ISSN Online: 2177-1235 | ISSN Print: 1983-5175
Changes in the orofacial myofunctional system after treatment for facial trauma: a critical review of the literature
Sistema miofuncional orofacial e trauma de face: revisão crítica da literatura
ABSTRACT
INTRODUCTION: This qualitative literature review aims to highlight international scientific publications selected from the PubMed database that describe the changes in the function of the orofacial myofunctional system after facial trauma and the associated treatment outcomes.
METHODS: Studies published in English between 2005 and 2011 and including individuals of all age groups were included in this review. Publications that were not open access, studies appearing more than once because of overlapping keywords, case studies, literature reviews, letters to the editor, and studies that were not directly related to the subject were excluded.
RESULTS: A total of 831 studies were identified, 14 of which fulfilled the established criteria. Assessment of jaw function was the most frequent evaluation performed in the included studies, followed by the analysis of treatments. The incidence of condylar fractures was higher than that of mandibular angle fractures. The majority of cases were managed by surgery combined with conservative treatment, followed by surgery alone and conservative treatment alone. Adult men exhibited a higher incidence of facial trauma. Few studies included children or control groups. Further assessment of jaw and clinical functions before and after surgery revealed the following findings. The bite force and occlusal contact area improved after treatment, whereas mandibular asymmetry persisted even after surgery. The maximum mouth opening returned to normal after treatment, although the range of mouth opening was lower in patients with facial trauma than in controls. Persistent mobility in the mandibular teeth and pain were observed even after treatment. Myofunctional therapy resulted in an overall improvement in jaw function.
CONCLUSIONS: Although the number of studies on facial trauma is increasing, few studies address the use and benefits of orofacial myofunctional therapy in this field. Further studies on orofacial myofunctional therapy combined with surgery and/or conservative treatment for facial trauma are necessary.
Keywords:
Facial trauma; Myofunctional Therapy; Rehabilitation; Speech Therapy; Stomatognathic System.
RESUMO
INTRODUÇÃO: Esta revisão qualitativa da literatura levantou publicações científicas internacionais sobre a funcionalidade do sistema miofuncional orofacial nos traumas faciais, por meio da base de dados PubMed.
MÉTODO: O levantamento realizado limitou-se a seres humanos, de qualquer faixa etária, no idioma inglês, entre os anos de 2005 e 2011. As publicações sem acesso completo, repetidas por sobreposição das palavras chave, estudos de caso, revisões de literatura, cartas ao editor e as não relacionadas diretamente ao tema foram excluídas.
RESULTADOS: Foram identificados 831 estudos, sendo 14 dentro dos critérios estabelecidos. Notou-se que a avaliação mais frequente foi a da função mandibular e depois análise de tratamentos; ocorreu mais fratura no côndilo que ângulo mandibular; utilizou-se mais tratamento cirúrgico juntamente com o conservador, seguido pelo somente cirúrgico e finalmente somente conservador; a maior incidência de traumas faciais foi em adultos do sexo masculino; poucas pesquisas foram realizadas com crianças e grupo-controle; utilizaram-se mais avaliações da função mandibular e clínicas, na maioria pré e pós-cirurgia; a força de mordida e a área oclusal apresentaram melhora pós-tratamento, no entanto a assimetria mandibular permaneceu; os valores de abertura máxima da boca atingiram a normalidade, porém inferiores ao grupo-controle; houve persistência de alterações na mobilidade mandibular e dor, mesmo após o tratamento; e a terapia miofuncional melhorou o quadro de alterações.
CONCLUSÃO: É necessário mais publicações sobre o tratamento fonoaudiológico baseado na abordagem miofuncional orofacial nos traumas faciais.
Palavras-chave:
Lesões Faciais; Terapia Miofuncional; Reabilitação; Fonoaudiologia; Sistema Estomatognático.
INTRODUCTION
Facial trauma involves injuries to the facial soft tissues and bones, and, in cases of extensive trauma, the brain, eyes, sinuses, and teeth. The epidemiology of this form of trauma is diverse and varies with type, severity, and cause of the injury1.
The primary cause of maxillofacial fractures is road accidents2,3. However, increased interpersonal violence1 and the use of firearm bullets also lead to an increased incidence of facial trauma.
The effects of facial trauma may be reversible or irreversible and may lead to emotional, functional, and esthetic impairments. The incidence of facial fractures is higher in men than in women. However, over the past few decades, the incidence has increased in women aged below 40 years5-7, with a lower incidence in children and individuals older than 40 years8,9.
Changes in the organs of articulation after facial trauma are a topic of great interest in the field of speech and language therapy. Such changes interfere with stomatognathic functions such as breathing, speaking, chewing, and swallowing. Speech therapy based the changes in the function of the orofacial myofunctional system after facial trauma is an important complementary treatment because it helps in restoring normal oral functions and decreases the risk of hypomobility and prevents the progression of possible sequelae10-15.
In the abovementioned context, this literature review was performed to analyze scientific publications describing changes in the function of the orofacial myofunctional system after facial trauma, specifically in the maxilla and mandible, and the associated treatment outcomes.
METHODS
This qualitative literature review included articles selected from the PubMed database using the following keywords: "facial injuries and oral muscle," "facial injuries and oral structure," "facial injuries and speech," "facial injuries and voice," "facial injuries and chewing," "facial injuries and mastication," "facial injuries and deglutition," "facial injuries and swallowing," "facial injuries and breathing," "facial injuries and myofunctional system," and "facial injuries and oral function." All studies published in English between 2005 and 2011 and including all age groups were included.
To establish the principles of the research method employed, the precepts of the Cochrane Handbook16 were followed with regard to formulation of the question, location, study selection, and critical evaluation.
For appropriate study selection, it was first necessary to achieve compatibility among the researchers. The articles were independently searched in the database by the authors, with the aim to minimize possible citation loss. Studies published in languages other than English were excluded. Studies without full text access (obtained from the CAPES Journal Portal); those appearing multiple times because of overlapping keywords; full articles submitted as case studies, literature reviews, or letters to the editor; and studies that were not directly related to the subject (studies related to surgical technique, fractures in regions of the face other than the maxilla and/or mandible, or changes in sensitivity and animal studies) were also excluded. All phases of the study were independently conducted by the researchers. In case of disagreement, studies were included on the basis of a final consensus. This study was not a simple blind search.
The study selection flowchart is illustrated in Figure 1.

Figure 1. Study selection flowchart
After the bibliographic survey and study selection, the manuscripts were analyzed with regard to the aims, number, and gender of the participants, age groups, evaluated parameters, treatment controls, and results. This analysis is described in subsequent session.
RESULTS
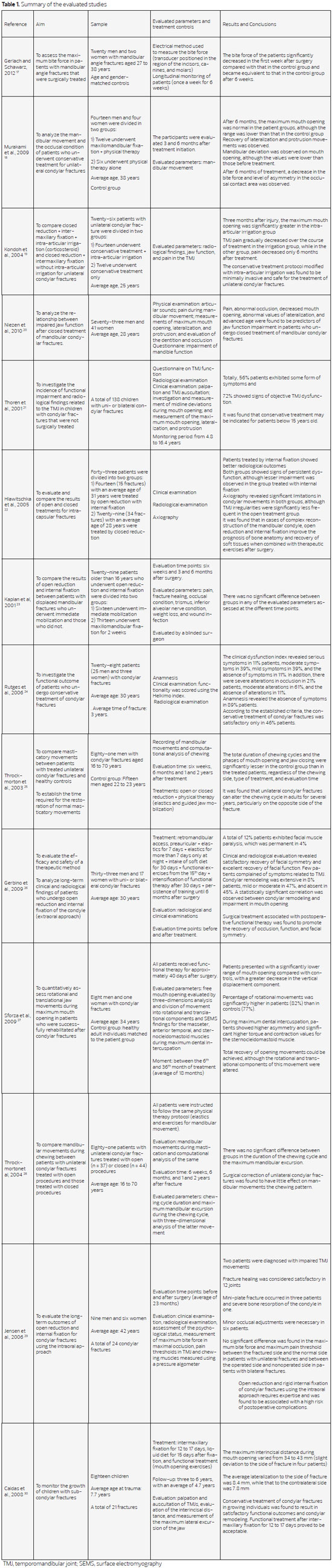
The results of the literature search used in this study are briefly described in Table 1.
DISCUSSION
The findings of this literature review indicated that most of the studies aimed at the evaluation of mandibular function17,18,21,24,25,27,28-30 and the analysis of treatment outcomes19,22,23,26 and facial trauma-related complaints (poor or moderate occluded area, decreased maximum mouth opening, asymmetric lateralization, mandibular deviation, and persistent pain)20. Most studies included patients with condylar fractures18-21-29, followed by mandibular angle17 and subcondylar fractures30.
With regard to the treatment approach (surgical or conservative), five studies17,19,20,26,29 involved surgery, three18,21,24 involved conservative treatment, and six22,23,25,27,28,30 involved a combination of surgical and conservative treatments.
In general, these studies were performed in adults17-20,22-29, with a higher incidence of facial trauma in men17,18,20,24-27,29,30. Only two studies included children21,30. Most studies did not use control groups19-23,26,28-30. Studies with control groups allow for direct comparison of results and their application in the clinical setting and decrease potential biases that may lead to inaccurate interpretation of the results.
Most of the studies evaluated mandibular function19-21,23,28-30 and performed clinical examinations20-23,26,29,30, followed by radiological19,21,22,26,29, physical19,20, psyschological29, and axiographic22 assessments. As in most of the surveys, the evaluation time points corresponded to the pre- and postoperative periods, with 6 weeks23,28 and 16.4 years21 as the minimum and maximum follow-up periods, respectively, after fracture.
For better discussion and characterization of the findings and conclusions related to orofacial myofunctional characteristics found in the articles that were fundamental for this study, specific aspects of greater relevance were addressed separately and were divided for didactic purposes into aspects related to the bite force and occlusal contact area, aspects related to static and dynamic occlusion and jaw mobility, and aspects related to pain.
With regard to the bite force and occlusal contact area, three studies showed that the bite force17,18,26 improved after treatment and over time, two showed an improved occlusal contact area18,26, and three18,21,27 reported the presence of asymmetry in these parameters after fracture correction.
With regard to dynamic occlusion, the maximum mouth opening returned to normal in some studies18,24,27,30. However, some of these studies18,27,30 reported a lower range of mouth opening in patients than in controls. In one study20, the maximum mouth opening was not restored to normal.
With regard to jaw mobility, one study18 observed a limited recovery in jaw mobility. In four studies20-22,30, alterations in jaw mobility persisted in the long term.
The persistence of pain despite treatment was reported in several studies20,22,29, and only one study19 reported a decrease in pain.
In several studies22,25,27,28,30, jaw function improved when facial fractures were treated in combination with orofacial myofunctional therapy, and even after surgical and/or conservative treatment, changes in asymmetry and jaw mobility were still observed. The combination of a myofunctional approach with surgery and/or conservative treatment for jaw fractures can improve the overall jaw function.
CONCLUSIONS
Although the number of studies on facial trauma is increasing, few studies address the use and benefits of orofacial myofunctional therapy in this field. Although an increasing number of studies in international databases are emphasizing on the use of orofacial myofunctional therapy in combination with surgery and/or conservative treatment for facial trauma, these are inadequate and provide little scientific evidence. More specific studies are required to demonstrate the benefits of this therapy and define the methodologies that should be applied by skilled professionals.
REFERENCES
1. Carvalho TB, Candian LR, Marques CG, Piatto VB, Maniglia JV, Molina FD. Six years of facial trauma care: an epidemiological analysis of 355 cases. Braz J Otorhinolaryngol. 2010;76(5):565-74.
2. Chandra Shekar BR, Reddy C. A five-year retrospective statistical analysis of maxillofacial injuries in patients admitted and treated at two hospitals of Mysore city. Indian J Dent Res. 2008;19(4):304-8.
3. Hussaini HM, Rahman NA, Rahman RA, Nor GM, Ai Idrus SM, Ramli R. Maxillofacial trauma with emphasis on soft-tissue injuries in Malaysia. Int J Oral Maxillofac Surg. 2007;36(9):797-801.
4. Bianchini EM, Moraes RB, Nazario DA, Luz JG. Terapêutica interdisciplinar para fratura cominutiva de côndilo por projétil de arma de fogo - enfoque miofuncional. Rev. CEFAC. 2010;12(5):881-8.
5. Martini MZ, Takahashi A, Oliveira Neto, HG, Carvalho Júnior JP, Cúrcio R, Shinohara EH. Epidemiology of mandibular fractures treated in a brazilian level I trauma public hospital in the city of São Paulo, Brazil. Braz Dent J. 2006;17:243-8.
6. Montovani JC, Campos MP, Gomes MA, Moraes VR, Ferreira FD, Nogueira EA. Etiologia e incidência das fraturas faciais em adultos e crianças: experiência em 513 casos. Braz J Otorhinolaryngol. 2006;72:235-41.
7. Macedo JL, Camargo LM, Almeida PF, Rosa SC. Perfil epidemiológico do trauma de face dos pacientes atendidos no pronto-socorro de um hospital público. Rev Col Bras Cir. 2008;35:9-13.
8. Bakardjiev A, Pechalova P. Maxillofacial fractures in Southern Bulgaria - a retrospective study of 1706 cases. J Craniomaxillofac Surg. 2007;35(3):147-50.
9. Ogunlewe MO, James O, Ladeinde AL, Adeyemo WL. Pattern of paediatric maxillofacial fractures in Lagos, Nigeria. Int J Paediatr Dent. 2006;16:358-62.
10. Maliska MC; Lima Júnior SM; Gil JN. Analysis of 185 maxillofacial fractures in the state of Santa Catarina, Brazil. Braz Oral Res.2009;23(3):268-74.
11. Oliveira DM, Vasconcellos RJ, Laureano FJ, Cypriano RV. Fracture of the coronoid and pterygoid processes by firearms: case report. Braz Dent J. 2007;18(2):168-70.
12. Sakae EK, Barroso, MV, Hiraki PY, Moura T, D'Agostinho L. Tratamento conservador de fratura cominuta de mandíbula ocasionada por arma de fogo: relato de caso. Rev Soc Bras Cir Craniomaxilofac. 2008;11(3):16-16.
13. Bianchini EM. Ajuda fonoaudiológica. In: Bianchini EMG. organizadora. Articulação temporomandibular: implicações, limitações e possibilidades fonoaudiológicas. 2a ed. Carapicuiba: Pró-Fono. 2010; p.321-61.
14. Marzotto SR, Bianchini EMG. Anquilose temporomandibular bilateral: aspectos fonoaudiológicos e procedimentos clínicos. Rev CEFAC 2007;9(3):358-66.
15. Laverick S, Patel N, Jones DC. Maxillofacial trauma and the role of alcohol. Br J Oral Maxillofac Surg. 2008;46:542-6.
16. The Cochrane Collaboration.Cochrane Handbook for Systematic Reviews of Intervention. 2011.
17. Gerlach KL, Schwarz A. Bite forces in patients after treatment of mandibular angle fractures with miniplate osteosynthesis according to Champy. J. Oral Maxillofac. Surg. 2002;31:345-348.
18. Murakami K, Yamamoto K, Sugiura T, Yamanaka Y, Kirita T. Changes in mandibular movement and oclusal condition after conservative treatment for condilar fractures. J. Oral Maxillofac. Surg. 2009;67:83-91.
19. Kondoh T, Hamada Y, Kamei K, Kobayakawa M, Horie A, Iino M, et al, Seto K.Comparative study of intra-articular irrigation and conticosteroid injection versus closed reduction with intermaxillary fixation for the management of mandibular condyle fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004;98:651-6.
20. Niezen ET, Bos RR, Bont LG, Stegenga B. Complaints related to mandibular function impairment after closed treatment of fractures of the mandibular condyle. J. Oral Maxillofac. Surg. 2010;39:660-665.
21. Thore'n T, Hallikainen D, Iizuka T, Lindqvist C. Condylar process fractures in children: a follow-up study of fractures with total dislocation of the condyle from the glenoid fossa. J Oral Maxillofac Surg. 2001;768-73.
22. Hlawitschka M, Loukota R, Eckelt U. Functional and radiological results of open and closed treatment of intracapsular (diacapitular) condylar fractures of the mandible. J. Oral Maxillofac. Surg. 2005;34:597-604.
23. Kaplan BA, Hoard MA, Park SS. Immediate mobilization following fixation of mandible fractures: a prospective, randomized study. Laryngoscope. 2001;111(9):1520-4.
24. Rutges JP, Kruizinga EH, Rosenberg A, Koole R. Functional results after conservative treatment of fractures of the mandibular condyle. Br J Oral Maxillofac Surg. 2007 Jan;45(1):30-4.
25. Throckmorton GS, Ellis E 3rd, Hayasaki H. Jaw kinematics during mastication after unilateral fractures of the mandibular condylar process. Am J Orthod Dentofacial Orthop. 2003;124(6):695-707.
26. Gerbino G, Boffano P, Tosco P, Berrone S. Long-term clinical and radiological outcomes for the surgical treatment of mandibular condylar fractures. J Oral Maxillofac Surg. 2009;67:1009-14.
27. Sforza C, Tartaglia GM, Lovecchio N, Ugolini A, Monteverdi R, Gianni AB. Mandibular movements at maximum mouth opening and EMG activity of masticatory and neck muscles in patients rehabilitated after a mandibular condyle fracture. J Craniomaxillofac Surg. 2009 Sep;37(6):327-33.
28. Throckmorton GS, Ellis III E, Hayasaki H. Masticatory motion after surgical or nonsurgical treatment for unilateral fractures of the mandibular condylar process. J Oral Maxillofac Surg. 2004;62:127-38.
29. Jensen T, Jensen J, Norbolt SE, Dabt M, Lenk-Hansen L, Svensson P. Open reduction and rigid internal fixation of mandibular condilar fractures by an intraoral approach: a long-term follow-up sudy of 15 patients. J Oral Maxillofac Surg. 2006;64(12):1771-9.
30. Caldas IM, Magalhães T, Afonso A, Matos E. Orofacial damage resulting from road accidents. Dent Traumatol. 2008;24(4):410-5
1 - Specialist in Speech Therapy and Facial Functions - Support Unit of Speech Therapy, Central Institute of Hospital das Clínicas, Faculty of Medicine, University of São Paulo - Speech Therapist
2 - Doctor of Science - Scientific researcher at the Laboratory of Medical Investigation - Rehabilitation Sciences - Hospital das Clínicas, Faculty of Medicine, University of São Paulo
3 - Doctor of Science - Speech Therapist at the Department of Physical Therapy, Speech Therapy and Occupational Therapy, Faculty of Medicine, University of São Paulo
4 - Professor - Senior lecturer at the Department of Physical Therapy, Speech Therapy and Occupational Therapy, Faculty of Medicine, University of São Paulo
Institutions: Department of Physical Therapy, Speech Therapy and Occupational Therapy, Faculty of Medicine, University of São Paulo and Hospital das Clínicas.
Corresponding author:
Prof. Dr. Claudia Regina Furquim de Andrade
Rua Cipotânea, 51- University campus
São Paulo/SP, ZIP: 05360-160
Telephone: 30918406/30917714
E-mail: clauan@usp.br
Article received: June 19, 2012
Article accepted: December 24, 2012
 All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license
All scientific articles published at www.rbcp.org.br are licensed under a Creative Commons license