

Original Article - Year 2014 - Volume 29 -
Cutaneous melanoma: clinical, epidemiological, and anatomopathological aspects of a training center in Belo Horizonte
Melanoma Cutâneo: aspectos clínicos, epidemiológicos e anatomopatológicos de um centro de formação em Belo Horizonte
ABSTRACT
INTRODUCTION: Malignant cutaneous melanoma (MCM) comprises nearly 5% of all malignant cutaneous tumors and shows increasing incidence and a high mortality. The objective of this study is to review the clinical, epidemiological, and anatomopathological characteristics of MCM in patients treated at the plastic surgery and pathological anatomy services of a general hospital.
METHOD: Data corresponding to 47 lesions from 45 patients treated between 2011 and 2013 were reviewed. We analyzed the sex and age of patients, as well as the site and histopathological characteristics of the lesions.
RESULTS: A total of 24 patients were men and 21 were women. Their average age at the medical appointment was 61.9 years. Twenty-four neoplasias were in the extremities, 14 in the torso, and 9 in the face. Concerning histological diagnosis, 34.0% of the tumors were in situ melanoma and 66.0% were invasive melanoma. In the latter group, 14 lesions corresponded to the nodular melanoma type, 12 to the superficial spreading, three to the acral lentiginous, and two to the malignant lentigo melanoma type. Sentinel node biopsy was performed in 14 invasive melanomas, with 4 being positive. Among the lymphadenectomies performed, four were positive for metastasis. At diagnosis, four patients showed in-transit metastasis, whereas three patients had lymph node metastasis. Local tumor relapse was observed in two cases. Concerning tumor staging, 14 patients were in stage 0, 11 in stage I, 10 in stage II, and 10 in stage III.
CONCLUSION: The data from this study support the findings described in the literature. Early diagnosis and surgical treatment remain the best way to increase survival.
Keywords: Melanoma; Malignant melanoma; Epidemiology.
RESUMO
INTRODUÇÃO: O melanoma cutâneo maligno (MCM) constitui cerca de 5% dos tumores cutâneos malignos e apresenta crescente incidência e alta letalidade. O objetivo deste estudo é rever as características clínicas, epidemiológicas e anatomopatológicas do MCM em pacientes tratados nos serviços de Cirurgia Plástica e Anatomia Patológica de um hospital geral.
MÉTODO: Dados de 45 pacientes, correspondendo a 47 lesões, tratados entre 2011 e 2013, foram revisados. Estudou-se: gênero e idade dos pacientes, localização e características histopatológicas das lesões.
RESULTADOS: Vinte e quatro pacientes eram do gênero masculino e 21 do feminino. A média de idade à consulta foi de 61,9 anos. Vinte e quatro neoplasias localizaram-se nas extremidades, 14 acometeram o tronco e nove a face. Quanto ao diagnóstico histológico, 34,0% dos tumores consistiu-se em melanoma in situ e 66,0% em melanoma invasor. Neste grupo, 14 lesões correspondiam ao tipo nodular, 12 ao extensivo superficial, três ao acral lentiginoso e dois ao lentigo maligno. A biópsia de linfonodo sentinela foi realizada em 14 melanomas invasores, com positividade em quatro procedimentos. Dentre as linfadenectomias realizadas, quatro mostraram-se positivas para metástase. No momento do diagnóstico, quatro pacientes apresentavam metástase em trânsito e três com metástase linfonodal. Recidiva tumoral local foi verificada em dois casos. Em relação ao estadiamento, 14 pacientes encontravam-se no estádio 0, 11 no I, 10 no II e 10 no III.
CONCLUSÃO: Os dados deste estudo corroboram os achados da literatura. O diagnóstico e tratamento cirúrgico precoce permanecem o melhor caminho para o aumento da sobrevida.
Palavras-chave: Melanoma; Melanoma maligno; Epidemiologia.
Neoplasia occurs when a group of cells change their normal mechanisms of growth, and multiply regardless of tissue or organ structural and normal aspects1. Melanoma results from the transformation of a melanocyte, and therefore, may occur in any region where these cells are present2.
Malignant cutaneous melanoma (MCM) comprises nearly 5% of all malignant cutaneous tumors and shows increasing incidence and a high mortality 3. MCM is responsible for most skin cancer deaths4. For 2012, The Brazilian National Cancer Institute estimated that there were 3070 new cases in men, with 290 reported in the state of Minas Gerais, and 3060 cases in women, with 240 in Minas Gerais5.
The condition occurs more frequently in persons with Fitzpatrick phototypes I and II, a history of ultraviolet exposure, and a greater genetic predisposition, being mainly observed in adults from 20 to 50 years old. Women are more affected below 40 years of age, whereas men above 50 years6.
The survival rate of patients with MCM has been gradually increasing in recent years. For each decade, since 1940, a 10% increase in the 5-year survival rate was observed6. This may be due to early diagnosis and public health education programs, such as the mnemonic ABCDE (A: asymmetry of the lesion; B: borders, irregular; C: color, variegated; D: diameter >6 mm; and E: evolving of the lesion over time) and use of sun protectors. In the last 20 years, the proportion of early-stage tumors being removed was higher6. Even with the development of new therapies, early detection and prevention remain the key factors in decreasing the mortality of MCM5.
OBJECTIVE
The objective of this study is to review the clinical, epidemiological, and anatomopathological aspects of cutaneous melanoma, in patients treated at the plastic surgery and pathological anatomy departments in a general hospital.
METHOD
Data corresponding to 47 lesions from 45 patients treated from February 2011 to May 2013 were reviewed retrospectively, with the aim of determining the clinical, epidemiological, and anatomopathological aspects of cutaneous melanoma. The following characteristics were assessed: sex and age of patients, tumor staging and location, histological type and subtype, Breslow rate, and Clark level. Also, the results of sentinel lymph node (SLN) biopsies and lymphadenectomy were quantified. In-transit or local regional metastases, lymph node involvement, and multiple lesions or relapses were also analyzed.
Forty-four patients were subjected to surgery and subsequently followed in the postoperative period at the Plastic Surgery Clinic of the Felício Rocho Hospital (Belo Horizonte, MG, Brazil). One patient was treated in a different clinic at the same hospital; however, the surgical specimen was examined at the pathological anatomy department of that same institution. Postoperative monitoring during outpatient visits was performed with the following frequency: quarterly during the first two years, four-monthly in the third year, six-monthly in the fourth and fifth years, and annually from the sixth year onward. In cases of invasive melanoma, the patients were monitored every 6 months with determination of alkaline phosphatase, gamma-glutamyltransferase, and lactic dehydrogenase, as well as chest radiography.
All patients were submitted to the surgical resection of lesions. The resected tissues were sent for histological evaluation, including hematoxylin-eosin staining. The excisional biopsies to determine diagnosis were carried out with surgical margins of 1-2 mm. For surgical treatment of the primary lesion of the MCM, in the local excision performed to extend the lateral margins, we used parameters (see Table 1) according to the thickness of neoplasia7,8.
The deep margin was determined through insertion of all underlying subcutaneous tissue.
The data were entered in a Microsoft Office Excel spreadsheet (Microsoft, 2013). Graphics were created by using the software Microsoft Office PowerPoint (Microsoft, 2013).
The literature related to the topic was searched in the PubMed database with the following used as keywords and descriptors: melanoma, melanoma maligno, epidemiologia, malignant melanoma, and epidemiology.
RESULTS
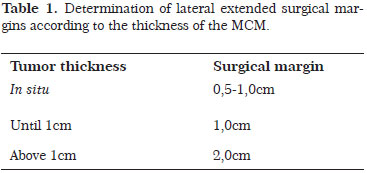
Twenty-four patients (53.3%) were men and 21 (46.7%) were women, with the male/female ratio being 1.14. (Figure 1).
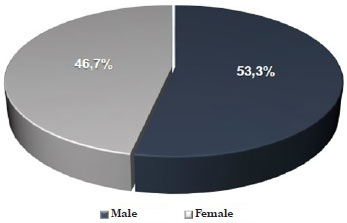
Figure 1. Distribution of patients with malignant cutaneous melanoma according to sex.
The age of patients at the time of surgery varied from 24 to 93 years, with an average age of 61.9 years. Nearly 70% of lesions occurred between the fifth and eight decades of life. The peak age of incidence occurred between 60 and 69 years, and 80 and 89 years (Figure 2).
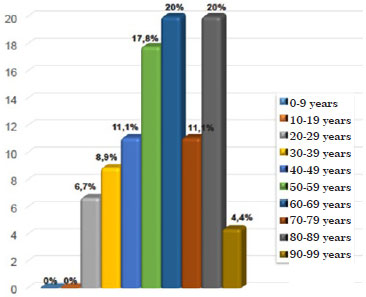
Figure 2. Distribution of patients with malignant cutaneous melanoma according to age group.
Among a total of 47 neoplasias, 24 (51.1%) affected the extremities, 14 (29.8%) affected the torso, and 9 (19.1%) affected the face (Figure 3).
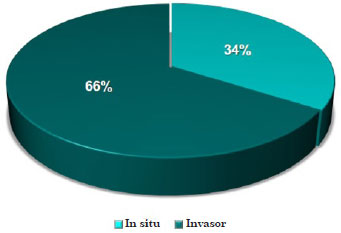
Figure 3. Distribution of patients with malignant cutaneous melanoma according to lesion site.
Concerning the histological diagnosis, 16 lesions (34.0%) comprised in situ melanoma and 31 (66.0%) invasive melanoma (Figure 4).
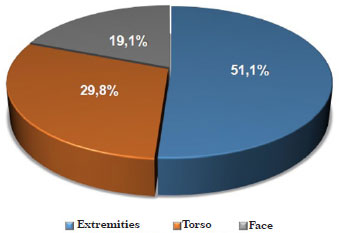
Figure 4. Distribution of lesions in patients with malignant cutaneous melanoma according to histological diagnosis.
The data of the patients with in situ melanoma (15 patients and 16 tumors) revealed a predominance of men (66.7%), with a male/female ratio of 2.0, and average age of 61.3 years. At the moment of diagnosis, 60% of women were in their fifth decade and 40% of men were in their sixth decade of life. The neoplasias were located in the extremities (43.8%), torso (37.5%), and face (18.7%) (Figure 5).
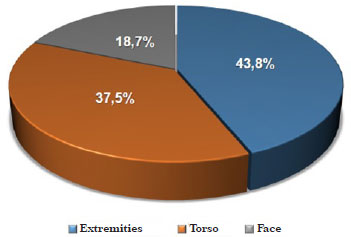
Figure 5. Distribution of lesions according to the location of in situ melanomas.
On the other hand, in patients with invasive melanoma (30 patients and 31 lesions), no significant sex preponderance was observed, with a male/female ratio of 0.88, and an average age of 62.2 years. Most women (56.1%) had their diagnosis between the fourth and sixth decades of life; whereas among men, 64.3% had their diagnosis between the sixth and eight decades of life. Concerning tumor location, 54.8% of neoplasias were found in the body extremities, 25.8% in the torso, and 19.4% in the face (Figure 6).
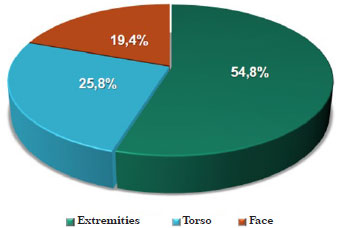
Figure 6. Distribution of lesions according to location of invasive melanomas.
Concerning histological subtypes, 14 tumors (45.2%) were nodular, 12 (38.7%) were superficial spreading, 3 (9.7%) were acral lentiginous, and 2 (6.4%) were malignant lentigo melanomas (Figure 7). The average age of patients with each of these subtypes was 57.6, 64.7, 65.3, and 87.5 years, respectively. Concerning the histopathological characteristics of the melanomas reported in the literature, the Breslow rate was reported to vary from 0.1 to 17 mm, with an average of 1.73 mm. One (3.3%) tumor was classified as Clark level I, 9 (30.0%) as level II, 3 (10.0%) as level III, 11 (36.7%) as level IV, and 6 (20.0%) as level V (Figure 8).
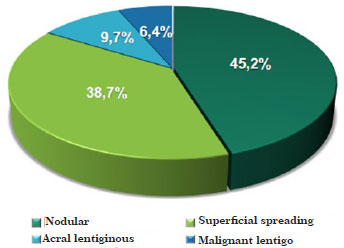
Figure 7. Distribution of lesions according to histological type of invasive melanomas.
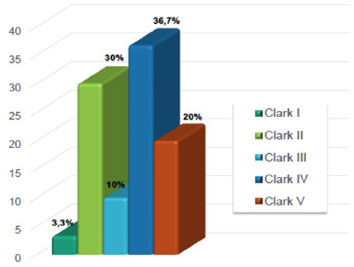
Figure 8. Distribution of lesions according to Clark levels of invasive melanomas.
SLN biopsy was indicated in case of an anatomopathological finding associated with a Breslow rate >0.75 mm, which corresponded to 14 of the 31 neoplasias (45.2%) of the invasive melanomas. In one case, characterized by the presence of an acral lentiginous melanoma, this procedure was performed in a lesion with a Breslow rate of 0.1 mm. Ten (71.4%) sentinel lymph nodes were negative, whereas four (28.6%) were positive for metastasis (Figure 9); among these, three (75.0%) required lymphadenectomy.
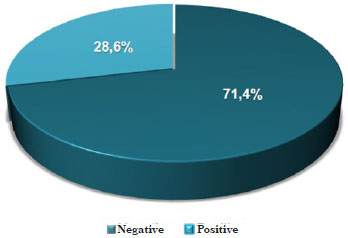
Figure 9. Distribution of sentinel lymph node biopsies according to the presence of metastases in invasive melanomas.
Seven lymphadenectomies were performed during the study period. Among these, four (57.1%) were performed because of a previous positive SLN. The remaining three (42.9%), which corresponded to 10% of the total of patients with invasive melanoma, were performed because of the involvement of the lymph node, and a previous SLN was not required. From the four lymphadenectomies performed after the positive SLN, one (25%) showed a positive result on the lymph nodes dissected. In the lymphadenectomies performed without requiring a previous SLN, all patients had a positive anatomicopathological result, thus corresponding to 100% of cases.
At diagnosis, four (13.3%) patients showed in-transit metastasis that were positive in the SLN, and three (10.0%) showed local regional metastases affecting the lymph node chains of the drainage site. Two (4.4%) patients had multiple lesions: one with a nodular melanoma in the scalp, and another in the posterior thorax; moreover, one patient had a superficial spreading melanoma at the right pectoralis, and another patient had in situ melanoma in the left leg. In two (4.4%) patients, a local tumor relapse was observed. One patient showed an in situ melanoma recurrence at the presternal region 4 months after the initial surgery, and one female patient developed an in situ melanoma at the site adjacent to the scar of the nodular melanoma resection in the left arm, which was performed 3 years before.
Concerning the staging of cutaneous melanoma, 14 patients (31.1%) were in stage 0, 11 (24.5%) in stage I, 10 (22.2%) in stage II, and 10 (22.2%) in stage III. None of the patients were found to be in stage IV (Figure 10).
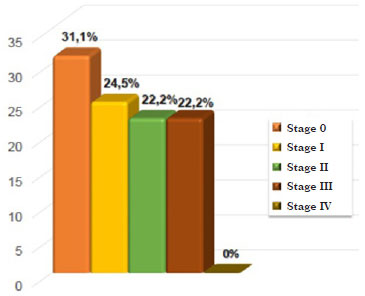
Figure 10. Distribution of patients according to the stage of malignant cutaneous melanoma.
DISCUSSION
MCM comprises nearly 5% of the malignant cutaneous tumors, and shows increasing incidence and a high mortality3.
This neoplasia was found to be predominant in white Caucasian men, and in people living close to the equator9-11.
Although each histological type has a predilection site in the body, the chest in men and the extremities in women remain the most involved areas in cases of neoplasia12, a fact that is supported in this article, as 48% of tumors in men were found in the torso and 72.8% of lesions found in women were in the extremities. Other relevant risk factors include socioeconomic level, sun exposure as a modifiable risk factor, and local latitude of the living area4,13.
In our study, 45.2% of tumors were of the nodular subtype, 38.7% were superficial spreading melanoma, 9.7% were acral lentiginous, and 6.4% were malignant lentigo melanomas; these data support the information described in the literature4,14, as superficial spreading melanoma comprises the most common subtype, with a frequency up to 70%, followed by the nodular type with 15% frequency, then the acral lentiginous type with 5-10%, and finally the malignant lentigo type with a frequency of 4-15%. Other variations were also described according to the tumor type: superficial spreading melanoma affects diverse anatomical sites and age group around the fourth decade of life, whereas acral lentiginous melanoma shows predominance in the palms of the hands, sole of the foot, and subungual regions, affecting patients at the sixth decade of life. Malignant lentigo melanoma, in turn, involves mainly the face, affecting the age group from the seventh decade of life. Finally, nodular melanoma may affect any location, being predominant between 40 and 50 years of age. With the exception of superficial spreading melanoma, which affects patients with an average age of 64 years, all the remaining melanoma subtypes described in the assessed articles were associated with age groups similar to those in this study3,15.
The Felício Rocho Hospital has a tertiary level of health care, and a comprehensive and multidisciplinary approach to the treatment of patients with MCM, owing to its specialist departments of plastic surgery, nuclear medicine, radiotherapy, and oncology. Therefore, it is a state reference hospital for the treatment of the condition. Thus, patients directed to the plastic surgery clinic for the evaluation of skin lesions have a diverse profile when compared with the general community; that is, their lesions look atypical and, therefore, are difficult to diagnose. Nodular melanoma is included among these lesions, in which the visual characteristics do not correspond to the requirements described in the ABCDE mnemonic, justifying the striking differences found among the nodular melanomas in the present case series.
In 1977, Donald Morton proposed the SLN biopsy for the first time as an essential procedure to assess patients with invasive melanoma, with the aim of preventing unnecessary lymphadenectomies16. In the present article, SLN was indicated as a result of an anatomicopathological finding corresponding to a Breslow rate >0.75mm, which corresponded to 45.2% of neoplasias whose histological diagnosis revealed an invasive melanoma. Moreover, 28.6% of the lymph nodes were positive for metastasis, a result very similar to a study from 1999 that demonstrated a rate of 26% of positive sentinel lymph nodes16,17.
We observed a close relation between tumor resection margins and local recurrence of the MCM. The local recurrence, characterized by the development of a new lesion with a distance up to 2 cm of the initial scar, was strongly associated with excisions performed with narrower margins. The determination of the margin to be extended depends on the tumor thickness, according to the guidelines from the Brazilian Melanoma Group and the Brazilian Ministry of Health, and its correct performance is of utmost importance for the successful treatment of this condition7,8. The presence of only two (4.4%) local relapses in this series of cases demonstrated the relevance of using those criteria in the management of MCM.
A gradual increase in the diagnosis of melanoma in all of its histological subtypes has been observed in the last few years4,13. This increase is in part due to improved education of the population concerning the disease, and in part due to the increase in the absolute value of skin neoplasias18. In the United States, an increase of 6.4:100,000 to 16:100,000 cases of MCM were observed between 1973 and 1996, which is equivalent to an estimated increase of 120%, despite an expected annual increase of 4.3%19. It is assumed that 10-21% of MCM cases in the United States are underestimated every year owing to the lack of notifications20.
MCM has a higher mortality rate compared with other skin conditions, being responsible for three-fourth of all deaths20. Currently, a 40% increase in the mortality rate is observed, with 50% occurring in men and 20% in women. A relevant factor for the higher mortality among males may be the higher tendency for the appearance of lesions in the chest in males, which is, in itself, considered a criterion of a worst diagnosis12.
CONCLUSION
This study confirms the global tendency of an increase in the incidence of MCM, earlier diagnosis, and correct indication for the use of lymphoscintigraphy, SLN, and lymphadenectomy.
The nodular melanoma subtype showed diverse prevalence when compared with the prevalence described in the literature, according to the epidemiological profile of the patients in the present work.
Finally, this article underlines that the presence of an adequate hospital infrastructure, characterized by appropriate services of pathological anatomy and nuclear medicine, and experienced surgical teams, is fundamental for the successful treatment of MCM.
REFERENCES
1. Nussbaum LR, Mclnnes RR, Williard HF. Thompson& Thompson: genética médica. Rio de Janeiro: 7 ed. Elsevier; 2008. p. 640.
2. Grabb and Smith's plastic surgery. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2007. p.960.
3. Zacharias DPM, Santos IDAO. Melanoma cutâneo. In: Mélega JM. Cirurgia plástica fundamentos e arte: princípios gerais. Rio de Janeiro: Guanabara Koogan; 2009. p.361-370.
4. Chen ST, Geller AC, Tsao H. Update on the epidemiology of melanoma. Curr Derm Rep. 2013;2(1):24-34.
5. Instituto Nacional de Câncer José Alencar Gomes da Silva. Coordenação Geral de Ações Estratégicas. Coordenação de Prevenção e Vigilância. Estimativa 2012: incidência de câncer no Brasil. Rio de Janeiro: Inca, 2011. p.118.
6. Pereira, SM. Melanoma: introdução e epidemiologia. Disponível em: <http://www.gbm.org.br/GBM>.
7. Grupo Brasileiro de Melanoma. Tratamento do melanoma cutâneo. Disponível em: <http://www.gbm.org.br/GBM>.
8. Brasil. Ministério da Saúde. Diretrizes diagnósticas e terapêuticas do melanoma maligno cutâneo. Portaria no. 357, de 8 de abril de 2013.
9. Swerdlow AJ. International trends in cutaneous melanoma. Ann N Y Acad Sci. 1990;609:235-251.
10. Eide MJ, Weinstock MA. Association of UV index, latitude and melanoma incidence in nonwhite populations - US Surveillance, Epidemiology, and End Results (SEER) Program, 1992 to 2001. Arch Dermatol. 2005;141(4):477-481.
11. Chan V, Thompson I, Whitney D, Switzer M, Anderson AD, Smits S. Migration and melanoma incidence rates among Washington state counties. Melanoma Res. 2013;23(4):312-320.
12. Elder DE. Skin cancer. Melanoma and other specific nonmelanoma skin cancers. Cancer. 1995;75(1 Suppl):245-256.
13. Ries LAG, Kosary CL, Hankey BF, et al, editors. SEER Cancer Statistics Review, 1973-1994. Bethesda: National Cancer Institute, NIH Publication 1997;97(2789):305-318.
14. Schaffer JV, Rigel DS, Kopf AW, Bolognia JL. Cutaneous melanoma - past, present, and future. J Am Acad Dermatol. 2004;51(1):S65-9.
15. Sober AJ, Haluska FG. Skin cancer. Hamilton: B.C. Decker Incorporated, 2001. 350 p.
16. Morton DL, Wen D, Wong JH, Economou JS, Cagle LA, Storm FK, Foshag LJ, Cochran AJ. Technical details of intraoperative lymphatic mapping for early stage melanoma. Arch Surg. 1992;127(4):392-399.
17. Morton DL, Chan AD. Current status of intraoperative lymphatic mapping and sentinel lymphadenectomy for melanoma: is it standard of care? J Am Coll Surg. 1999;189(2):214-223.
18. Hall HI, Miller DR, Rogers JD, Bewerse B. Update on the incidence and mortality from melanoma in the United States. J Am Acad Dermatol. 1999 Jan;40(1):35-42.
19. Karagas MA, Thomas DB, Roth GJ, Johnson LK, Weiss NS. The effects of changes in health care delivery on the reported incidence of cutaneous melanoma in western Washington State. Am J Epidemiol. 1991;133(1):58-62.
20. Weinstock MA. Death from skin cancer among the elderly: epidemiologic patterns. Arch Dermatol. 1997;133(10):1207-1209.
1. Doctor - Aspirant Member in Training of the Brazilian Society of Plastic Surgery (SBCP); Resident Doctor at the Plastic Surgery Service of the Felício Rocho Hospital, Belo Horizonte, MG, Brazil
2. Doctor - Plastic Surgeon; Specialist Member of the SBCP; Member of the Clinical Staff at the Biocor Institute, Belo Horizonte, MG, Brazil
3. Doctor - Plastic Surgeon; Specialist Member of the SBCP; Member of the Clinical Staff at the Biocor Institute and Vera Cruz Hospital, Belo Horizonte, MG, Brazil; Member of the Clinical Staff at the Hospital Unimed - Unidade Betim, Betim, MG, Brazil
4. Doctor - Aspirant Member in Training of the SBCP; Resident Doctor at the Plastic Surgery Service of the Felício Rocho Hospital, Belo Horizonte, MG, Brazil
5. Doctor - Aspirant Member in Training of the SBCP; Resident Doctor at the Plastic Surgery Service of the Felício Rocho Hospital, Belo Horizonte, MG, Brazil
6. Doctor - Plastic Surgeon; Full Member of the SBCP; Member of the Clinical Staff at the Plastic Surgery Service of the Felício Rocho Hospital and Institute for Advanced Plastic Surgery, Belo Horizonte, MG, Brazil
7. Doctor - Plastic Surgeon; Specialist Member of the SBCP; Member of the Clinical Staff at the Plastic Surgery Service of the Felício Rocho Hospital and Institute for Advanced Plastic Surgery, Belo Horizonte, MG, Brazil
8. Doctor - Plastic Surgeon; Full Member of the SBCP; Member of the Clinical Staff at the Plastic Surgery Service of the Felício Rocho Hospital and Institute for Advanced Plastic Surgery, Belo Horizonte, MG, Brazil
Institution: Hospital Felício Rocho, Belo Horizonte, MG, Brazil
Corresponding author:
Clênio Martins de Souza Coelho
Rua Ouro Preto, 1707/701 - Bairro Santo Agostinho
Belo Horizonte, MG, Brasil CEP: 30170-041
E-mail: cleniomed@yahoo.com.br
Article submitted: July 9, 2014.
Article accepted: November 14, 2014.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter