

Original Article - Year 2012 - Volume 27 -
Simple and safe technique for nipple-areola reconstruction with intradermal tattoo
Técnica simples e segura para a reconstrução areolopapilar com tatuagem intradérmica
ABSTRACT
BACKGROUND: The final step in the creation of the neo-breast is reconstruction of the nippleareolar complex (NAC), which is aimed toward bringing the appearance of the NAC closer to that of the contralateral breast following mastectomy. NAC restoration has historically been a stepwise procedure, in which reconstruction of the nipple by the use of grafts or local flaps was followed by reconstruction of the areola to achieve the correct color. Currently, the popularity of the areolar tattoo is increasing compared to traditional techniques. The aim of this study was to describe the technique and equipment used for intra-dermal tattooing in mastectomized patients at the Plastic Surgery and Reconstructive Microsurgery Service of the Walter Cantídio University Hospital (Fortaleza, CE, Brazil).
METHODS: This study describes the steps of the repair procedure by using permanent areolar tattooing with conventional equipment from a professional tattoo artist. The procedure was used in 10 patients undergoing post-mastectomy breast reconstruction.
RESULTS: The advantages of this method included the technical simplicity of the procedure, the ability to use this procedure in outpatients, and the lack of morbidity of the donor areas.
CONCLUSIONS: Tattooing the NAC is a safe, fast procedure with low morbidity and good results of breast reconstruction.
Keywords: Tattooing. Nipples, surgery. Reconstructive surgical procedures.
RESUMO
INTRODUÇÃO: A reconstrução do complexo areolopapilar (CAP) constitui o passo final na criação da neomama, com o objetivo de aproximá-la da mama contralateral após a mastectomia. A restauração do CAP tem sido historicamente um procedimento feito em estágios, com a reconstrução da papila realizada por meio de enxertos ou retalhos locais, previamente, e da aréola, posteriormente, buscando a coloração adequada. Atualmente, a utilização da tatuagem areolar está alcançando popularidade cada vez maior, comparativamente às técnicas tradicionais. O objetivo deste trabalho é descrever a técnica e os equipamentos utilizados para a tatuagem intradérmica em pacientes mastectomizadas, realizada no Serviço de Cirurgia Plástica e Microcirurgia Reconstrutiva do Hospital Universitário Walter Cantídio (Fortaleza, CE, Brasil).
MÉTODO: O presente trabalho descreve os passos para a realização do procedimento reparador utilizando a tatuagem areolar permanente com equipamento convencional de tatuagem artística profissional. O procedimento foi aplicado em 10 pacientes submetidas a reconstrução mamária pós-mastectomia.
RESULTADOS: O método demonstrou as vantagens da simplicidade técnica do procedimento, não requerendo internamento nem resultando em morbidade de áreas doadoras.
CONCLUSÕES: A tatuagem do CAP é um procedimento seguro, rápido, com baixa morbidade e bons resultados na finalização da reconstrução mamária.
Palavras-chave: Tatuagem. Mamilos, cirurgia. Procedimentos cirúrgicos reconstrutivos.
Restoration of the nipple-areolar complex (NAC) is becoming increasingly important in post-mastectomy breast reconstruction. The NAC has great symbolic significance for women, and it is an essential part of the breast1. Several studies have shown that reconstructing the NAC has a positive influence on the recovery process from the damages to both physical and mental health inherent to breast cancer treatment2.
After the neo-breast is constructed with perfect symmetry relative to the contralateral breast, NAC reconstruction is the final part of the restoration process3. The main parameters of a successful NAC reconstruction are symmetry, position, size, projection, texture, and color4. Although various surgical techniques are available for the reconstruction of both the nipple and the areola, the final color of the NAC is rarely close to that of the contralateral breast, except when the nipple is grafted from the opposite breast3-5.
The areola's pigmentation and texture are the subjects of various recent studies that seek permanent and natural reconstruction results. Snyderman and Guthrie6 have proposed the use of flaps from the contralateral areola in reconstructed NAC repair. However, contralateral nipple and areola grafts, in spite of their advantage in terms of symmetry with the original tissue, result in considerable morbidity of the donor area. Although Gruber7 stated that these procedures do not significantly affect the sensitivity of the donor nipple, the potential adverse effect of this procedure should not be overlooked. This technique is currently used selectively when preparation of local flaps cannot be safely performed, such as in patients with a hypertrophied nipple or a thin skin cover in cases of alloplastic reconstruction3-5.
Several donor areas have been described as suitable for NAC reconstruction. Adams8 introduced total skin grafting from the labia minora for areola restoration. Later, the labia majora were also used, but the disadvantages of this technique were the unpopularity of the donor area and the frequently hyperpigmented color. Moreover, inguinal perineal skin was used for grafting darker NACs. The inner upper thigh has become a popular donor site because it provides darker tones than breast skin and is less hyperpigmented than the labial mucosa. In lighter NACs, grafts from the retroauricular upper lip and oral mucosa have been described, which provide a pinkish color. Exposure to UV light has also been used in an attempt to increase the pigmentation of these grafts, but the results were not permanent. In spite of the attempts to predict and control pigmentation in these cases, results similar to those of the contralateral NAC are seldom obtained3-5.
NAC saving or NAC banking consists of the attempt to implant the NAC removed from the mastectomized breast into the abdominal, inguinal, or buttocks area followed by subsequent transfer to the neo-breast. In spite of the criticism surrounding the possibility of neoplastic dissemination, some authors have defended cryopreservation and histopathological testing of the specimen before tissue grafting. However, this technique did not yield encouraging results, with inappropriate pigmentation and loss of nipple projection3.
Dermabrasion, another technique that was tested on black patients, produced regular pigmentation of the areola, but the results were not long term3.
It is within the context of this difficulty in obtaining adequate NAC color that intradermal tattooing has been gaining ground in plastic surgery.
Although artistic tattooing has been known for millennia, it was only recently introduced in medical practice. Bunchman et al.9 described the use of tattooing in NAC reconstruction of burn patients. Rees10 was the first to report pigmentation by tattooing the areola in post-mastectomy breast reconstruction. Initially, areolar tattooing was used as a complementary technique to skin grafting following tone loss, but Elliott and Hartrampf11 began using it as a standalone procedure in areola preparation since the 1990s. Tattooing can also be used to correct discrepancies in the format, size, or location of the reconstructed NAC3,5.
Pigmentation through tattooing is a simple, low-cost outpatient procedure that does not cause morbidity of the donor areas and shows a low rate of complications such as allergies and infections3-5.
In the past, emulsions with a dense base containing colored pigments were used. The current availability of several pigment tones similar to the areolar skin color has provided results that are more natural. Masser et al.12 introduced the gel-suspended pigment technique, which achieves natural results with fewer reactions and therefore prevents a painted appearance. When introduced in the dermis, these pigments show a distribution pattern similar to that of melanin in melanocytes and hemoglobin in the skin capillaries. Spears and Arias13 reported a minimal prevalence of skin reactions to titanium dioxide and ferrous oxide pigments, stating that NAC tattooing with these components is completely safe in patients with healthy skin3,5.
The aim of this study was to describe the technique and equipment used for intradermal tattooing in mastectomized patients at the Plastic Surgery and Reconstructive Microsurgery Service of the Hospital Universitário Walter Cantídio (Fortaleza, CE, Brazil).
METHODS
Breast reconstruction was performed immediately before NAC reconstruction by using a conventional technique with autologous flaps or implants. Preparation of the nipple flap took place 6 months after the mastectomy with reconstruction or mastopexy of the contralateral breast in cases requiring symmetrization. Intradermal tattooing was performed 6 to 12 weeks after preparation of the nipple.
Pigmentation was performed using a professional artist's electric tattoo machine (Figure 1). Flat-type, brush-shaped needles were welded together in a group of 15 needles for use. Disposable tattoo gun tips and ink cup holders were used in the procedure (Figures 2 and 3).
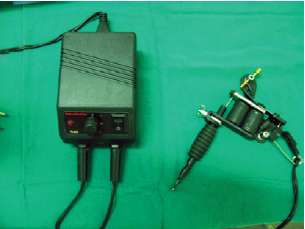
Figure 1 - Electric machine for indelible artistic tattooing.

Figure 2 - Disposable needle and tip.
Figure 3 - Disposable ink cup holders used to separate the inks of the selected color palette.
The patient was examined in the sitting position and the size, shape, and position were marked in relation to the contralateral breast. The areolar mold was prepared with a bottle of saline and the measures were transferred to the reconstructed breast (Figure 4). The color was assessed and pigments with similar tones were distributed across the ink cup holders. A mix of brown, chocolate, white, and rose pigments was used.

Figure 4 - Assessment of the contralateral areola shape and preparation of the mold with a saline bottle for transposing the measures to the opposing breast.
Breast antisepsis was performed with a transparent alcohol solution and a local anesthetic with 2% lidocaine combined with a vasoconstrictor agent was subsequently applied (Figure 5). Thus, the procedure became more comfortable for the patient and the skin bleeding was reduced, facilitating the visualization of the applied pigments (Figure 6).

Figure 5 - Local anesthetic procedure following antisepsis with alcohol solution.

Figure 6 - Immediate result after the procedure, showing ecchymosis and skin bleeding.
A few minutes after starting the procedure, the skin became erythematous and discrete skin bleeding was visible, mainly in the areas of previous scars.
The various inks of light and dark tones were applied in homogeneous layers onto the areola in the attempt to achieve the color of the contralateral areola. Darker tones were used on the nipple. Excess pigments that did not penetrate the dermis were removed from the skin by using alcohol.
Following the procedure, a dressing with a wound healing ointment (dexpanthenol) and polyvinyl chloride (PVC) film was applied (Figure 7). Patients were instructed to keep the NAC dry for 48 h.

Figure 7 - Dressing with wound healing ointment and PVC film.
RESULTS
The technique described herein was applied in 10 patients undergoing post-mastectomy breast reconstruction.
Nine patients underwent immediate reconstruction with a transverse rectus abdominis myocutaneous flap and 1 patient underwent temporary extensor apposition followed by subsequent replacement with a sub-chest breast implant.
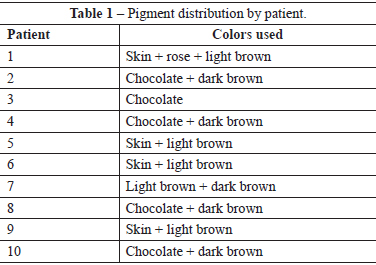
Prior to preparing the NAC, 5 patients underwent contralateral breast symmetrization. Chocolate and brown tones were used in the darker to black areolas and pink, skin, and light brown tones were used in Caucasian patients (Table 1).
No allergic reactions occurred and only 1 patient showed cellulitis, which was quickly resolved with systemic antibiotherapy.
Several of the cases in this study are shown in Figures 8 to 10.

Figure 8 - Late result in a Caucasian patient.

Figure 9 - Late result in a nipple-areolar complex of intermediate color.

Figure 10 - Result in a patient with a dark nipple-areolar complex in an irradiated breast.
DISCUSSION
Preparing the NAC and the subsequent pigmentation through intradermal tattooing is an increasingly common procedure performed by plastic surgeons because a specialized and precise prior assessment is required for the desired outcome of perfect symmetry between the reconstructed and the contralateral breast.
The patients who undergo this procedure have common risk factors such as lymphadenectomy, scars, implants, and previous chemotherapy and local radiotherapy that may result in physiopathological locoregional alterations and require special care. Thus, pigmentation of the reconstructed breast becomes a process worthy of special care.
The skin can be tattooed before or after nipple preparation, depending on the surgeon's preference. A minimum gap of 6 to 12 weeks must be observed when this procedure is performed after reconstruction in order to allow the nipple to stabilize and contract. Several authors have reported results that are more homogeneous with better color distribution when skin pigmentation is performed prior to elevation of the breast flap.
NAC reconstruction and simultaneous tattooing have been described in the literature. In this study, tattooing was performed only after elevation of the breast flap because this prevents additional trauma and the resulting scars become disguised through subsequent pigmentation over the surgical site. Differences in relief did not make nipple pigmentation difficult2-5.
The tattooing technique requires training and experience in order to obtain good results. The depth of the pigment in the skin is an important parameter because the pigment can be lost with scaling of the epidermis if it is placed too superficially, whereas the deeper pigments are carried away by lymphatic vessels. Both situations cause the tattoo to become faded2-5. The patient must be instructed not to remove the crusts because this may clear away the pigments.
Histological studies have revealed pigment deposition in the epidermis and in various levels of the dermis. After a few days, the epidermis usually scales and only the dermal pigments remain. After 7 to 10 days, the tattoo site heals and the dermal pigments accumulate in the perivascular space in macrophages and in the extracellular matrix in collagen fibers. At this stage, the tattoo is still dark and distinct. Phagocytes absorb the particles after a few months, resulting in the slow fading of colors and less pronounced margins. The pigments eventually reside in the superficial dermis, mainly inside the cell membranes of fibroblasts. At that time, the pigments are no longer found in macrophages, melanocytes, or in the intercellular space. These findings show that the tattoo color stabilizes after only a few months and is determined by the remaining pigments embedded in fibroblasts2-5.
Tattoo machines specifically for medical use have been developed. The conventional artist tattoo machine that we used in this study proved to be as safe as the machines developed for medical use, and had the advantages of a lower cost and the ability to use of several types of needles, which facilitated the procedure. The material should be selected according to the surgeon's preference5.
Local application of antibiotics was recommended in several studies, and Spears and Arias13 defended the use of systemic antibiotherapy for 48 h. In this study, local or systemic prophylactic antibiotics were not used because an aseptic technique was adopted to avoid bacterial dissemination.
Edema and ecchymosis usually recede after 1 week, allowing an initial assessment of the colors. Secondary retouching may be required in cases in which fading occurs after some months. In rare cases, the initial color is retained for several months3-5.
CONCLUSIONS
Tattooing the NAC is a safe and fast procedure that produces low morbidity and good results in breast reconstruction finalization. The resulting areola shows regular edges with colors similar to those of the contralateral NAC. The procedure rarely causes discomfort, reactions, or infections when it is performed properly by following basic aseptic and antiseptic techniques.
REFERENCES
1. Tostes ROG, Silva KDA, Andrade Júnior JCCG, Ribeiro GVC, Rodrigues RBM. Reconstrução do mamilo por meio da técnica do retalho C-V: contribuição à técnica. Rev Soc Bras Cir Plást. 2005;20(1):36-9.
2. Mohamed SA, Parodi PC. A modified technique for nipple-areola complex reconstruction. Indian J Plast Surg. 2011;44(1):76-80.
3. Farhadi J, Maksvytyte GK, Schaefer DJ, Pierer G, Scheufler O. Reconstruction of the nipple-areola complex: an update. J Plast Reconstr Aesthet Surg. 2006;59(1):40-53.
4. Murphy AD, Conroy FJ, Potter SM, Solan J, Kelly JL, Regan PJ. Patient satisfaction following nipple-areola complex reconstruction and dermal tattooing as an adjunct to autogenous breast reconstruction. Eur J Plast Surg. 2010;33(1):29-33.
5. Saad JF. Reconstrução do complexo aréolo-papilar com retalho em fechadura associado à pigmentação com tatuagem [dissertação de mestrado]. São Paulo: Universidade de São Paulo, Faculdade de Medicina; 2001. 102p.
6. Snyderman RK, Guthrie RH. Reconstruction of the female breast following radical mastectomy. Plast Reconstr Surg. 1971;47(6):565-7.
7. Gruber RP. Nipple-areola reconstruction: a review of techniques. Clin Plast Surg. 1979;6(1):71-83.
8. Adams WM. Labial transplant for correction of loss of the nipple. Plast Reconstr Surg. 1949;4(3):295-8.
9. Bunchman HH 2nd, Larson DL, Huang TT, Lewis SR. Nipple and areola reconstruction in the burned breast. The "double bubble" technique. Plast Reconstr Surg. 1974;54(5):531-6.
10. Rees TD. Reconstruction of the breast areola by intradermal tattooing and transfer. Case report. Plast Reconstr Surg. 1975;55(5):620-1.
11. Elliott LF, Hartrampf CR Jr. Breast reconstruction: progress in the past decade. World J Surg. 1990;14(6):763-75.
12. Masser MR, Di Meo L, Hobby JA. Tattooing in reconstruction of the nipple and areola: a new method. Plast Reconstr Surg. 1989;84(4):677-81.
13. Spear SL, Arias J. Long-term experience with nipple-areola tattooing. Ann Plast Surg. 1995;35(3):232-6.
1. Plastic surgeon, full member of the Sociedade Brasileira de Cirurgia Plástica /Brazilian Society of Plastic Surgery (SBCP), coordinator of the Plastic Surgery and Reconstructive Microsurgery Service of the Hospital Universitário Walter Cantídio (HUWC), Fortaleza, CE, Brazil.
2. Resident physician of Plastic Surgery at the Plastic Surgery and Reconstructive Microsurgery Service of the HUWC, Fortaleza, CE, Brazil.
3. Plastic surgeon, specialist member of the SBCP, medical officer at the Plastic Surgery and Reconstructive Microsurgery Service of the HUWC, Fortaleza, CE, Brazil.
4. Plastic surgeon, full member of the SBCP, medical officer at the Plastic Surgery and Reconstructive Microsurgery Service of the HUWC, Fortaleza, CE, Brazil.
5. Undergraduate student of Medicine at the Universidade Federal do Ceará, member of the Academic League of Plastic Surgery, Fortaleza, CE, Brazil.
Correspondence to:
Juliana Régia Furtado Matos
Rua Mombaça, 164 - Aldeota
Fortaleza, CE, Brazil - CEP 60160-190
Email: julianarfm@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: May 31, 2012
Article accepted: August 21, 2012
This study was performed at the Plastic Surgery and Reconstructive Microsurgery Service of the Hospital Universitário Walter Cantídio (HUWC), Fortaleza, CE, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter