

Original Article - Year 2014 - Volume 29 -
Blepharoplasty: transpalpebral brow elevation
Blefaroplastia: elevação transpalpebral das sobrancelhas
ABSTRACT
INTRODUCTION: The brows lowdown naturally occur as an aspect of the aging upper face process. The glabelar muscular action is one cause of this ptosis and also of others aging signs. These signs must be adequately treated during the blepharoplasty, to avoid the penalty of a limited final result.
METHODS: Along of the last 17 years, a total of 246 patients with aesthetic problems of the upper face and with blepharoplasty indication, were submitted to a transpalpebral browlift by modified McCord technique, based in a extended dissection, more fixation stitches and prócerus and corrugators muscles miomectomy. Out patients follow-up were in ambulatory conditions with photographic records after 6 and 12 months.
RESULTS: The most common intercurrence was a transient parestesia of the frontal region and of the scalp. No postoperative hematomas were registered. The results were consistent with maintenance of the eyebrows elevation and the effective reduction of the glabelar muscles action, without the necessity of any type of coronal incision.
CONCLUSIONS: The transpalpebral brow elevation associated with glabellar myomectomy shows to be an adequate option, by its safe and effective procedures for the treatment of the upper face aging signs.
Keywords: Brows; Transpalpebral Elevation; Brow lift; Corrugators Muscles Myomectomy; Blepharoplasty.
RESUMO
INTRODUÇÃO: A descida das sobrancelhas faz parte do processo natural de envelhecimento do terço superior da face. A ação da musculatura glabelar é uma das causas desta ptose e de outros sinais de envelhecimento. Estes sinais devem ser diagnosticados e tratados de maneira adequada durante os procedimentos de blefaroplastia sob pena de piora da ptose e de resultado não satisfatório.
MÉTODOS: Ao longo dos últimos 17 anos, um total de 246 pacientes, portadores de alterações do terço superior da face e com indicação de blefaroplastia, foram submetidos à elevação transpalpebral das sobrancelhas pela técnica de McCord modificada, mediante ampla dissecção, maior número de pontos de fixação e miomectomias dos músculos corrugadores e prócerus. Os pacientes foram acompanhados com avaliações ambulatoriais e com registros fotográficos nos 6 e 12 meses de pós-operatório.
RESULTADOS: A intercorrência mais comum foi a parestesia temporária da região frontal e do couro cabeludo. Não ocorreram casos de hematomas pós-operatórios. Ao longo do tempo foram observados resultados consistentes, com manutenção da elevação das sobrancelhas e diminuição efetiva da ação da musculatura glabelar, sem cicatrizes no couro cabeludo.
CONCLUSÕES: A elevação transpalpebral de sobrancelhas, associada à miomectomia glabelar, mostra-se uma alternativa adequada, segura e efetiva para tratamento dos sinais de envelhecimento do terço superior da face.
Palavras-chave: Sobrancelhas; Elevação Transpalpebral; Secção Músculos Corrugadores; Blefaroplastia.
Although the ideal position of the eyebrows is still a matter of debate and subject to racial and cultural variations, it is known that ptosis of the eyebrows is one of the changes resulting from the aging of the frontal and glabellar regions. Aside from the aesthetic problem this creates, an impaired field of vision may also occur in patients with ptosis of varying degrees.
A drop of the structures occurs due to gravity and the forces exerted by the muscles of this region (frontal, orbicularis, corrugator, procerus, and depressor supercilii). The most pronounced drop is on the side of the eyebrow due to lower traction of both the lower force of the frontal muscle in the eyebrow tail and the weaker attachment strength of the structures in the lateral region of the orbit. In addition, dynamic and static horizontal wrinkles of the forehead arise due to the constant force of the frontal muscle. Vertical wrinkles in the glabella, due to the corrugator muscle and the action of Procerus, leads to horizontal wrinkles in the nose1,2. Ptosis of the eyebrows often accompanies and accentuates the anatomic abnormalities of the upper eyelids3 and a failure or limitation in the correction of ptosis during upper blepharoplasty compromises the final aesthetic result.
In women, the highest ideal point should be between 0.5 and 1.0cm from the orbital rim, depicting a more pronounced arch. In men, the eyebrows should be flat along the orbital rim, with a less defined arch4.
The first attempts at browpexy and treatment in the upper third of the face date back to 19195. Since then, numerous authors have described various procedures and surgical approaches for changes in the upper third of the face. Since the initial publication on browpexy via a transpalpebral3 approach in 1982, several approaches have been proposed4-12. Ptosis of the eyebrows should be properly diagnosed and treated. Many patients seek surgical help with the false impression that an aged appearance is due only to eyelid changes, as in dermatochalasis. The surgeon, in turn, must be qualified to assess changes of the upper third of the face and propose specific treatment for the aesthetic problems. Upper blepharoplasty without proper correction of the drop in the structures in the upper third of the face can lead to a worsening of symptoms, due to suture of the eyelid skin and reduction of compensation by the frontal muscle 13.
AIMS
The aims of this study are to describe the technique and present the results obtained over 17 years in the treatment of ptosis of the eyebrows and glabellar muscles through transpalpebral access.
METHODS
The McCord technique 6 was modified by a wide dissection, a higher number of attachment sutures and myomectomy of the corrugator and procerus muscles13,14,15 applied in 246 patients with ptosis. Of these patients, 228 were female (92.7%) and 18 (7.3%) were male. All patients were referred from private and outpatient clinics of the Plastic Surgery Service of the Hospital das Clínicas of the Federal University of Minas Gerais. The age distribution of the 246 operated patients in decades was 14 patients (6%) 30-40 years old; 54 patients (22%) 40-50 years old; 117 patients (47%) 50-60 years old; 54 patients (22%) 60-70 years old and 7 patients (3%) 70-80 years old.
All patients underwent routine preoperative evaluation. Surgeries were always bilaterally associated with conventional blepharoplasty and usually performed under sedation and local anesthesia. Photographic documentation was performed pre- and postoperation at 6 and 12 months.
Markings
Markings were always performed with patients in the supine position. The area to be dissected was comprised of the whole extension of the eyebrows and extended in an arc anteriorly positioned in the frontal region. A medial and bilateral triangle not be dissected bordered the emergence area of the supraorbital and supratrochlear nerves, which were preserved [Figure 1]. Cutaneous excesses in the upper eyelids were marked for resection.

