

Letters to the Editor - Year 2015 - Volume 30 -
Dermatofibrosarcoma protuberans
Dermatofibrossarcoma protuberante
Editor-in-Chief of the Brazilian Journal of Plastic Surgery
Dear Editor:
To begin with, I would like to congratulate the authors of the work entitled, "Extended resection in the treatment of dermatofibrosarcoma protuberans," published in the Brazilian Journal of Plastic Surgery (volume 29 number 3, pages 395-403, 2014). The study stands out owing to its clarity in methodology, discussion, and conclusion, as well as study sample and excellent results. However, it would be recommended to note that the main characteristic of this type of tumor is its high rate of local recurrence after surgical excision, especially for head and neck tumors.
History of trauma as the triggering factor is described in 10% to 20% of cases. Several reports, however, describe tumors developing in scars from a previous surgery, burns, and immunization for bacillus Calmette-Guerin, and a rapid growth during pregnancy, a fact attributed to progesterone receptors in tumor tissue1,2.
The indolent behavior of dermatofibrosarcoma and its imprecise characteristics often lead to a delay in its perception by patients, thus delaying its diagnosis. However, when the lesion has progressed, the tumor is not difficult to diagnose owing to its distinctive clinical appearance (Figure 1).

Figure 1. A patient with dermatofibrosarcoma protuberans in deltoid region, which was confused for a keloid lesion because of its location in the deltoid region and the appearance of the tumor.
Dermatofibrosarcoma tumor cells stain positive for CD34 and vimentin by immunohistochemistry, but not for CD44, S-100 protein, and factor XIIIA. On the other hand, dermatofibromas stain strongly positive for CD44 and stromelysine 3 (ST3) and negative for CD34 and vimentin (Figures 2 and 3)3.
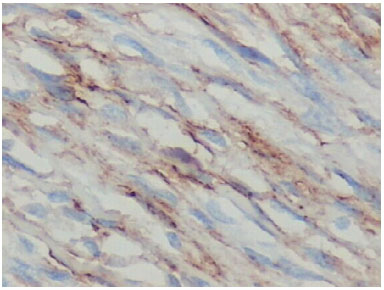
Figure 2. Immunohistochemical examination of histological sections of dermatofibrosarcoma protuberans with positive staining for CD34.
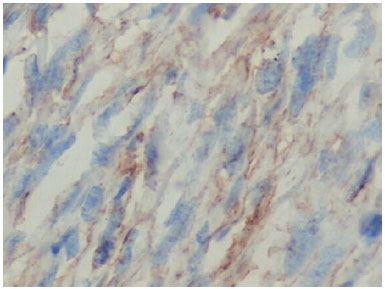
Figure 3. Immunohistochemical examination of histopathological sections of dermatofibrosarcoma protuberans with positive staining for vimentin.
The histological tumor margins are usually well beyond the macroscopic margins, because of horizontal dissemination of the tumor. Even apparently small tumors can, in fact, present distant projections interspersed in fat lobules, explaining the high rate of local recurrence. The surgical resection of the tumor must include the skin, subcutaneous tissue, and underlying fascia. Most recurrences are detected within 3 years after the primary excision, but these may appear 10 years after surgery. Owing to the high rate of local recurrence, revaluations are recommended every 6 months, with biopsies of suspected areas4.
The more frequent predisposing factors reported for recurrences are age older than 50 years, resection next to positive microscopic margins, fibrosarcomatotic variant of dermatofibrosarcoma, high mitotic rate, increased cellularity, and disease-free surgical margins less than 2 cm 5.
Finally, the only way to reduce the incidence of recurrences is by creating a wide initial excision of the tumor. However, for head and neck tumors, the margins tend to be reduced in order to preserve noble structures.
In conclusion, dermatofibrosarcoma protuberans is a locally infiltrative malignant tumor with a high recurrence rate but with a low potential for metastasis. The main differential diagnosis is with dermatofibroma. The possible presence of dermatofibrosarcoma protuberans should always be considered in cases of recurrence of injury with histopathological diagnosis of fibroma. The histopathological diagnosis of dermatofibrosarcoma protuberans may be difficult owing to the absence of nuclear atypia and low mitotic index, requiring an immunohistochemical analysis for a definitive diagnosis.
REFERENCES
1. Aoki T, Campaner AB, Ribeiro PAAG, Auge AP, Müller H, Kondo L, et al. Dermatofibrosarcoma protuberans em região inguinal: relato de caso. Rev Bras Ginecol Obstet. 2007;29(3):153-7. DOI: http://dx.doi.org/10.1590/S0100-72032007000300007
2. Cakir B, Misirlioğlu A, Gideroğlu K, Aköz T. Giant fibrosarcoma arising in dermatofibrosarcoma protuberans on the scalp during pregnancy. Dermatol Surg. 2003;29(3):297-9.
3. Kim HJ, Lee JY, Kim SH, Seo YJ, Lee JH, Park JK, et al. Stromelysin-3 expression in the differential diagnosis of dermatofibroma and dermatofibrosarcoma protuberans: comparison with factor XIIIa and CD34. Br J Dermatol. 2007;157(2):319-24. PMID: 17596171 DOI: http://dx.doi.org/10.1111/j.1365-2133.2007.08033.x
4. Kimmel Z, Ratner D, Kim JY, Wayne JD, Rademaker AW, Alam M. Peripheral excision margins for dermatofibrosarcoma protuberans: a meta-analysis of spatial data. Ann Surg Oncol. 2007;14(7):2113-20. DOI: http://dx.doi.org/10.1245/s10434-006-9233-3
5. Macedo JLS, Barbosa GS, Rosa SC. Dermatofibrosarcoma protuberante. Rev Bras Cir Plast. 2008;23(2):138-43.
1 Universidade de Brasília, Brasília, DF, Brazil
2. Escola Superior de Ciências da Saúde, Brasília, DF, Brazil
3. Hospital Regional da Asa Norte, Brasília, DF, Brazil
Institution: Hospital Regional da Asa Norte, Brasília, DF, Brazil.
Corresponding author:
Jefferson Lessa Soares de Macedo
SQS 213 Bloco H ap 104, Asa Sul
Brasília, DF, Brazil Zip Code 70292-080
E-mail: jlsmacedo@yahoo.com.br
Article received April 21, 2015.
Article accepted May 26, 2015.
Answer
Extended resection for treatment of dermatofibrosarcoma protuberans
José Carlos Ribeiro Resende Alves1,2,3,4; Rebeca Paohwa Liu da Fonseca2,3,4; Aloísio Ferreira da Silva Filho2,3,4; José de Souza Andrade Filho2,5; Izabella Costa Araújo4,6; Augusto César de Melo Almeida4,7,8; Nárlei Amarante Pereira2,3,4; Lívia Neffa2,4
Professor Dr. Ricardo Baroudi
Editor-in-Chief Brazilian Journal of Plastic Surgery
In the Letter to the Editor, we expressed our appreciation for the complimentary words of the authors. We present their observations and our rebuttal:
1. "It would be recommended to note that the main characteristic of this type of tumor is its high rate of local recurrence after surgical excision, especially in tumors of the head and neck."Answer: The Summary states that "it is a rare skin tumor and of intermediate malignancy, with low metastatic potential, but high recurrence rate after surgical treatment." The Introduction states, "On the basis of progressive behavior and recurrent neoplasm, the standard treatment of dermatofibrosarcoma protuberans (DFSP) has been, for decades, radical surgical resection with ample lateral margins of healthy tissue. The deep margin should include an anatomical structure not infiltrated by the tumor, such as fascia, muscle or external bone lamina."
2. They mention the indolent behavior of the tumor and the association with prior trauma.Answer: We state that (A) "history of previous trauma and association with immunosuppression were observed"; (B) "The clinical diagnosis of early forms is difficult (...); (C) "the development of the lesion may be prolonged (...)." It should be noted that prior trauma is common in sarcomas in general.
3. In the differential diagnosis, they refer to vimentin as an important immunohistochemical marker, which would be expressed by DFSP and would be negative in dermatofibroma. This is certainly a misunderstanding. Vimentin is expressed in dermatofibroma1. It cannot be used for the differential diagnosis of DFSP. It is a mesenchymal marker expressed by all fusocellular tumors. CD34, in turn, is expressed by a small group of neoplasms, namely DFSP, neurofibroma, and the rare solitary fibrous tumor, which is described more recently. CD102. is a useful marker of dermatofibroma. Dermatofibromas rarely express CD34. In the study in English3 cited by the authors, who recommended the use of vimentin, the word vimentin was not even mentioned. This error had already been stated in a study by the same group, written in 20084.Answer: We wrote that "factors that contribute to a worse prognosis include high mitotic index, age greater than 50 years, fibrosarcomatosis variant and compromised or exiguous excision margins," which are words to the same effect.
4. They state that "The more frequent predisposing factors reported for recurrences are age higher than 50 years, resection next to positive microscopic margin, fibrosarcomatosis variant of dermatofibrosarcoma, high mitotic rate, increased cellularity and disease free surgical margins lesser than two centimeter."
5. "The only way to reduce the incidence of recurrences is the wide initial excision of the tumor. However, for head and neck tumors, the margins tend to be reduced to preserve noble structures." They also state that "the main characteristic of this type of tumor is its high rate of local recurrence after surgical excision, especially in head and neck tumors."Answer: We frankly disagree with the relationship to smaller resection margins. Smaller margins explain higher recurrence rates in DFSP of the head and neck. We recommend, in any occasion, lateral margins of 3 cm and a deep margin, including an anatomical structure not infiltrated by the tumor, be it the fascia, muscle, or outer bone lamina. Local recurrences cause mutilative operations, besides facilitating the appearance of the fibrosarcomatosis variant.
In conclusion, "the objective of this retrospective study is to verify if a wide resection is a reliable method in the treatment of DFSP." The limited space did not allow considerations that do not relate to the surgical treatment of already diagnosed cases. If we had space, we could have dealt with the differential diagnosis with neurofibroma; the solitary fibrous tumor (expressing CD34, but histologically is a nodule with circumscribed growth and regular margins); fibrosarcoma; malignant histiocytoma; dermatofibroma; giant cell fibroblastoma; fibrous multinodular histiocytoma; dermatomiofibroma; and perineurioma.
REFERENCES
1. Sampurna R. Pathology of fibrous histiocytoma (dermatofibroma). Histopathology-India.net. Soft tissue pathology [Acesso 25 Ago 2015]. Disponível em: http://www.histopathology-india.net/dermatofibroma.htm
2. de Feraudy S, Mar N, McCalmont TH. Evaluation of CD10 and procollagen 1 in atypical fibroxantoma and dermatofibroma. Am J Surg Pathol. 2008;32(8):1111-22. DOI: http://dx.doi.org/10.1097/PAS.0b013e31816b8fce
3. Kim HJ, Lee JY, Kim SH, Seo YJ, Lee JH, Park JK, et al. Stromelysin-3 expression in the differential diagnosis of dermatofibroma and dermatofibrosarcoma protuberans: comparison with factor XIIIa and CD34. Br J Dermatol. 2007;157(2):319-24. PMID: 17596171 DOI: http://dx.doi.org/10.1111/j.1365-2133.2007.08033.x
4. Macedo JLS, Barbosa GS, Rosa SC. Dermatofibrossarcoma protuberante. Rev Bras Cir Plast. 2008;23(2):138-43.
1. Faculdade de Medicina da Universidade de Itaúna, Itaúna, MG, Brazil
2. Hospital Felício Rocho, Belo Horizonte, MG, Brazil
3. Instituto de Cirurgia Plástica Avançada, Belo Horizonte, MG, Brazil
4. Sociedade Brasileira de Cirurgia Plástica, Belo Horizonte, MG, Brazil
5. Faculdade de Ciências Médicas de Minas Gerais, Belo Horizonte, MG, Brazil
6. Biocor Instituto, Nova Lima, MG, Brazil
7. Hospital e Maternidade Terezinha de Jesus, Juiz de Fora, MG, Brazil
8. Hospital Monte Sinai, Juiz de Fora, MG, Brazil


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter