

Original Article - Year 2014 - Volume 29 - Issue 1
Parenthesis-shaped deformity of the alar cartilages: a retrospective analysis of 49 cases of treatment by caudal rotation of the lateral crura
Deformidade das cartilagens alares em forma de parênteses: tratamento pela rotação caudal das crura laterais, experiência de 49 casos
ABSTRACT
INTRODUCTION: Alar cartilage cephalic malposition was first described as a parenthesis-shaped deformity by Sheen. The aim of this study was to analyze the results of treatment by caudal rotation of the lateral crus for this deformity.
METHOD: A retrospective study was conducted with 49 cases, operated on between July 2011 and January 2013 at the 2nd Infirmary of the Santa Casa da Misericórdia in Rio de Janeiro and at a private clinic.
RESULTS: Most of the patients (76% of cases) had a severe form of this deformity. All others presented with a moderate form (24% of cases). Fifty seven percent of the patients (57%) had a "boxy tip" and an initial alar pinching, 61% showed alar retraction and 8%, external valve collapse. The "boxy tip" was corrected in 100% of cases; initial alar retraction, 97%; alar pinching, 96%; and external valve collapse, 100%. The 3 cases of unilateral relapse were corrected by the same technique during a second rhinoplasty.
CONCLUSIONS: This study shows that caudal rotation of the lateral crus can treat the deformity described by Sheen with a small number of relapses and without serious complications.
Keywords: Plastic Surgery; Rhinoplasty; Nasal Cartilages; Structural Collapse; Postoperative Complications.
RESUMO
INTRODUÇÃO: Sheen descreveu pela primeira vez uma má posição cefálica das cartilagens alares como a «deformidade em forma de parênteses». O objetivo deste trabalho foi analisar os resultados do tratamento desta deformidade pela rotação caudal da cruz lateral.
MÉTODO: Foi realizado estudo retrospectivo, com 49 casos, operados entre Julho 2011 e Janeiro 2013 na 2ª Enfermaria da Santa Casa da Misericórdia do Rio de Janeiro e em uma clínica particular.
RESULTADOS: A maioria dos pacientes (76% dos casos) tinha a forma severa desta deformidade, os outros apresentavam uma forma moderada (24% dos casos). Cinquenta e sete por cento dos pacientes tinham um "boxy tip" e um piçamento alar inicial, 61% apresentavam uma retração alar e 8% um colapso da válvula externa. O «boxy tip" foi corrigido em 100% dos casos, a retração alar inicial foi corrigida em 97% dos casos, o pinçamento alar em 96% e o colapso da válvula externa foi tratado em 100% dos casos. Os 3 casos de recidiva unilateral foram corrigidos pela mesma técnica durante uma segunda rinoplastia.
CONCLUSÕES: Este trabalho mostra que a rotação caudal da cruz lateral permite tratar a deformidade descrita por Sheen com poucas recidivas e sem complicações graves.
Palavras-chave: Cirurgia Plástica; Rinoplastia; Cartilagens Nasais; Colapso Estrutural; Complicações Pós-Operatórias.
Cephalic-positioned alar cartilage was first described by Sheen1. According to Sheen, this is alar cartilage with a lateral crura oriented towards the medial instead of the lateral canthus of the eyelid1. Constantian2 described this anatomical variation as a "malposition of the alar cartilage", in which the lateral crus is rotated in the anterior direction and moves away from the nostril plane at an angle of 45º or higher. Hamra3 defines such variation as a "malrotated lateral crus" and presents a technique to correct it to the "correct anatomical position". According to Peck4 and Rees5, such "malposition" of the alar cartilage has received little attention, although it is a common anatomical variation. In a study of 50 consecutive cases by Daniel6, the author defines "cephalic malposition of the lateral crus" as an offset of 7mm or more from the center of the alar rim. Clinically, the alar rim appears pinched and the tip squared (boxy tip), an appearance described as a "parenthesis-shaped deformity"7. Hamra3 claims that, considering the high frequency of this anatomical condition, it would be more appropriate to name it "cephalic-positioned" alar cartilage than "malpositioned".
The cephalic position of the alar cartilage leaves the ala without effective cartilaginous support7,8. It is important to identify this variation in the position of the alar cartilage during the preoperative period and surgery, since resection of excess malpositioned alar cartilage could cause weakening of the lateral crura and collapse under the force of cephalic traction due to scar retraction7. Without proper treatment, alar retraction and pinching ("notching"), as well as external valve collapse due to lack of cartilaginous support, may develop during the late postoperative period8,9.
OBJECTIVES
This study aimed to describe the alar cartilage caudal rotation technique based on Sheen's technique and present the results in 49 operated cases.
METHOD
A retrospective study was conducted on 49 cases of patients with "parenthesis-shaped alar cartilage deformity" who benefited from a rhinoplasty with caudal rotation of the lateral crura performed between July 2011 and January 2013 at the 2nd Infirmary of the Santa Casa da Misericórdia in Rio de Janeiro and at one private clinic.
All patients underwent open rhinoplasty with general anesthesia and orotracheal intubation.
After marking of the domes and incisions with methylene blue, the nose was infiltrated with a 1/100,000 solution of adrenaline to reduce perioperative bleeding and facilitate dissection (hydrodissection). A marginal and transcolumellar incision in an "inverted V" shape, was performed to access the alar cartilages (Figure 1), which were detached (Figure 2). Excess cartilage in the lateral crura was assessed and resected at the cephalic and/or caudal edge (Figure 3).

Figure 1. Marginal and transcolumellar incision

Figure 2. Detachment and exposure of alar cartilages
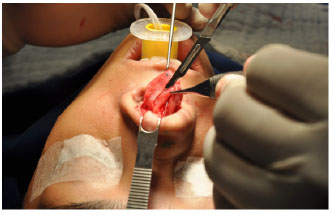
Figure 3. Excess resection of the lateral crura
Resection of the caudal excess allowed avoidance of irregularities at the alar rim9. Total detachment of the lateral crura and the dome was performed (release of the vestibule's skin) to exposure them (Figure 4 and 5). Next, a "columellar strut" was fixed between the two medial crura to maintain tip support. In cases of very weak and/or short lateral crus, a cartilaginous graft was added for support ("lateral crural strut graft") (Figure 6).

Figure 4. Total skin release from the vestibule of the lateral crura

Figure 5. Caudal rotation of the lateral crura

Figure 6. Fixation of the lateral crural strut grafts
The lateral extremity of this graft ("lateral crural strut graft") was supported at the edge of the piriform aperture, as shown by Gunter10, to prevent medial graft displacement. Transdomal and interdomal suturing was performed with 5/0 nylon thread, to stabilize the lateral crura in their new positions (Figure 7). With fine-tipped scissors, a pocket was made at the alar rim on each side to accommodate the rotated lateral crura (Figure 8). After the caudal rotation, the lateral crus stayed anchored inside the constructed pocket (Figure 9). In some cases, for greater safety, the cartilage was fixated with loose 6/0 nylon transcutaneous sutures (Figure 10) or 5/0 monocryl sutures on the skin of the vestibule.

Figure 7. Transdomal and interdomal sutures to stabilize the lateral crura in their new position

Figure 8. Preparation of the pockets to accommodate the rotated lateral crura

Figure 9. Insertion of the lateral crura inside the pockets

Figure 10. Fixation of the lateral crura with loose transcutaneous sutures
The patients' age group, sex, race, skin type, clinical characteristics of the alar cartilages, surgical modalities used to treat the deformity and the observed post-operative complications were analyzed.
RESULTS
In this study, 40 patients were female (92%) and 9 were male (18%). The mean age was 33 years, ranging from 18 to 74 years (Figure 11). Thirty-one patients were Caucasian (63%) and 18 were of African descent (37%); no Asian patients were included in our sample.
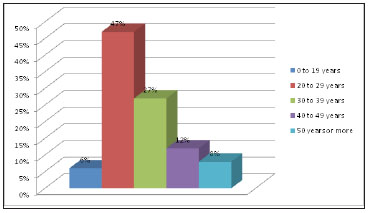
Figure 11. Patient age groups
In 90% of cases (44 patients), rhinoplasty was primary; in 4 patients, secondary rhinoplasty was performed, and in one patient, tertiary.
Thirty-five percent of patients (17 cases) had thick skin; 24%, thin skin (12 patients) and 41%, skin of intermediate thickness (20 patients). In 76% of cases (37 patients), the lateral crus was oriented towards the medial canthus of the eyelid, and in 24% of cases, it had an intermediate orientation (12 patients).
The clinical characteristics of the alar cartilages, relative to the parenthesis-shaped deformity, are summarized in Figure 12. We found excess alar cartilage in 61% of cases (30 patients), alar asymmetry in 18% (9 patients) and concave lateral crus in 12% of cases (6 patients).
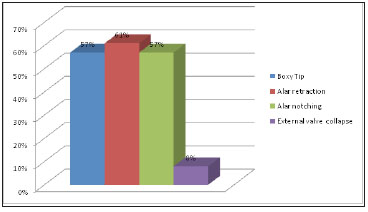
Figure 12. Parenthesis-shaped deformity characteristics
the surgical modalities used to treat the deformities are summarized in Figure 13.
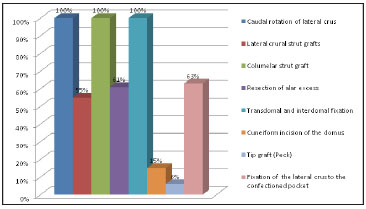
Figure 13. Surgical modalities used to treat parenthesis-shaped alae
Boxy tips were corrected in 100% of cases, as illustrated by Patients 1, 2 and 3 (Figures 14 to 18). Initial alar retraction was treated successfully in 97% of cases. Patients 1, 2 and 3 showed three different degrees of alar retraction, all corrected using the same technique (Figures 14 to 18). Alar pinching was corrected in 96% of cases, as shown in Figure 15. External valve collapse was successfully treated in 100% of cases, as shown in Patient 4 (Figure 19 and 20).

Figure 14. Front view and three-quarter view to the right of Patient 1. The case was a 37-year-old patient with a boxy tip, lateral crura oriented towards the medial canthus, bilateral marked alar retraction and left alar pinching. All characteristics were corrected using the technique described.

Figure 15. Right profile and nasal base view of Patient 1

Figure 16. Front view and three-quarter view to the left of Patient 2. The case was a 24-year-old patient with a boxy tip, bilateral moderate alar retraction and lateral crura oriented towards the medial canthus. All characteristics of the deformity were corrected by the same technique.

Figure 17. Left profile and nasal base view of Patient 2

Figure 18. Patient 3. The case was of a 29-year-old patient with a boxy tip, lateral crura oriented towards the medial canthus and mild bilateral alar retraction. The same technique was used to correct all characteristics.

Figure 19. Patient 4. The case was of a 27-year-old patient with external valve collapse and concave lateral crura oriented towards the medial canthus. All characteristics were corrected.
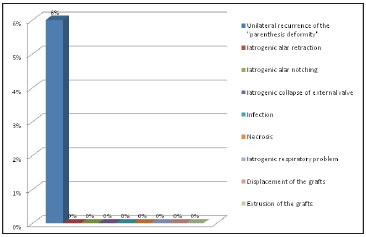
Figure 20. Post-operative complications
DISCUSSION
Sheen11,12 has described four characteristics of this deformity.
First, the caudal edge of the lateral crus appears almost perpendicular to the alar rim from the front, creating a visible discontinuity on the alar rim. He called it a "parenthesis-shaped deformity". All patients with this appearance between July 2011 and January 2013 were included in our study and treated by caudal rotation of the lateral crus. The majority of patients (76%) had the severe form of this deformity and all others presented with a moderate form (24%). Second, a broad, square tip, a "boxy tip", was found in 57% of patients. Third, pinching of the alar rim due to lack of support was observed in 57% of cases. Finally, the contour appeared square when viewed from the base of the nose (57% of patients).
Sheen11 described the lateral crura caudal rotation technique to treat this deformity. Here, we have also added the alar graft (lateral crural strut graft) described by Gunter10. Such a graft is suitable, according to Gunter, for the treatment of alar retraction, external valve collapse, or convex, concave or malpositioned lateral crus. The preferred source for this type of graft is the septal cartilage but, if this is depleted, costal cartilage could also be used10. Other modalities exist to correct it.
The cartilaginous graft on the alar rim (alar rim graft) can be used in mild retraction cases (3-4mm), if nasal lining and skin with appropriate elasticity are present, to allow expansion of the retracted ala13. In more serious cases, composite grafts, cartilaginous grafts fixated on the lateral crus (lateral crural strut graft) or a cartilaginous graft can be used to avoid external valve collapse (alar batten graft)7.
Caudal rotation of the lateral crura was the technique of choice (100% of patients) here, since patients had either a severe (76% of cases) or moderate (24% of cases) form of the deformity, as described by Sheen. No mild form justifying an alar rim graft was found. A lateral crural strut graft with caudal rotation was applied in 27 patients (55% of cases), as they showed a weak and/or concave lateral crus, to ensure good definition and support of the alar rim. The use of septal cartilage grafts was also applied by several authors for cases of hypoplastic alar cartilage14,15. In our sample, no case of scar retraction of the skin of the vestibule justified the use of a composite graft.
A wedge incision into the domes has been proposed by several authors8,9 to reduce tension in the domes at the time of caudal rotation, thereby making its approximation easier. This incision was used in 15% of our cases.
There were 3 cases of unilateral deformity relapse following caudal rotation (6% of patients). In these cases, lateral crura were not fixated into the prepared pockets. These patients benefited from a second rhinoplasty with a new lateral crura caudal rotation and fixation into the pocket. There have been no cases of relapse since we began performing routine fixation.
Initial alar retraction was corrected in 97% of cases, alar pinching in 96% and external valve collapse in 100% of cases. There were no iatrogenic cases of alar retraction or pinching or external valve collapse. In his study, Constantian16 showed that external valve collapse occurs at the time of inspiration, when the alar rim is left without cartilaginous support. Cephalic-positioned caudal rotation of the lateral crus provides good support to the alar rim, thereby improving functional and aesthetic features, as shown by our results.
CONCLUSIONS
Parenthesis-shaped alar cartilage deformity must be acknowledged when planning surgery, since resection of the alar excess leaves the ala unsupported7 and may cause retraction and collapse of the external valve in the late postoperative period8,9.
We conducted a retrospective study with 49 cases treated by lateral crura caudal rotation, between July 2011 and January 2013. Our results encourage the selection of this technique as the first choice in the treatment of this deformity.
REFERENCES
1. Sheen JH. Aesthetic Rhinoplasty. St Louis, MO: CV Mosby; 1978.264-5.
2. Constantian MB. Functional effects of alar cartilage malposition. Ann Plast Surg. 1993;30:487-99.
3. Hamra S. Repositioning of the lateral alar crus. Plast Reconstr Surg. 1993;92(7):1244-53.
4. Peck GC. Techniques in aesthetic rhinoplasty. 2nd ed. Philadelphia: JB Lippincott. 1990. p.17-28.
5. Rees TD. Aesthetic plastic surgery. Philadelphia: WB Saunders.1980: p.181-187.
6. Daniel RK. Discussion: the two essential elements for planning tip surgery in primary and secondary rhinoplasty: observation based on review of 100 consecutive patients. Plast Reconstr Surg. 2004;114(6):1582-5.
7. Boahene KD, Hilger PA. Alar rim grafting in rhinoplasty: indications, technique, and outcomes. Arch Facial Plast Surg. 2009;11(5):285-9.
8. Hamra ST. Repositioning the lateral alar crus. Plast Reconstr Surg. 1993;92(7):1244-53.
9. Rochira D, Ottaviani A. Malposition of alar cartilages: a personal modification of the Sheen technique. Plast Reconstr Surg. 2008;122(2):72e-3e.
10. Gunter JP, Friedman RM. Lateral crural strut graft: technique and clinical applications in rhinoplasty. Plast Reconstr Surg. 1997;99:943.
11. Sheen JH, Sheen AP. Aesthetic Rhinoplasty, 2nd Ed. St Louis: Mosby, 1987.
12. Sheen JH. Malposition of the Alar Cartilages. Presented at the Annual Meeting of the American Society of Aesthetic Plastic Surgery, May 1992; Los Angeles, USA.
13. Brissett AE, Shari's DA. Changing the nostril shape. Face Plast Clin North Am. 2000;8:433-45.
14. Constantian MB. The incompetent external nasal valve: pathophysiology and treatment in primary and secondary rhinoplasty. Plast Reconst Surg. 1994;93(5):919-31; discussion 932-3.
15. Fomom S, Gilbert JG, Carou AL, Segal S. Collapsed ala. Arch Otolaryngol. 1950;51:465-84.
16. Constantian MB. The external Nasal Valve: The Forgotten Element in Rhinoplasty Diagnosis and Treatment. Presented at the Annual Meeting of the American Society of Aesthetic Plastic Surgery; May 1992; Los Angeles, USA.
1 - Full Member of the Brazilian Society of Plastic Surgery, Professor at the 2nd Infirmary of the Santa Casa da Misericórdia, Rio de Janeiro, Brazil
2 - Diploma in General Surgery, Postgraduate Student at the Ivo Pitanguy Institute
3 - Full Professor of Plastic Surgery at the Fluminense Federal University, Full Professor of Plastic Surgery at the Federal University of Rio de Janeiro, Honorary Doctor of the Simom Bolivia University (Colombia), Associate Professor at the Ivo Pitanguy Institute, Assistant Professor at the 2nd Infirmary of the Santa Casa da Misericórdia of Rio de Janeiro, Senior Fellow of the Brazilian Society of Plastic Surgery, Senior Fellow of the Brazilian College of Surgeons
Institution: 2nd Infirmary of the Santa Casa da Misericórdia, Rio de Janeiro.
Corresponding author:
Ali Bouchama
Rua Santa Luzia, 206 - Centro
Rio de Janeiro (RJ) - CEP: 20020-020
E-mail: alidocsurf@gmail.com
Article received: June 18, 2013
Article accepted: November 25, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter