

Case Report - Year 2013 - Volume 28 -
Leiomyoma of hand
Leiomioma de mão
ABSTRACT
The aim of this report was to present the case of a leiomyoma with a rare anatomical location and an unusual age of disease onset. The patient was a 17-year-old girl who developed a leiomyoma of the hand. Leiomyoma is a benign smooth muscle tumor that most frequently occurs in the uterine cavity. When it occurs in the extremities, it is most common in the legs, feet, and ankles. Leiomyoma usually develops between the third and fourth decades of life and is rarely identified before surgical resection. Thus, a histological examination is necessary to confirm the diagnosis.
Keywords: Leiomyoma. Hand. Tumor.
RESUMO
O objetivo deste trabalho é relatar o caso de uma jovem de 17 anos que desenvolveu leiomioma na mão esquerda: raro sítio anatômico de localização e idade incomuns de desenvolvimento da doença. O leiomioma é um tumor benigno de músculo liso, raro e incomum na mão, apresentando-se com maior frequência na parede da cavidade uterina. Quando de ocorrência em extremidades é mais comum na região das pernas, dos pés e dos tornozelos. Em geral se desenvolve entre a terceira e a quarta décadas de vida e raramente é identificado antes da ressecção cirúrgica. Dessa forma, faz-se necessário, para a confirmação do diagnóstico, um exame histológico.
Palavras-chave: Leiomioma. Mãos. Tumor.
Leiomyoma is a benign smooth muscle tumor, which occurs more often in women, specifically in the uterus. The occurrence of leiomyoma in the hand is extremely rare because of the minimal amount of smooth muscle in the area. Leiomyoma of the hand is predominantly vascular in origin but may also arise from the erector pili muscles, muscles adjacent to glands or from deep soft tissues.
This report describes the case of a 17-year-old girl who attended the Plastic Surgery Service of the University Hospital of Brasília, whose complaint was a painless nodule in her left hand, which had been growing for 7 years. The nodule was resected, and a diagnosis of leiomyoma was made based on the immunohistochemical analysis result.
CASE REPORT
A 17-year-old patient presented to the Plastic Surgery Service of the University Hospital of Brasília with a 7-year history of a painless, slow-growing tumor in the volar aspect of the fifth finger of the left hand. On physical examination, the hardened tumor was 7 cm in diameter, mobile, not adhered to deep planes, and not painful to palpation (Figure 1). Examinations of the vascular, sensory, and motor functions of the left hand showed no significant changes.

Figure 1 - The tumor that measured 7 cm in diameter and involved the volar region of the fifth finger of the left hand.
Under brachial plexus block, an incision was made on the base of the tumor. A skin flap was elevated, and the neurovascular pedicles of the volar aspect of the fifth finger of the left hand were identified and preserved. The tumor was encapsulated and did not involve the flexor tendon sheaths of the fifth finger, vessels, or digital nerves. The dissection around the capsule was simple, and the tumor was completely removed (Figure 2).
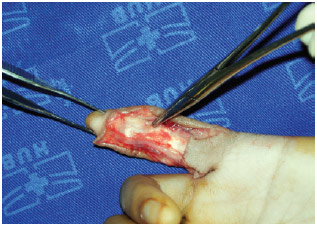
Figure 2 - Immediate postoperative aspect, with preservation of the tendon, nerve, and vascular structures of the fifth finger of the left hand.
An immunohistochemical study using antibodies directed against smooth muscle alpha actin, desmin, S-100 protein, and cell proliferation antigen Ki-67 revealed diffuse immunoreactivity for desmin and smooth muscle actin and negative results for S-100 protein and Ki-67. Accordingly, a diagnosis of leiomyoma was made (Figure 3). The patient had no evidence of recurrence during the 2-year postoperative follow-up examination and showed no motor or sensory limitation of the left hand (Figures 4 and 5).
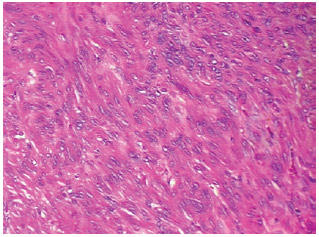
Figure 3 - Bundles of spindle cells without atypia (hematoxylin-eosin staining, original magnification x100).
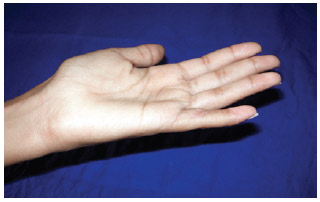
Figure 4 - Postoperative aspect at 2 years, with preservation of extension of the fifth finger of the left hand.

Figure 5 - Postoperative aspect at 2 years, with preservation of flexion of the fifth finger of the left hand.
DISCUSSION
Leiomyoma is an extremely rare tumor that affects the smooth muscles, predominantly the uterus, as tumor cells are hypersensitive to estrogen. It has been reported to occur in the esophagus, intestine, lung pleura, and lower extremities1. Only a few cases with hand involvement are reported in the medical literature because of the lack of smooth muscles in the hand, being present only in the tunica media of vessels, the erector muscles, and the muscles adjacent to glands. Leiomyoma can be vascular, cutaneous, and of deep soft tissues. Leiomyoma of the hand is most commonly vascular, originating in the tunica media layer of veins1. Cutaneous tumors are intradermal and originate in the erector pili muscles. Deep soft tissue leiomyomas have not been described in the hand but are generally present as large tumors in the lower extremities.
Normally, leiomyoma of the hand occurs between the third and fourth decades of life, affecting more women than men2. The first reported case of leiomyoma of the hand was published in 1960 by Butler et al.3. In most cases, the leiomyoma does not affect bone and neurovascular structures, is approximately 2 cm in diameter, and is encapsulated.
Only a few cases involving children have been reported2,4. The youngest patient reported was 10 years old and a human immunodeficiency syndrome carrier. This patient had multiple skin tumors, some of which were leiomyomas. Among children, the most common benign tumors of the hand are those arising from congenital malformations5.
On clinical examination, nodules ranging from 2 to 7 cm in diameter are detectable. However, most tumors are less than 2 cm in diameter, with calcified parts in the nodules4. When in an advanced state, such tumors become a source of pain to the patient. Information on clinical history is usually available for tumors reported between 6 and 12 months, during which the pain tends to become increasingly severe, probably owing to nerve compression. The most frequently recommended test for the analysis of anatomical boundaries of the nodule is magnetic resonance imaging (MRI), as a radiological examination is only useful for prominent tumors of the hand and radiography itself cannot provide enough bases to diagnose benign tumors. MRI can detect homogeneous tumors with well-defined boundaries without involvement of neurovascular structures, which helps in the differentiation of malignant tumors because the latter usually involve neurovascular structures.
The differential diagnosis of hand tumors includes synovial cysts, fibroma, lipoma, schwannoma, glomus tumor, neurofibroma, neurilemmoma, melanoma, nodular fasciitis, and vascular malformations6.
The optimal treatment of leiomyoma of the hand is complete surgical resection because tumor growth may cause discomfort to the patient, such as pain or hand motor function impairment7. Natural or drug-induced regression of smooth muscle tumors has not yet been reported5, neither has tumor recurrence after complete resection4,5,7.
For a definitive diagnosis of leiomyoma, a histopathological study of the surgically resected nodule is necessary. On histological examination, a leiomyoma appears to be composed of bundles of spindle cells that tend to intersect each other at right angles. Tumor cells have elongated nuclei with blunt ends and show minimal atypia and few mitotic figures. Three types of leiomyomas have been described as follows: solid, composed of smooth muscle bundles surrounded by thin-walled vessels that intersect one another; cavernous, containing dilated vascular channels with small amounts of smooth muscle; and venous, comprising channels with thick bundles of smooth muscle easily distinguishable from adjacent bundles of smooth muscle1,8.
In the present case, the leiomyoma was cutaneous and histologically solid, with a favorable prognosis. According to the clinical history of the patient, the tumor likely began to develop at 10 years of age. The case is distinct because of the location and size of the leiomyoma, and patient's age.
Leiomyoma of the hand is rare and should be diagnosed when the patient presents with slow-growing isolated nodules. The optimal treatment is complete surgical resection. The diagnosis can only be confirmed through histopathological analysis.
ACKNOWLEDGEMENTS
We thank Dr. Larissa Sena Teixeira Mendes of the Department of Pathology, University Hospital of Brasília, University of Brasília, for providing the histological material.
REFERENCES
1. Kulkarni AR, Haase SC, Chung KC. Leiomyoma of the hand. Hand. 2009;4:145-9.
2. Yang SS, Williams RJ, Bear BJ, McCormack RR. Leiomyoma of the hand in a child who has the human immunodeficiency virus. J Bone Joint Surg Am. 1996;78:1904-6.
3. Butler E, Hamil J, Seipel R, Dellorimier A. Tumors of the hand. A ten-year survey and report of 437 cases. Am J Surg. 1960;100:293-302.
4. Maresca A, Gagliano C, Marcuzzi A. Leiomyoma of the hand: a case report. Chir Main. 2005;24:193-5.
5. Boutayeb F, El Ibrahimi A, Chraibi F, Znati K. Leiomyoma in an index finger: report of case and review of literature. Hand. 2008;3:210-1.
6. Sobanko JF, Dagum AB, Davis IC, Kriegel DA. Soft tissue tumors of the hand. 1. Benign. Dermatol Surg. 2007;33:651-67.
7. Harb Z, Bismil Q, Ricketts DM. Trigger finger presenting secondary to leiomyoma: a case report. J Med Case Rep. 2009;3:7284.
8. Jimenez RM, Jaramillo D, Connolly SA. Imaging of the pediatric hand: soft tissue abnormalities. Eur J Radiol. 2005;56(3):344-57.
1. PhD, associate professor of the Faculty of Medicine, University of Brasília (UnB), full member of the Brazilian Society of Plastic Surgery (BSPS), Brasília, DF, Brazil
2. Medical student, Faculty of Medicine, UNB, Brasília, DF, Brazil
3. Master in Medicine by the UnB, full member of the BSPS, Brasília, DF, Brazil
Correspondence to:
Jefferson Lessa Soares de Macedo
SQS 213 - Bloco H - ap. 104 - Asa Sul
Brasília, DF, Brazil - CEP 70292-080
E-mail: jlsmacedo@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: 10/24/2010
Article accepted: 2/15/2011
Work conducted in the Plastic Surgery Service, University Hospital of Brasília, Brasília, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter