

Ideas and Innovation - Year 2012 - Volume 27 -
Design of a novel surgical instrument for rhytidoplasty: the SMAS suspension needle
Design de novo instrumento cirúrgico para ritidoplastia: agulha para suspensão do SMAS
ABSTRACT
This article describes an alternative surgical instrument that can be used for suspension of the malar fat pad. The needle was created using Kirschner wire to ensure that both tips were blunt. The double tip allows for passage of the wire through the superficial muscular aponeurotic system, ensuring that the suture is sufficiently deep to avoid dermatography. The utility of the new instrument was tested in rhytidoplasties involving minimal dissection. The needle described herein was proven safe, and could easily migrate through the tissues, without creating vascular and nerve lesions, and facilitate the positioning of the fixation points at the intended sites. The use of this needle for rhytidoplasty was quick, simple, and cost-effective, without any resulting dissection or damage to the anatomical structures or tissues.
Keywords: Face/surgery. Rhytidoplasty/methods. Rejuvenation.
RESUMO
Neste artigo é apresentado um instrumento cirúrgico alternativo para suspensão da camada fibroadiposa do terço médio da face. A agulha foi confeccionada com fio de Kirschner, de forma que ambas as pontas se tornaram rombas. A dupla ponta possibilita a passagem do fio pelo sistema musculoaponeurótico superficial da face (SMAS), mantendo a sutura com a profundidade necessária para evitar dermatografia. Os testes com o novo instrumento foram realizados em ritidoplastias com dissecção mínima. A agulha descrita demonstrou-se segura, com fácil migração pelos tecidos e ausência de lesões vasculonervosas, facilitando o posicionamento dos pontos de fixação nos locais planejados. A agulha desenvolvida possibilitou a realização da ritidoplastia sem descolamento resultante de forma rápida, simples e custo-efetiva, com mínimo dano às estruturas anatômicas e aos tecidos.
Palavras-chave: Face/cirurgia. Ritidoplastia/métodos. Rejuvenescimento.
The development of minimally invasive techniques is a current trend in modern plastic surgery. Treatments with fewer complications, shorter surgical time, more discrete scars, and effective facial contour correction are increasingly being developed. Several studies in the national and international literature demonstrated the effectiveness of wire facial suspension techniques, either isolated or in combination with rhytidoplasty, such as round block, Russian wire, and others, that attempt to meet such demands1,2.
Surgical procedures are considered surgeon-dependent; therefore, the instruments used are of paramount importance in obtaining good results. The use of surgical needles in daily practice and the need for greater agility during surgery prompted the development of a novel device that facilitates the use of suture wires within that context1.
The current study presents a model of an easily built device that was initially developed for use in rhytidoplasties with minimal resulting dissection.
METHODS
The device was designed to enable the fixation of the repositioning of the superficial muscular aponeurotic system (SMAS) and of the malar fat pad using subcutaneous sutures without dissection.
The needle was created using Kirschner wire to ensure that both tips are blunt (Figure 1). The instrument has a body diameter of 2.5 mm, which is 3 mm at the tip, and is 22 cm long.
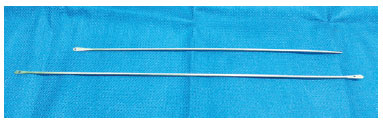
Figure 1 - Needle for superficial muscular aponeurotic system suspension. The double blunt tip has orifices for wire passage.
The round and atraumatic double tip, with holes at both extremities, allows the passage of common suture wires (Figure 2). The double tip allows for passing of the wire through the SMAS without exiting the skin and ensuring that the suture is sufficiently deep to avoid dermatography.

Figure 2 - Passage of wire through the retroauricular region with the wire mounted on the distal extremity.
The atraumatic round tip prevents the formation of lesions in vascular and nerve structures of the face that may result from the maneuvering of sharp instruments without any visual guidance.
The new instrument was tested in rhytidoplasties, wherein the needle was passed through the subcutaneous tissue without cutting the skin, with its passage being facilitated by an incision with a scalpel through the external portion of the skin (Figure 3).

Figure 3 - Encircling of the muscular and aponeurotic structures without any dissection.
Surgical Technique
The patients were administered general anesthesia as well as local anesthesia with 0.25% lidocaine and epinephrine at a 1:200,000 ratio in the region of the face to be dissected.
Pre- and retroauricular incisions and minimal dissection were made to limit the portion of redundant skin to be resected. The needle was introduced through the retroauricular region to allow for positioning of the clear 4.0 nylon wire. After the SMAS was encircled with the wire, the threadless needle with holes at both extremities facilitated the easy return of the wire to the retroauricular region, where the knots were tied. Three fixation points were used and selected for suspension of the midface and the cervical region. Following cutaneous resection, synthesis was performed without resulting dissection.
RESULTS
The needle described here proved to be safe, could migrate easily through tissue, did not cause vascular or nerve lesions, and facilitated positioning of the fixation points at the intended sites.
DISCUSSION
SMAS suspension with traction points contributes to maintaining the aesthetic features of the skin by decreasing the tension in the scar region and improving facial contour by repositioning the deep structures3. The use of varying techniques for closed suturing of such structures is widespread, although they are associated with certain limitations such as mild to moderate ptosis of the muscular and aponeurotic structures, discrete or absent skin redundancy, and limited results4,5.
The development of a new instrument that is able to combine minimally invasive rhytidoplasty with SMAS suspension enables obtaining a satisfactory aesthetic result along with short surgery time, less trauma, and discrete scars. This device improves results and makes the operation easier for the surgeon.
This instrument differs from other commercially available needles, such as Casagrande, Reverdin, and Graziosi needles, due to the absence of a thread, which allows structures to be passed through, and by the presence of a double tip with holes for the passage of wire, which facilitates passage and return of the needle through the tissue. The absence of wire externalization enables structures to be stitched at a certain depth, away from the skin surface, thus avoiding dermatography. During attempts to perform the same procedures using the other needles, several passages and wire removals were needed, which prolonged surgery time and made the procedure difficult to perform.
CONCLUSIONS
The newly developed needle allows rhytidoplasty to be performed quickly, simply, and cost-effectively without any resulting dissection and with minimal damage to anatomical structures and tissues. This instrument offers the promise of reduced surgical trauma and diminished complication rates, and has the potential to become a clinically effective instrument in SMAS suspension.
REFERENCES
1. Atiyeh BS, Dibo SA, Costagliola M, Hayek SN. Barbed sutures "lunch time" lifting: evidence-based efficacy. J Cosmet Dermatol. 2010;9(2):132-41.
2. Bafutto MG. Agulha para pontos internos de suspensão por fios. Rev Bras Cir Plást. 2008;23(4):310-2.
3. Farrapeira AB. Abordagem segmentar do terço médio da face. Triângulo na região geniana: ponto de sutura dermogorduroso. Rev Bras Cir Plást. 2009;24(4):497-503.
4. Murtha AP, Kaplan AL, Paglia MJ, Mills BB, Feldstein ML, Ruff GL. Evaluation of a novel technique for wound closure using a barbed suture. Plast Reconstr Surg. 2006;117(6):1769-80.
5. Fernandes JW. The sling lift: an ancillary procedure for malar rejuvenation. Aesthetic Plast Surg. 2007;31(5):454-9.
1. Resident physician of Plastic Surgery and Reconstructive Microsurgery Department, Hospital Universitário Walter Cantídio da Universidade Federal do Ceará (Walter Cantídio University Hospital, Federal University of Ceará), associate member of the Sociedade Brasileira de Cirurgia Plástica/Brazilian Society of Plastic Surgery (SBCP), Fortaleza, CE, Brazil.
2. Plastic surgeon, associate member of the SBCP, preceptor at the Plastic Surgery and Reconstructive Microsurgery Department, Hospital Universitário Walter Cantídio da Universidade Federal do Ceará (Walter Cantídio University Hospital, Federal University of Ceará), Fortaleza, CE, Brazil.
3. Medical student at the Universidade Federal do Ceará (Federal University of Ceará), Fortaleza, CE, Brazil.
4. Plastic surgeon, full member of the SBCP, regent of the Plastic Surgery and Reconstructive Microsurgery Department, Hospital Universitário Walter Cantídio da Universidade Federal do Ceará (Walter Cantídio University Hospital, Federal University of Ceará), Fortaleza, CE, Brazil.
Correspondence to:
Juliana Régia Furtado Matos Rua Mombaça, 164 - Aldeota
Fortaleza, CE, Brazil - CEP 60160-190
E-mail: julianarfm@gmail.com
This study was performed at the Plastic Surgery and Reconstructive Microsurgery Department of the Hospital Universitário Walter Cantídio da Universidade Federal do Ceará (Walter Cantídio University Hospital, Federal University of Ceará), Fortaleza, CE, Brazil.
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: June 5, 2012
Article accepted: July 23, 2012


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter