ABSTRACT
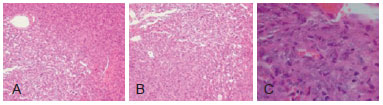
Hemangiopericytomas are rare tumors arising from the proliferation of pericytes. They may be found in the lungs, bones, skull, deep soft tissue or limbs. The tumor has an unpredictable prognosis and when it affects the orbital region, may have an aggressive behavior, with high incidence of recurrence. We report a case of orbital hemangiopericytoma and highlight clinical, surgical, and histopathological features of these tumors. Orbital hemangiopericytomas usually are solid, slow-growing tumors. They should be considered in the differential diagnosis of well-defined orbital masses along with epidermoid cysts, schwannomas, neurofibromas, fibrous histiocytomas, lipomas, and vascular malformations. The diagnosis is confirmed by anatomopathologic examination and sometimes complemented by immunohistochemistry. Complete excision of the tumor with wide margins is usually curative; however, radiotherapy and chemotherapy may be required for recurrent lesions.
Keywords:
Hemangiopericytoma. Neoplasms, vascular tissue. Orbit/surgery.
RESUMO
Hemangiopericitomas são tumores raros originados a partir da proliferação de pericitos, ou seja, células que envolvem os capilares. São encontrados em ossos, pulmões, crânio, partes moles profundas ou membros inferiores, principalmente na coxa. É considerado um tumor com potencial de malignidade incerto e quando afeta a região orbitária pode apresentar um comportamento biológico agressivo, com grande chance de recidiva. O objetivo deste trabalho é relatar um caso de hemangiopericitoma orbital e destacar suas características clínicas, cirúrgicas e histopatológicas. Usualmente, os hemangiopericitomas da órbita são tumores sólidos, únicos e de crescimento lento. Devem ser lembrados no diagnóstico diferencial dos tumores orbitários bem delimitados, como cistos epidermoides, schwannomas, neurofibromas, fibro-histiocitomas, lipomas e malformações vasculares. A confirmação diagnóstica é realizada pelo exame anatomopatológico e, por vezes, complementada pelo estudo imuno-histoquímico. O tratamento deve ser realizado com exérese completa do tumor, com margens amplas, sendo a radioterapia e a quimioterapia reservadas para casos de lesões reincidentes.
Palavras-chave:
Hemangiopericitoma. Neoplasias de tecido vascular. Órbita/cirurgia.