Figure 1. The lateral border of the detachment was the orbital ligament or Hakme ligament and its superior continuation, the accession zone. A triangle delimiting the emergence area of the supraorbital and supratrochlear nerves was not dissected.
After blepharorrhaphy, the skin was tractioned superiorly with a non-absorbable 6.0 monofilament suture and the lower incision on the upper eyelid crease was marked. Starting at a point 0.5cm from the outer edge of the palpebral commissure, the upper eyelid crease was marked to about 1.0cm from the medial corner of the eye. A line approximately 2.0cm long was drawn 0.5cm outside of the palpebral commissure that accompanies one of periorbital wrinkles. Using anatomical clamps, the skin excesses were also estimated and marked. Eyebrows were positioned in the calculated location of lift. The upper edge of skin and orbicularis muscle resection was marked, taking into account the remaining skin. This resection was always more lateral. The locations of the attachment sutures of the eyebrows were indicated by five punctate demarcations in the eyebrow (two lateral, one central, and two medial) (Figures 2 and 3).

Figure 2. Blepharoplasty marking was made from the upper eyelid crease, with care mark the eyebrow in the final programmed position to avoid excessive removal of eyelid skin.
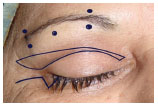
Figure 3. Five punctate demarcations in the eyebrow (two lateral, one central and two medial) indicated the location of the attachment sutures of the eyebrows.
By marking the lower edge of the skin resection of the upper eyelid crease, we were confident that the necessary skin for adequate coverage of the eyeball was available. We also gained direct access to the superior orbital rim without crossing any major anatomical structures.
By marking the top of the skin resection with the eyebrows in the calculated location of the lift and paying attention to skin that is superiorly placed, a tensionless suture was made (Figure 2).
Surgical Technique
The patient was placed under operating conditions, with an anesthetic block of the supratrochlear and supraorbital nerves, and frontal area to be dissected by infiltration with 0.25% bupivacaine and 1% lidocaine with 1:100,000 epinephrine, together with a prolonged-effect corticosteroid to limit edema in the immediate postoperative period.
A skin incision and resection of skin and muscle excesses within the marked area on the upper eyelid were executed. From the midline of the resected area, dissection continued towards the superior orbital rim, with full exposure of the galea aponeurotica. Upon dissection of a distance of 4 cm, the adhesions between the galeal plane and soft tissues above were fully released. The galea was preserved on the periosteum to anchor the attachment points that maintain the eyebrows in place. This preservation also protected the deep branch of the supraorbital nerve running 2 cm below the area between the galea and the periosteum, which are anatomically attached to each other. Superiorly at the end of the galea fat pad, the deep branch of the supraorbital nerve switched to the intra-galeal2 layer (Figure 4 and 5).
The dissected area extended from the eyebrow to its medial edge and in a 4.0cm cranial arc. The medial triangular area marking the emergence of the supratrochlear and supraorbital nerves was not dissected (Figure 1). The lateral limit of dissection was the orbital or Hakme ligament. Its superior continuation, the accession zone, was preserved. The adhesions of the galea to the fat pad and frontalis muscle were released to the extent estimated to be necessary to achieve the desired lift in the eyebrow2 (Figures 4 and 5).

Figure 4. Dissection in the galea aponeurotica, allowing medial visualization of the superficial branch of the supraorbital nerve. The galea was preserved on the periosteum to anchor the attachment points of the eyebrows. This preservation also protected the deep branch of the supraorbital nerve by keeping it below or inside the galea.

Figure 5. Illustration of the region's anatomy showing the detachment area in the galea aponeurotica.
Dissection and resection of the small portion of the corrugator muscle was executed between the supraorbital and supratrochlear bundles (Figure 6). When it was very hypertrophic, the procerus muscle was dissected and sectioned under direct vision with the aid of a cold light source (Figure 7). Grafts with fat pads were added selectively in the resected areas of the corrugator and sections of the procerus muscles to avoid depressions13-15.

Figure 6. Corrugator muscle isolated for resection between the supratrochlear and supraorbital muscle bundles

Figure 7. Procerus muscle exposed for sectioning with the aid of a cold light source
Fixation was accomplished along each eyebrow using five sutures with non-absorbable 5.0 monofilament. Two medial sutures, one median and two lateral sutures were used, with the latter positioned at the tail of the eyebrow. The first medial suture was applied immediately lateral to the supraorbital nerve in the projection of the upper edge of the eyebrows, through the inner side of the dissected soft tissues and internally bordering the dermis. The needle was returned to the inner edge of the soft tissues and the suture loop was pulled down. If the exterior was profoundly marked, a new loop was made with the needle farther from the dermis to avoid external depressions at the attachment sites of the sutures. The suture was completed by crossing the galea and the periosteum about 2.0 cm from the superior orbital rim. The suture was firm and did not have too much tension. The second suture was made in the same way, along the projection of the lower margin of the eyebrow and was set in the galea and periosteum, several millimeters below the first suture. The third and fourth sutures were added in the same way in relation to the eyebrow tail and were fixed in the periosteum and galea at the same height as the first two sutures. The fifth suture was added midway between the first four (Figure 3).
In women, eyebrows should be set between 0.5 and 1.0 cm above the superior orbital margin; in men, along the orbital margin. The sutures form fixing loops and a natural drop occurs, which must be compensated by higher attachment points to obtain the final position of the eyebrows.
This is an outpatient procedure and patients are discharged after the post-anesthetic recovery period. Postoperative guidance is the same as in a conventional blepharoplasty, and the patient should be alert for the presence of a large edema, which may occur in cases with more manipulation and larger dissected areas. Patients received follow-up examinations in outpatient care after 3, 7, 15, 30, 90, 180, and 365 days.
RESULTS
The results of these procedures have been consistent over 17 years, with one of the obvious advantages the circumvention of coronal incisions of any length. Regarding endoscopic approaches, they have a lower complexity of implementation, easier learning curve and lower cost.
In this study, the most frequent complication was bilateral paresthesia of the frontal and parietal scalp, which resolved spontaneously after a few months. Initial bilateral numbness in the areas of the supratrochlear nerves and superficial and deep branches of the supraorbital nerve occurred. This insensitivity is reduced from the posterior area of the parietal region toward the frontal area after several weeks, with some patients still having points of paresthesia for several months. In most cases, this occurs during the initial phase of a large edema, or partial or complete paralysis of the frontalis muscle, which was never permanent in any patient.
There were no postoperative hematomas. Some cases had initial depressions in the treatment areas of the glabellar muscles, which were not seen after the use of fat pad grafts added during blepharoplasty. These grafts were used in all patients, except in the initial ones that demonstrated no such need. Figures 8 to 15 illustrate the results obtained.

Figure 8. Preoperative and 4-year postoperative images of a 39-year-old patient

Figure 9. Preoperative and 12-month postoperative images of a 46-year-old patient

Figure 10. Preoperative and 6-month postoperative images of a 47-year-old patient

Figure 11. Preoperative and 8-year postoperative images of a 52-year-old patient

Figure 12. Preoperative and 1-year postoperative images of a 55-year-old patient

Figure 13. Preoperative and 10-year postoperative images in a patient 61 years old at the time of operation. Maintenance of the eyebrows in a higher position than the preoperative position is evident.

Figure 14. Preoperative and 13-month postoperative images of a 70-year-old patient

Figure 15. Preoperative and 8-year postoperative images of a patient operated at 74 years. At 82 years, maintenance of the eyebrows in a higher position than the preoperative position is evident.
DISCUSSION
The surgical approach to the upper third of the face requires an understanding of the anatomical features that define a youthful appearance and changes that cause an aged appearance. The opinions of different races and cultures regarding the appearance and position of an aesthetically pleasing eyebrow differ greatly. A suitable position is one where the medial part begins in a vertical line and touches the nose wing.
In women, the highest ideal point is between 0.5cm and 1.0cm from the orbital rim, presenting a more pronounced arc. In men, the eyebrow should be flat along the orbital rim with a less defined arc 4.
Aging leads to a drop of these structures due to gravity and the forces exerted by the muscles of this region (frontal, orbicularis, corrugator, procerus, and depressor supercilii). The drop is most pronounced on the side of the eyebrow due to lower support, due to lower activity of the frontal muscle in the eyebrow tail and the weaker attachment of the structures on the side of the orbit, which determine the pseudo-excess skin on the eyelid. Dynamic and static horizontal wrinkles arise on the forehead due to the constant activity of the frontal muscle, the only elevator muscle of the eyebrows. Vertical wrinkles appear on the glabella due to the corrugator muscle. The action of the procerus muscle leads to horizontal wrinkles in the nose1,2. Finally, in addition to aesthetic problems, there can be a loss of the field of vision in patients with moderate to severe ptosis, necessitating treatment.
There are many published contributions to the aesthetic and functional improvement of blepharoplasty. Several reports16 have studied the degree of improvement in quality of life of patients undergoing browpexy via a transpalpebral approach. Anatomical studies1,2 have outlined the surgical goals of the procedures used to treat eyebrow ptosis. Firstly, the periosteum or galea adhesions in the superior orbital rim must be released. The orbital ligament, a ligamentous structure between the plane of the superficial temporal fascia and the side of the superior orbital rim, should also be released. Lastly, the accession zone, an area about 6 mm wide located medially to the upper temporal fusion line of the skull, which continues inferiorly with the orbital ligament, should be released. Throughout this area, the periosteum and galea should be fixed to the bone.
The detachment proposed by us occurred in the galea aponeurotica and such structures were not detached from the bone. We essentially released the galea from the fat pad and the frontal muscle, preserving the accession zone (Figure 5).
Over the years, different approaches have been proposed, such as direct excisions in the supraorbital or frontal region, and coronal, endoscopic, temporal and transpalpebral approaches. Each one has its own peculiarities, specific indications, advantages and disadvantages5,8. Initial work on the transpalpebral approach in 19823 was followed by numerous publications and refinements4-12. In 1990, a browpexy and browplasty technique6 using a conventional incision for upper blepharoplasty was published. The small dissection applied limited the lift of the eyebrows and the preserved glabellar muscles tended to cause recurrence of ptosis.
In this study, we propose the use of a wide dissection of the frontal region, with fixation of the eyebrows with a larger number of points, more cranial, with a more effective lift. It associates treatment of glabelar13-15 muscles in order to limit the caudal traction of these muscles and prevent recurrence of ptosis.
The transpalpebral approach has, in comparison to other approaches, the advantage of not requiring another incision other than the one used in blepharoplasty. It allows easy access, direct visualization, release of the periorbital structures, and treatment of glabellar muscles. The procedure is safe and avoids an increase in the length of the upper third face. It can be used in bald patients and does not cause alopecia. In our study, these procedures led to good results, high levels of patient satisfaction and a low rate of complications.
CONCLUSION
The transpalpebral eyebrow lift associated with upper blepharoplasty enables satisfying aesthetic effects in the long term in patients over several decades without the use of more aggressive procedures that leave scars on the scalp. Systematic surgical maneuvers are assimilated by a short training period and the use of devices and long training periods in endoscopic surgery are unnecessary.
REFERENCES
1. Knize DM. An anatomically based study of the mechanism of eyebrow ptosis. Plast Reconstr Surg. 1996;97(7):1321-1333.
2. Knize DM. Anatomic concepts for brow lift procedures. Plast Reconstr Surg. 2009;124(6):2118-2126.
3. Sokol AB, Sokol TP. Transblepharoplasty Brow Suspension. Plast Reconstr Surg. 1982;60(6):940-944.
4. Codner MA, Kikkawa DO, Korn BS, Pacella SJ. Blepharoplasty and browlift. Plast Reconstr Surg. 2010;126(1):01-17.
5. Paul MD. The evolution of the brow lift in aesthetic plastic surgery. Plast Reconstr Surg. 2001;108(5):1409-1424.
6. McCord CD, Doxanas MT. Browplasty and browpexy: an adjunct to blepharoplasty. Plast Reconstr Surg. 1990;86:248-254.
7. Zarem HA. Browpexy. Aesth Surg J. 2004;24(4):368-372.
8. Niechajev I. Transpalpebral browpexy. Plast Reconstr Surg. 2004;113(7):2172-2180; discussion pp. 2181.
9. Tyers AG. Brow lift via the direct and trans blepharoplasty approaches. Orbit, 2006;25:261-265.
10. Langsdon PR, Metzinger SE, Glickstein JS, Armstrong DL. Trans-blepharoplasty brow suspension: an expanded role. Ann Plast Surg. 2008;60(1):02-05.
11. Cintra HP, Basile FV. Transpalpebral browlifting. Clin Plast Surg. 2008;35:381-392; discussion pp. 379.
12. Graziosi AC, Beer, SMC. Browlifting with undermining using minimum incisions. Aesth Plast Surg. 1998;22:120-125.
13. Guyuron B, Michelow BJ, Thomas T. Corrugator supercilii muscle resection through blepharoplasty incision. Plast Reconstr Surg. 1995;95(4):691-696.
14. Knize DM. Transpalpebral approach to the corrugator supercilii procerus muscles. Plast Reconstr Surg. 1995;95(1):52-60; Discussion pp. 61-62.
15. Guyuron B, Knize DM. Corrugator Supercilii Resection through Blepharoplasty Incision. Plast Reconstr Surg. 2001;107(2):606-607.
16. Mellington F, Khooshabeh R. Brow ptosis: are we measuring the right thing? The impact of surgery and the correlation of objective and subjective measures with postoperative improvement in quality-of-life. Eye (Lond). 2012 Jul;26(7):997-1003.
1 - Coordinator of the Plastic Surgery Service, Hospital das Clínicas, UFMG, Adjunct Professor, Faculty of Medicine, UFMG
2 - Medical specialist in Plastic Surgery, Ex-resident of SCPHCUFMG
3 - Resident Physician, 3rd Year, SCPHCUFMG
4 - Resident Physician, 2nd Year, SCPHCUFMG
5 - Resident Physician, 2nd Year, SCPHCUFMG
Institution: Plastic Surgery Service, Hospital das Clínicas, UFMG.
Corresponding author:
Armando Chiari Júnior
Rua Herculano de Freitas, 58, Sala 110
Belo Horizonte, Minas Gerais 30441-039 Brazil.
E-mail: chiari@chiari.com.br
Article received: November 21, 2013
Article accepted: February 9, 2014


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter