

Original Article - Year 2012 - Volume 27 -
Surgical treatment of basal and squamous cell carcinomas: experience of the Plastic Surgery Services of Hospital Ipiranga
Tratamento cirúrgico dos carcinomas basocelular e espinocelular: experiência dos Serviços de Cirurgia Plástica do Hospital Ipiranga
ABSTRACT
BACKGROUND: A higher incidence and prevalence of non-melanoma skin cancers has been reported in Brazil. Among them, basal cell carcinoma (BCC) is the most common, accounting for 70%-75% of all cases. Squamous cell carcinoma (SCC) constitutes 20% of non-melanoma skin cancers. The aim of this study was to examine the patients who underwent surgery for the treatment of non-melanoma skin cancer between 2005 and 2010 at the Plastic Surgery Service of Hospital Ipiranga.
METHODS: The medical records of the patients who were treated for non-melanoma skin cancer at the surgical center were reviewed and classified according to age, gender, occupation, race, anatomical location, risk factors, number of lesions, and histological subtype.
RESULTS: A total of 145 patients were evaluated; 15.9% exhibited multiple lesions, which resulted in a total of 168 tumors. BCC was most commonly detected (87.6% of the tumors), whereas 26.2% of tumors were SCC. Solid or nodular BCC comprised 44.1% of all skin cancers, whereas Broders I SCC accounted for 42.1% of SCC cases. The lesions were present on the face in 80.7% of the patients and on the upper limbs in 12.4%. The average patient age was 69.5 years, and 59.4% of the patients were female. The tumors were more commonly observed in Caucasians, and smoking was the major risk factor recorded in 79.3% of cases.
CONCLUSIONS: The patients with cancer in this study tended to have BCC and/or were predominantly female - observations that reflect the current tendency of this tumor. The presence of a significant number of patients with multiple lesions emphasizes the importance of undergoing a periodic examination. Moreover, high smoking rates were observed among these patients.
Keywords: Basal cell carcinoma. Squamous cell carcinoma. Carcinoma/surgery.
RESUMO
INTRODUÇÃO: Os tumores de pele malignos não-melanoma são o tipo de câncer de maior incidência e prevalência no Brasil. Dentre eles, o carcinoma basocelular (CBC) é o mais comum, correspondendo entre 70% e 75% dos casos. O carcinoma epidermoide (CEC) responde por 20% dos casos. Este trabalho tem por objetivo analisar os casos de câncer de pele não-melanoma operados, entre os anos de 2005 e 2010, no Serviço de Cirurgia Plástica do Hospital Ipiranga.
MÉTODO: Foi realizada análise de prontuários de pacientes submetidos a exérese de carcinoma de pele não-melanoma em centro cirúrgico, avaliados quanto a idade, sexo, profissão, raça, localização anatômica, fatores de risco, número de lesões e subtipo histológico.
RESULTADOS: Foram analisados 145 pacientes, dos quais 15,9% apresentavam lesões múltiplas, totalizando 168 tumores. Houve predomínio de CBC, correspondendo a 87,6% dos casos, seguido de CEC, com 26,2%. Os CBCs sólidos ou nodulares predominaram, com 44,1%, e os CECs Broders I representaram 42,1% dos CECs. Dos pacientes, 80,7% possuíam lesão em face e 12,4%, em membros superiores. A média de idade dos pacientes foi de 69,5 anos, sendo 59,4% do sexo feminino. A raça branca foi mais frequente e o tabagismo foi o principal fator de risco, presente em 79,3% dos casos.
CONCLUSÕES: Observou-se predomínio de CBC e do sexo feminino nos pacientes estudados, demonstrando a tendência atual desse tumor. O número significativo de pacientes com lesões múltiplas ressalta a importância do exame periódico dessa população. A alta prevalência de tabagismo entre os pacientes não pode deixar de ser observada.
Palavras-chave: Carcinoma basocelular. Carcinoma de células escamosas. Carcinoma/cirurgia.
A higher incidence and prevalence of non-melanoma skin cancers has been reported in both men and women. Although these malignant skin cancers have low mortality rates and a low ability to generate metastases, they are locally destructive and lead to high morbidity rates.
Basal cell carcinoma (BCC), the most common skin cancer, accounts for 70%-75% of all cases. BCC is a high-grade malignant tumor that has the potential for local invasion, tissue destruction, and recurrence, but a limited ability to generate metastases1.
Squamous cell carcinoma (SCC) accounts for 20% of all skin cancers in the United States. Although rare, SCC can metastasize to the regional lymph nodes and other organs such as the bone, brain, and lungs2.
The main cause of BCC and SCC is chronic exposure to sunlight, which explains the frequent occurrence of lesions on areas of the body that are exposed to the sun, such as the face, ears, neck, scalp, shoulders, and back. In addition to burn scars and angiodermal ulcers, other etiological factors known to cause skin cancers include ultraviolet exposure, certain carcinogenic chemicals (arsenic and hydrocarbons), ionizing radiation, previous skin diseases such as xeroderma pigmentosum, Bazex and Gorlin syndromes, chronic irradiation or ulceration, and human papilloma virus (HPV) infection. Immunologically compromised patients are at higher risk of developing skin cancers2-4.
No premalignant conditions precede BCC, although hamartomas or sebaceous naevi may develop into this carcinoma. A total of 86% of BCC cases affect the head, whereas 7% affect the trunk and limbs. Skin cancers of the upper lip are frequently found to be BCC, whereas those of the lower lip tend to be SCC. SCC often develops on the face, hands, and forearms, and actinic keratosis is the most prevalent precursor lesion. SCC of the external auditory canal is the most common malignancy of the skin5.
Fair-skinned people often develop skin cancers, but they affect all ethnic groups, primarily those living in tropical areas that are highly exposed to the sun. Similarly, individuals with occupations that involve prolonged sun exposure, such as sailors, farmers, construction workers, and postal carriers, are at higher risk for developing skin cancer3,6. Malignant skin tumors are rare in children and, when present, are associated with underlying predisposing conditions7.
The involvement of cutaneous HPV in the pathogenesis of BCC and SCC is attributed to its anti-apoptotic activity and the ability to repair DNA defects of keratinocytes8. Smoking is an independent risk factor for SCC, although no increased risk was detected for BCC9.
Histologically, most cases of BCC seem to originate in the epidermis and hair follicles. Some authors suggest that BCC and SCC originate from the same pluripotent epithelial cell type and that certain factors, such as interaction with the stroma, determine the tumor type that develops10. BCC are divided into subtypes that have more or less aggressive behavior and are classified as nodular, micronodular, superficial, pigmented, cystic, infiltrative, and morpheaform. SCC resembles nests of abnormal epidermal cells invading the dermis, and its histological grade depends on the degree of cellular differentiation2.
From the clinical point of view, BCC is usually characterized by raised edges and the presence of a central pearly area with telangiectasia. BCC may present as peeled areas, atrophic regions, or fibrosis due to chronic inflammation2. BCC tends to grow slowly and develop as a single lesion, although simultaneous or subsequent lesions might be observed1,10. In contrast, SCC lesions show a nodular rigid plaque on the erythematous base with raised borders. A central ulcerated area may also be observed, whereas major lesions may appear along the infection2.
For the therapeutic treatment of BCC, several strategies may be recommended according to different factors such as age, the patient's medical condition, aesthetic result, anatomical location, size, and tumor borders in addition to histological pattern, number of lesions, and tumor classification (primary or recurrent). Therapeutic approaches include curettage, electrocautery, surgical resection, Mohs micrographic surgery, fluorouracil administration, radiotherapy, photodynamic therapy, and cryosurgery. Aspects and therapeutic approaches considered for SCC treatment are similar to those used for BCC treatment. However, factors related to potential metastasis or recurrence should also be assessed. In cases where the tendency for metastasis is high, the therapeutic approach involves resection of the lymph nodes and the assessment of metastases in other organs.
Although several treatments exist for skin cancer, post-surgical reconstruction is essential. Local flaps or grafts may repair the defects, although the latter provide worse outcomes due to the typical development of local depression and hyperpigmentation that is not observed in the neighboring tissues, which might lead to poor aesthetic results4.
Prognosis depends on tumor type and the chosen treatment. Risk factors associated with recurrence and metastasis include a lesion >2 cm in diameter in the central portion of the face or ears, a long-lasting lesion, incomplete resection, aggressive histological type, and perineural and perivascular invasion1.
The aim of this study was to analyze the patients who underwent surgical treatment for non-melanoma skin cancer between 2005 and 2010 at the Serviços de Cirurgia Plástica do Hospital Ipiranga (Plastic Surgery Services of Hospital Ipiranga).
