patients were not completely satisfied with the aesthetical results. Both of them were happy with the overall effect but expected better results in the upper abdomen. Both had BMI exceeding 30 Kg/m2 (obesity) and had a large amount of intra-abdominal fat with very significant abdominal bulging before the surgery. After the limits of the procedure were explained to them, they accepted the achieved results. Note that 94.12% of cases were very satisfied with the aesthetical results (Figures 14 and 15).
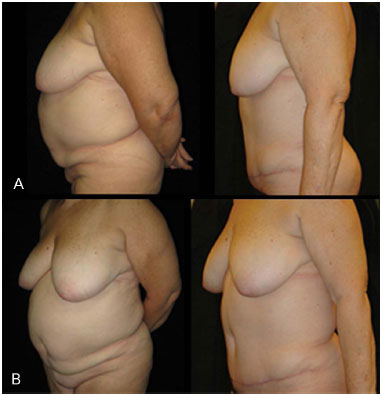
Figure 14. A: Preoperative and postoperative images. B: Preoperative and postoperative images. Semiprofile view.
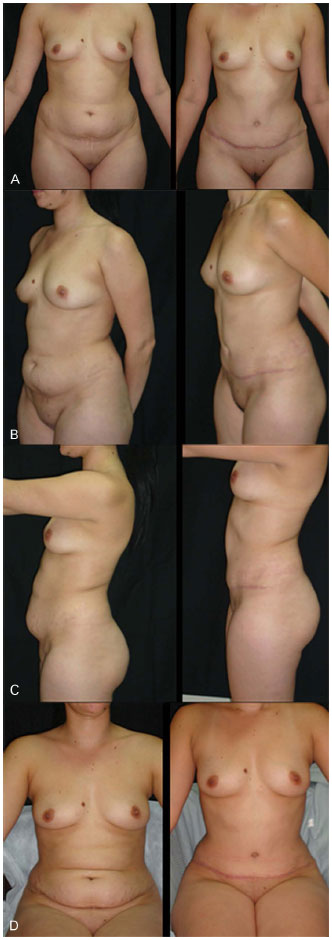
Figure 15. A: Preoperative and postoperative images. Front view. B: Preoperative and postoperative images. Semiprofile view. C: Preoperative and postoperative images. Profile view. D: Preoperative and postoperative images. Image taken with the patient seated.
Scar widening was observed in 14.7% of all the patients studied. The principal cause is excessive tension; this may occur due to failure in the marking, over-resection, or because the patient did not follow the postoperative recommendations related to posture. When each group is examined separately, Group 1 had more cases of scar widening (23.53%) compared to Group 2 (5.88%). We can suggest that the reason for this difference is reduced scar tension due to the distribution of force between the adhesion stitches that hold the flap to the aponeurosis from the base to its extremity.
Seroma is a frequent complication following abdominoplasty. The literature shows that it has been identified in 1 to 20% of cases in retrospective studies7,10-15. Prospective studies showed a higher number of cases, ranging from 38 to 42%1,16. According to Nahas et al.7 data from retrospective studies can be underestimated because seroma is considered a minor complication, and this information may be absent from the patient's file.
Dead space between the abdominal flap and the muscle aponeurosis after undermining is an important factor in seroma formation. Moreover, shear forces can break the fragile links between the flap and the aponeurosis in the initial period of wound healing. The adhesion stitches can reduce this effect by eliminating the dead space and promoting strong flap fixation, which in turn promotes healing and reduces the incidence of seroma.
This study strengthens this theory, as it shows that in Group 2 there were no cases of seroma, while it was diagnosed in 17.64% of cases of Group 1.
Seroma is usually diagnosed between 7 and 10 days after surgery. The maximum period of drainage in this study was 5 days, and therefore it could not have prevented the occurrence of seroma.
Baroudi & Ferreira4, Nahas7 and other authors report the use of a large number of adhesion stitches, between 30 and 40. In this study, 20 to 25 stitches were used. Even a smaller number of stitches was effective in preventing seroma formation and scar widening, as seen in the different incidence of those complications between the two groups.
Thromboembolic complications require special attention, and their prevention is extremely important, since they lead to serious morbidity and mortality. Pulmonary embolism (PE) is the most dramatic complication, with a mortality rate of 40 to 50%17,18. Pannucci et al.19 conducted a wide review of the literature at the University of Michigan and Vanderbilt University, which showed that 10% of patients with symptomatic pulmonary embolism died in 60 minutes, and that survivors can suffer right ventricular dysfunction or heart failure. Patients with deep venous thrombosis (DVT) can develop post-thrombotic syndrome that compromises quality of life. Pannuci's study also concluded that hospitalized patients often receive inadequate prophylaxis, and pointed out that plastic surgeons use less chemoprophylaxis than recommended in high-risk patients and may fail to recognize and modify thromboembolic risk factors19.
One reason that makes some plastic surgeons avoid the use of chemoprophylaxis is concern with hemorrhagic complications and hematoma formation. Several studies have already proven the safety of low molecular weight heparin as a prophylactic drug. Jatene stated that these drugs do not have thrombolytic action, but only prevent thrombus formation17,18. In 2008, the Plastic Surgery Foundation (American Society of Plastic Surgeons) started a deep venous thrombosis prevention study which showed after 30 months that enoxaparin use during the postoperative period of hospitalized patients reduced the rates of symptomatic venous thromboembolism without changing the number of reoperations due to hematoma19-22.
Abdominoplasty is a procedure with a high incidence of this serious complication. Papers published on this topic, specifically in plastic surgery, have increased in the last years. They state that the DVT incidence in face lifting is 0.35%23, in liposuction is 0.6%24, and in abdominoplasty is about 1.3%25,26; if circumferential abdominoplasty and abdominoplasty associated with intra-abdominal surgery are considered separately, the incidence increases to 3.4 and 2.17% respectively27. The TRAM flap has a DVT incidence of 1.3%28. Regarding pulmonary embolism, some data are: face lifting has a DVT incidence of 0.14%23, abdominoplasty has 0.8%26, when abdominoplasty is associated with other surgeries the incidence ranges from 1.1%29 to 6.6%30, in liposuction it is 1.1%24, and in TRAM flap it ranges from 0.7% to 18.8%31,32.
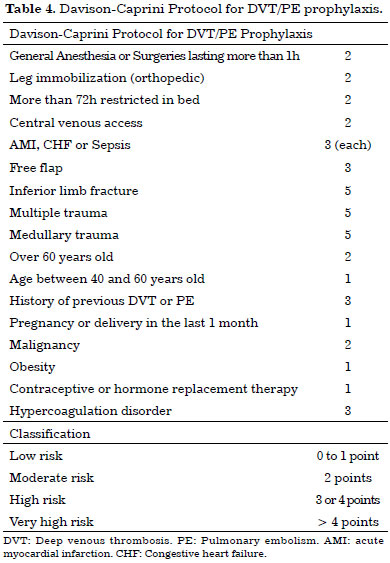
Some thromboembolic prevention protocols have been published. In Tables 4, 5, and 6 this study presents two important protocols: the Sandri Protocol, published by Brazilian authors, and the Davison-Caprini Protocol, published by American authors. The nonpharmacological prevention measures are use of intermittent compressive devices in the legs and encouraging the patient to start walking as soon as possible after surgery, and should be ensured in all patients13,17,33. According to the risk stratification, each protocol indicates the use or non-use of pharmacological prophylaxis, as shown in Tables 4, 5, and 634-36. When indicated, this prophylaxis is done by administering subcutaneous enoxaparin (Clexane) 40 mg, initiating 12 hours after surgery and repeating the dose every 24 hours until the patient is walking normally.
The author of this article used the Davison-Caprini Protocol during this study. All patients received the nonpharmacological prophylaxis and 8 of them (23.5%) had indication for pharmacological prophylaxis. None of these 8 patients who received enoxaparin had abnormal bleeding or hematoma formation. Even though the prevention measures were followed, there was one case of superficial venous thrombosis, which was diagnosed early and treated without further consequences. It is important to emphasize that this patient did not have indications to receive enoxaparin according to the protocol used during the study. But we can also note that this was a case of superficial venous thrombosis, an event with less morbidity compared to deep venous thrombosis.
CONCLUSIONS
The en bloc resection technique was seen to be safe and easy to perform, with good aesthetical results and complication rates similar to other techniques described in the medical literature.
The adhesion stitches showed advantages in reducing complications when compared to the control group. It is a simple technique and has a fast learning curve. However, it increases operating time. This time can be reduced as the surgeon's experience increases and with the possibility of using less stitches than originally described by Baroudi and Ferreira. As demonstrated in this study, even with a reduced number of stitches, the benefits remain.
A better evaluation of scar quality would be obtained if some method of quantification were used to determine the degree of scar widening.
The diagnosis of seroma would be improved if an ultrasound were used as a screening method. This might more accurately determine the presence of small amounts of fluid collection. However, its use in daily practice would make postoperative follow-up more onerous and complex.
Measures to prevent thromboembolic events should be adopted for all surgeries.
REFERENCES
1. Hafezi F, Nouhi AH. Abdominoplasty and seroma. Ann Plast Surg. 2002;48(1):109-10. DOI: http://dx.doi.org/10.1097/00000637-200201000-00022
2. de Castro CC, Aboudib Júnior JH, Salema R, Gradel J, Braga L. How to deal with abdominoplasty in an abdomen with a scar. Aesthetic Plast Surg. 1993;17(1):67-71. DOI: http://dx.doi.org/10.1007/BF00455052
3. Hay-Roe V. Seroma after lipoplasty with abdominoplasty. Plast Reconstr Surg. 1991;87(5):997-8. PMID: 1826790 DOI: http://dx.doi.org/10.1097/00006534-199105000-00041
4. Baroudi R, Ferreira CA. Seroma: how to avoid it and how to treat it. Aesthet Surg J. 1998;18(6):439-41. PMID: 19328174 DOI: http://dx.doi.org/10.1016/S1090-820X(98)70073-1
5. Pollock H, Pollock T. Progressive tension sutures: a technique to reduce local complications in abdominoplasty. Plast Reconstr Surg. 2000;105(7):2583-6. DOI: http://dx.doi.org/10.1097/00006534-200006000-00047
6. Rios JL, Pollock T, Adams WP Jr. Progressive tension sutures to prevent seroma formation after latissimus dorsi harvest. Plast Reconstr Surg. 2003;112(7):1779-83. PMID: 14663220 DOI: http://dx.doi.org/10.1097/01.PRS.0000090542.68560.69
7. Nahas FX, Ferreira LM, Ghelfond C. Does quilting suture prevent seroma in abdominoplasty? Plast Reconstr Surg. 2007;119(3):1060-4.
8. Oliveira EA, Valera F, Monte ALR, López C. Prevenção do seroma nas abdominoplastias associadas à lipoaspiração e sem drenagem ativa. Rev Bras Cir Plást. 2008;23(1):41-7.
9. Pontes R. Abdominoplastia: ressecção em bloco e sua aplicação em lifting de coxa e torsoplastia. Rio de Janeiro: Revinter; 2004.
10. Grazer FM, Goldwyn RM. Abdominoplasty assessed by survey, with emphasis on complications. Plast Reconstr Surg. 1977;59(4):513-7. PMID: 847027 DOI: http://dx.doi.org/10.1097/00006534-197759040-00006
11. Avelar J. Fat suction versus abdominoplasty. Aesthetic Plast Surg. 1985;9(4):265-75. DOI: http://dx.doi.org/10.1007/BF01571045
12. Cardoso de Castro C, Cupello AM, Cintra H. Limited incisions in abdominoplasty. Ann Plast Surg. 1987;19(5):436-47. DOI: http://dx.doi.org/10.1097/00000637-198711000-00009
13. Dillerud E. Abdominoplasty combined with suction lipoplasty: a study of complications, revisions, and risk factors in 487 cases. Ann Plast Surg. 1990;25(5):333-8. DOI: http://dx.doi.org/10.1097/00000637-199011000-00001
14. Floros C, Davis PK. Complications and long-term results following abdominoplasty: a retrospective study. Br J Plast Surg. 1991;44(3):190-4. PMID: 1827355 DOI: http://dx.doi.org/10.1016/0007-1226(91)90125-4
15. Chaouat M, Levan P, Lalanne B, Buisson T, Nicolau P, Mimoun M. Abdominal dermolipectomies: early postoperative complications and long-term unfavorable results. Plast Reconstr Surg. 2000;106(7):1614-8. DOI: http://dx.doi.org/10.1097/00006534-200012000-00029
16. Mohammad JA, Warnke PH, Stavraky W. Ultrasound in the diagnosis and management of fluid collection complications following abdominoplasty. Ann Plast Surg. 1998;41(5):498-502. PMID: 9827952 DOI: http://dx.doi.org/10.1097/00000637-199811000-00008
17. Jatene PR, Jatene MC, Barbosa AL. Abdominoplastia: experiência clínica e revisão da literatura. Rev Bras Cir Plást. 2005;20(2):65-71.
18. Abs R. Accidents thromboemboliques en chirurgie plastique: revue de la literature et proposition d'un algorithme de prophylaxie. Ann Chir Plast Esthet. 2000;45(6):604-9.
19. Pannucci CJ, Jaber RM, Zumsteg JM, Golgotiu V, Spratke LM, Wilkins EG. Changing practice: implementation of a venous thromboembolism prophylaxis protocol at an academic medical center. Plast Reconstr Surg. 2011;128(5):1085-92. PMID: 21738084 DOI: http://dx.doi.org/10.1097/PRS.0b013e31822b67ff
20. Pannucci CJ, Bailey SH, Dreszer G, Fisher Wachtman C, Zumsteg JW, Jaber RM, et al. Validation of the Caprini risk assessment model in plastic and reconstructive surgery patients. J Am Coll Surg. 2011;212(1):105-12. DOI: http://dx.doi.org/10.1016/j.jamcollsurg.2010.08.018
21. Pannucci CJ, Dreszer G, Wachtman CF, Bailey SH, Portschy PR, Hamill JB, et al. Postoperative enoxaparin prevents symptomatic venous thromboembolism in high-risk plastic surgery patients. Plast Reconstr Surg. 2011;128(5):1093-103. PMID: 22030491 DOI: http://dx.doi.org/10.1097/PRS.0b013e31822b6817
22. Pannucci CJ, Wachtman CF, Dreszer G, Bailey SH, Portschy PR, Hamill JB, et al. The effect of postoperative enoxaparin on risk for reoperative hematoma. Plast Reconstr Surg. 2012;129(1):160-8. PMID: 21915085 DOI: http://dx.doi.org/10.1097/PRS.0b013e318236215c
23. Reinisch JF, Bresnick SD, Walker JW, Rosso RF. Deep venous thrombosis and pulmonary embolus after face lift: a study of incidence and prophylaxis. Plast Reconstr Surg. 2001;107(6):1570-5. DOI: http://dx.doi.org/10.1097/00006534-200105000-00044
24. Albin R, de Campo T. Large-volume liposuction in 181 patients. Aesthetic Plast Surg. 1999;23(1):5-15. DOI: http://dx.doi.org/10.1007/s002669900235
25. Grazer FM, Goldwyn RM. Abdominoplasty assessed by survey, with emphasis on complications. Plast Reconstr Surg. 1977;59(4):513-7. PMID: 847027 DOI: http://dx.doi.org/10.1097/00006534-197759040-00006
26. van Uchelen JH, Werker PM, Kon M. Complications of abdominoplasty in 86 patients. Plast Reconstr Surg. 2001;107(7):1869-73. DOI: http://dx.doi.org/10.1097/00006534-200106000-00037
27. Hatef DA, Trussler AP, Kenkel JM. Procedural risk for venous thromboembolism in abdominal contouring surgery: a systematic review of the literature. Plast Reconstr Surg. 2010;125(1):352-62. PMID: 20048626 DOI: http://dx.doi.org/10.1097/PRS.0b013e3181c2a3b4
28. Erdmann D, Sundin BM, Moquin KJ, Young H, Georgiade GS. Delay in unipedicled TRAM flap reconstruction of the breast: a review of 76 consecutive cases. Plast Reconstr Surg. 2002;110(3):762-7. PMID: 12172136 DOI: http://dx.doi.org/10.1097/00006534-200209010-00007
29. Hester TR Jr, Baird W, Bostwick J 3rd, Nahai F, Cukic J. Abdominoplasty combined with other major surgical procedures: safe or sorry? Plast Reconstr Surg. 1989;83(6):997-1004. PMID: 2524854
30. Voss SC, Sharp HC, Scott JR. Abdominoplasty combined with gynecologic surgical procedures. Obstet Gynecol. 1986;67(2):181-5. PMID: 3945426 DOI: http://dx.doi.org/10.1097/00006250-198602000-00005
31. Olsson EH, Tukiainen E. Three-year evaluation of late breast reconstruction with a free transverse rectus abdominis musculocutaneous flap in a county hospital in Sweden: a retrospective study. Scand J Plast Reconstr Surg Hand Surg. 2005;39(1):33-8. DOI: http://dx.doi.org/10.1080/02844310410021730
32. Spear SL, Ducic I, Low M, Cuoco F. The effect of radiation on pedicled TRAM flap breast reconstruction: outcomes and implications. Plast Reconstr Surg. 2005;115(1):84-95. PMID: 15622237
33. Moulin JL, Sobreira ML, Malgor RD, Abreu CR, Araújo ESF, Palhares Neto AA. Estudo comparativo entre protocolos para profilaxia da trombose venosa profunda: uma nova proposta. Rev Bras Cir Plást. 2010;25(3):415-22. DOI: http://dx.doi.org/10.1590/S1983-51752010000300003
34. Sandri JL. Profilaxia do tromboembolismo em cirurgia plástica. In: Carreirão S, Cardim V, Goldenberg D, eds. Cirurgia Plástica - Sociedade Brasileira de Cirurgia Plástica. São Paulo: Atheneu; 2005. p.119-25.
35. Caprini JA, Arcelus JI, Reyna JJ. Effective risk stratification of surgical and nonsurgical patients for venous thromboembolic disease. Semin Hematol. 2001;38(2 Suppl 5):12-9. DOI: http://dx.doi.org/10.1053/shem.2001.25184
36. Davison SP, Venturi ML, Attinger CE, Baker SB, Spear SL. Prevention of venous thromboembolism in the plastic surgery patient. Plast Reconstr Surg. 2004;114(3):43E-51E. PMID: 15318036 DOI: http://dx.doi.org/10.1097/01.PRS.0000131276.48992.EE
1. Clínica Trufino, Londrina, PR, Brazil
2. Serviço de Residência Médica em Cirurgia Plástica do Prof. Ronaldo Pontes - Rio de Janeiro, RJ, Brazil
Institution: Clínica Trufino, Londrina, PR, Brazil.
Corresponding author:
Antonio Juliano Trufino
Rua Borba Gato, 785, Jardim América
Londrina, PR, Brazil Zip Code 86010-630
E-mail: ajtrufino@hotmail.com
Article received: July 17, 2013.
Article accepted: February 4, 2014.
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license