ABSTRACT
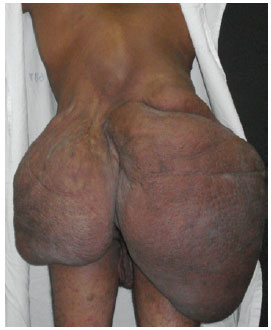
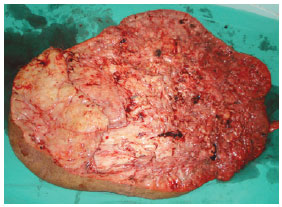
Neurofibromatosis is a disease of genetic origin with autosomal dominant inheritance that is classified into 3 types: neurofibromatosis type I (NF1), neurofibromatosis type 2 (NF2), and schwannomatosis. The main characteristics of NF1 are caféaulait spots, dermal and plexiform neurofibromas, false dermal and plexiform neurofibromas, false axillary or inguinal ephelides, and Lisch nodules. This study describes the case of a 26year-old man who presented with small cutaneous nodules, present since he was 3 years old, and caféaulait spots of different sizes distributed diffusely. At the age of 13, the patient developed a mass in the back and abdomen that subsequently developed into a rapidly growing voluminous mass, which hindered walking and caused social isolation. The surgical treatment consisted of the excision of the tumor in 2 phases, with a 2month interval between procedures. Although a cure for neurofibromatosis has not been discovered, surgical removal is indicated in cases of neurological involvement, pain, disfigurement, possible involvement of adjacent structures, and suspicion of malignancy. Partial resection is acceptable if total removal is not possible. In the present case, surgical treatment was an excellent choice because it enabled the complete excision of the lesion, with satisfactory wound healing and aesthetic results, as well as the improvement of the quality of life of the patient.
Keywords: Neurofibromatoses. Neurofibroma. Cafeaulait spots.