METHODS
This case series includes patients who underwent surgical treatment for non-melanoma skin cancer between 2005 and 2010 at the surgical center of Hospital Ipiranga and excluded patients who underwent outpatient surgical lesion resection.
The medical records of the patients included in this study were reviewed for the following parameters: gender, age, race, occupation, anatomical location, risk factors, number of lesions, and histological subtype.
Recommended excision margins of 3 mm-5 mm were followed to resect the lesions without Mohs micrographic surgery. Post-surgical reconstruction was heterogeneous, although it was not assessed in this study.
According to histological type, BCC were classified as nodular or solid, micronodular, sclerodermiform, adenoid, ulcerated, superficial, or pigmented. Broders' classification was used for SCC according to the percentage of undifferentiated cells: grade I, well-differentiated; grade II, slightly differentiated; grade III, poorly differentiated; and grade IV, undifferentiated.
RESULTS
Between 2005 and 2010, 145 patients underwent non-melanoma skin cancer resection at the surgical center. A total of 22.8% of the patients presented with multiple lesions, resulting in a total of 168 tumors.
Among the patients, 127 (87.6%) had BCC, whereas 38 (26.2%) had SCC (23 patients had more than one kind of tumor, BCC and SCC). Of the 168 tumors, 75.5% were BCC, 22.7% were SCC, and 1.8% were other carcinomas.
A high female prevalence (59.4%) was observed in this study. The average patient age was 69.5 years. The race of 61.4% of the patients was not mentioned in the medical records. Among the patients for whom this information was available, Caucasians accounted for 35.2% of patients, whereas mulattos comprised 3.4%. No Africans participated in the study.
Smoking was the leading risk factor for non-melanoma skin cancers (present in 79.3% of the patients), followed by sun exposure (2.8%).
In a topographic evaluation of the lesions, the face was the most commonly affected; a total of 117 (80.7%) patients developed tumors in this region (Figure 1). Lesions in the upper limbs were observed in 18 (12.4%) cases, whereas 8 (5.5%) had lesions on the back, 7 (4.8%) had lesions on the chest, and 4 (2.8%) had lesions in the lower limbs.
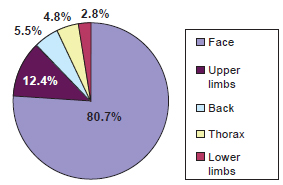
Figure 1 - Lesion topography.
In the group of patients analyzed, 112 (77.2%) presented with a single lesion, whereas 33 (22.8%) presented with multiple lesions.
Regarding BCC histological subtype, 44.1% of the patients presented with a solid or nodular BCC subtype, whereas 13.4% had sclerodermiform, 13.4% had micronodular, 8.66% had adenoid, 7.08% had ulcerated, 7.08% had superficial, and 2.36% had pigmented. Five (3.04%) patients did not have histologic subtypes identified (Figure 2).
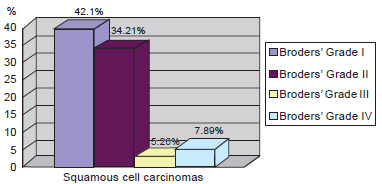
Figure 2 - Distribution of squamous cell carcinomas according to Broders' classification.
Among the SCC subtype, Broders' grade I was more common (Figure 2). In a more detailed analysis of the 38 SCC cases, 42.1% were classified as Broders' grade I, 34.21% were grade II, 5.26% were grade III, and 7.89% were grade IV and 10.53 did not have histologic subtypes identified (Figure 3).
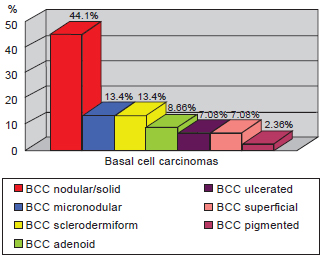
Figure 3 - Classification of basal cell carcinomas.
DISCUSSION
According to the literature, 75% of non-melanoma skin cancers are BCC and 20% are SCC. In this study, 75% of the lesions were due to BCC, whereas 22% were due to SCC; these findings are similar to those described in the literature. BCC with a solid or nodular histologic subtype was the most common, as noted in the literature. Among cases of SCC, Broders' grade I was the most frequent cancer and the malignant tumor with the best prognosis.
Although smoking is a risk factor related to SCC only, it was the main variable among the patients studied, as sun exposure was less representative. The predominance of Caucasians developing skin cancer confirms the findings described in the literature. With regard to topographic location, 80.7% of the patients presented with lesions on the face, which is similar to the value (86%) reported in earlier studies.
The peak incidence of BCC occurs around 40 years of age. However, the patients in this study had a higher average age (69.5 years).
CONCLUSIONS
The case series of non-melanoma skin cancers examined in this study showed epidemiological results similar to those found in the literature. Presumably, the encountered variations are due to the different profile of the patients analyzed and the fact that we excluded patients who underwent outpatient resection, which are simpler cases that may be frequently reported in the literature. The predominance of BCC and female gender in cancer development was detected among the patients evaluated - observations that reflect the current tendency of this tumor.
The significant number of patients with multiple lesions emphasizes the importance of periodic examination. In addition, high smoking rates were observed among the patients.
REFERENCES
1. Custódio G, Locks LH, Coan MF, Gonçalves CO, Trevisol DJ, Trevisol FS. Epidemiology of basal cell carcinomas in Tubarão, Santa Catarina (SC), Brazil between 1999 and 2008. An Bras Dermatol. 2010;85(6):819-26.
2. Culliford A, Hazen A. Dermatologia para cirurgiões plásticos. In: Thorne CH, Beasley RW, Aston SJ, Bartlett SP, Gurtner GC, Spear SL, eds. Grabb & Smith cirurgia plástica. 6ª ed. Rio de Janeiro:Guanabara Koogan; 2009. p.103-12.
3. Popim RC, Corrente JE, Marino JAG, Souza CA. Câncer de pele: uso de medidas preventivas e perfil demográfico de um grupo de risco na cidade de Botucatu. Cienc Saúde Coletiva. 2008;13(4):1331-6.
4. Park SW, Heo EP, Choi JH, Cho HC, Kim SH, Xu L, et al. Reconstruction of defects after excision of facial skin cancer using a venous free flap. Ann Plast Surg. 2011;67(6):608-11.
5. Netscher DT, Leong M, Orengo I, Yang D, Berg C, Krishnan B. Cutaneous malignancies: melanoma and non-melanoma types. Plast Reconstr Surg. 2011;127(3):37e-56e.
6. Sanabria Ferrand PA. Efectividad de um programa cognitivo social para prevenir el câncer de piel em mujeres adolescentes. Univ Psychol. 2006;5(3):585-97.
7. Tatiana KSC, Somers GR, Pope E, Zuker RM. Predisposing factors and outcomes of malignant skin tumors in children. Plast Reconstr Surg. 2010;126(2):508-14.
8. Nindl I, Gottschling M, Stockfleth E. Human papillomaviruses and non-melanoma skin cancer: basic virology and clinical manifestations. Dis Markers. 2007;23(4):247-59.
9. De Hertog SA, Wensveen CA, Bastiaens MT, Kielich CJ, Berkhout MJ, Westendorp RG, et al; Leiden Skin Cancer Study. Relation between smoking and skin cancer. J Clin Oncol. 2001;19(1):231-8.
10. Pimentel ERA, Góes LHFM. Tumores malignos da pele: carcinomas. In: Mélega JM, ed. Cirurgia plástica fundamentos e arte: princípios gerais. Rio de Janeiro: Guanabara Koogan; 2002. p.349-60.
1. Resident Plastic Surgeon at the Serviços de Cirurgia Plástica do Hospital Ipiranga (Plastic Surgery Services of Hospital Ipiranga), São Paulo, SP, Brazil.
2. Chief of the Serviços de Cirurgia Plástica do Hospital Ipiranga (Plastic Surgery Services of Hospital Ipiranga), full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery - SBCP), São Paulo, SP, Brazil.
3. Regent of the Serviços de Cirurgia Plástica do Hospital Ipiranga (Plastic Surgery Services of Hospital Ipiranga), full member of the SBCP, São Paulo, SP, Brazil.
4. Physician Preceptor at the Plastic Surgery Services of Hospital Ipiranga, full member of the SBCP, São Paulo, SP, Brazil.
Correspondence to:
José Octávio Gonçalves de Freitas
Av. Nazaré, 28
São Paulo, SP, Brazil - CEP 04262-000
E-mail: joseoctavio@ig.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: October 7, 2012
Article accepted: December 5, 2012
This study was performed at the Serviços de Cirurgia Plástica do Hospital Ipiranga (Plastic Surgery Services of Hospital Ipiranga), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter