

Original Article - Year 2012 - Volume 27 -
Treatment of facial burn sequelae using fractional CO2 lasers in patients with skin phototypes III to VI
Tratamento de sequelas de queimadura de face com laser de CO2 fracionado em pacientes com fototipos III a VI
ABSTRACT
BACKGROUND: Reports on improvement in post-traumatic or pathological scars with the use of fractional CO2 laser (CO2F) conclude that it is a safe and effective technology, though used only in patients with phototypes II to III. The aim of this study was to evaluate the effectiveness of CO2F in patients with facial burn sequelae with phototypes III to VI.
METHODS: A total of 14 patients (average age, 29 years) with facial burn sequelae and phototypes III to VI were subjected to a CO2F laser treatment. After 2 months, the burns were evaluated using a 6-parameter scale, including color, texture, hydration, surface irregularities, volume, and distensibility.
RESULTS: The average durations of pain, edema, and hyperemia were 19 hours, 1.3 days, and 6.5 days, respectively. The fall of crusts was completed between 5 and 36 days with an average of 13.4 days. Two months after the session, 5 patients developed punctiform hypochromia in a checkerboard pattern corresponding to the points of laser ablation. The subjective satisfaction of the evaluators (i.e., both patients and physicians) with the treatment was 84.6%. The patients reported improvements in surface irregularities, distensibility, and skin texture (57% of the cases); hydration (43%); volume (28%); and color (14%). Meanwhile, the doctors reported improvements in surface irregularities and distensibility (43%).
CONCLUSIONS: The treatment with CO2F laser with mild parameters was well tolerated and resulted in high satisfaction rates for patients with facial burn sequelae as well as improved skin texture, distensibility, and surface irregularities. The high incidence of hypopigmentation must be considered while prescribing CO2F laser treatment to patients with phototypes IV to VI.
Keywords: Burns/complications. Carbon dioxide. Laser therapy/methods.
RESUMO
INTRODUÇÃO: Relatos sobre melhora em cicatrizes pós-traumáticas ou patológicas com o uso do laser de CO2 fracionado (CO2F) concluem tratar-se de tecnologia segura e efetiva, apesar de utilizado apenas em pacientes com fototipos II a III. O objetivo deste estudo foi avaliar a eficácia do CO2F em pacientes com sequela de queimadura facial com fototipos III a VI.
MÉTODO: No total, 14 pacientes, com média de idade de 29 anos, portadores de sequela de queimadura facial e fototipos III a VI, foram submetidos a uma aplicação do laser de CO2F. Após dois meses, a queimadura foi avaliada por meio de escala com 6 parâmetros: cor, textura, hidratação, irregularidades de superfície, volume e distensibilidade.
RESULTADOS: A duração média da dor foi de 19 horas; do edema, 1,3 dia; e da hiperemia, 6,5 dias. A queda das crostas finalizou entre 5 dias e 36 dias, com média de 13,4 dias. Dois meses após a sessão, 5 pacientes evoluíram com hipocromia puntiforme no padrão quadriculado correspondente aos pontos de ablação do laser. A satisfação subjetiva dos avaliadores (pacientes e médicos) com o tratamento foi de 84,6%. Para os pacientes, houve melhora das irregularidades de superfície, da distensibilidade e da textura da pele (57% dos casos), da hidratação (43%), do volume (28%) e da cor (14%). Para os médicos, houve melhora das irregularidades de superfície e da distensibilidade (43%).
CONCLUSÕES: O tratamento com laser de CO2F com parâmetros suaves foi bem tolerado e apresentou alto índice de satisfação em pacientes com sequela de queimadura facial, com melhora de textura, distensibilidade e irregularidades de superfície. A alta incidência de hipopigmentação é um fator a ser considerado na indicação do laser de CO2F em pacientes com fototipos IV a VI.
Palavras-chave: Queimaduras/complicações. Dióxido de carbono. Terapia a laser/métodos.
Whether restored spontaneously or grafted, the skin exhibits permanent changes after burns, especially a reduction in the number of appendages. Changes in collagen and elastic fibers as well as differences in the composition of the extracellular matrix lead to a loss of skin mechanical properties; clinically, this means reduced distensibility, especially in hypertrophic scars1.
The improvement of the quality of post-burn skin, which is usually dry, scaly, dyschromic, and inelastic, can help improve patients' self-esteem and quality of life2.
In recent last years, fractional ablative lasers, especially fractional (CO2F) carbon dioxide (CO2) lasers, have gained acceptance as the preferred method for skin resurfacing. They minimize wrinkles, photoaging, acne scars, and sagging skin without the disadvantages or risks associated with prolonged epithelialization after use of traditional ablative lasers, such as prolonged erythema, hypopigmentation, and even scars. With CO2F lasers, a large part of the skin remains intact around the microablation columns3.
Recently, reports on the improvement of non-acne scars, including keloids, using CO2F lasers have appeared in the literature4-6. In atrophic scars, CO2F lasers reduced the depth of scars by 35.6%-that is, they improved the "volume" of surface irregularities7. In 2 cases of burn sequelae, the use of CO2F lasers resulted in contracture relaxation and improved skin surface irregularities, texture, and color8. In post-traumatic and pathological scars, CO2F lasers are reported to improve texture, tone, and skin appearance with a low incidence of dyschromia; the authors conclude that it is a safe and effective technology for the treatment of scars, although the method has been used only in patients with skin phototypes II and III4.
Despite the existence of studies on the use of CO2F lasers in Asian people8, there is no report on their use in patients with phototypes V and VI. However, the product manuals for laser devices present parameters for use in these patients. Furthermore, there is no existing report on the use of the Smartxide Dot® (Deka, Florence, Italy) device, which is commonly used by physicians for treating scars or burn sequelae.
Therefore, the aim of this study was to evaluate the effectiveness of CO2F lasers in treating patients with facial burn sequelae with phototypes III to VI and determine parameters for safe use in these patients.
METHODS
Fourteen facial burn sequelae patients were selected; 12 (85.7%) were female, and 2 (14.3%) were male. Their ages ranged from 17 to 50 years (average, 29 years).
The average interval between the burn and the procedure was 19 years, ranging from 3 to 43 years.
Patients with restored tegument after second-degree burns or with grafts that exhibited dyschromia or surface irregularities were included.
All patients were followed-up at the institution for at least 3 months; they were required to use a night cream with tretinoin 0.015% to 0.05% and hydroquinone 2% to 4%, and a sunscreen with a sun protection factor of 30 or higher during the day2.
All patients signed a consent form prior to study participation.
One out of the 14 individuals included in the study did not carry out the treatment on the entire face because after performing a test in a periauricular area of 2 cm2, the patient developed significant hypochromia. The remaining 13 patients were subjected to the laser on the entire area affected by burn sequelae.
The classification of the skin phototype according to Fitzpatrick ranged from III to VI (Figure 1).
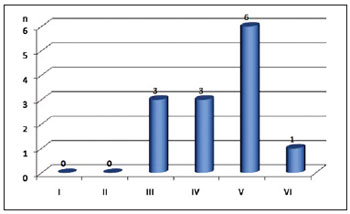
Figure 1 - Number of patients by skin phototype. n = number of patients.
Laser parameters
A CO2F Smartxide Dot laser was used.
One hour before the application, the patients received 1 g dipyrone orally.
The CO2F laser was applied using a cold-air blast to reduce pain sensitivity (Freddo® - Fabinject, Taubaté, SP, Brazil).
The parameters used for the session were stack 1 (single shot), 30 W power, spacing (Sp) 1.000 µm, and dwell time (DT) or exposure time of 500 µs.
Clinical evolution
The following parameters were evaluated:
a) Pain score, using a scale from 0 to 10
b) Duration of pain
c) Duration of edema
d) Duration of hyperemia
e) Time for crusts to fall off
f) Presence of dyschromia
g) Presence of itching or other symptoms
The initial follow-up period in this pilot study was 2 months, followed by weekly follow-ups until complete epithelialization and monthly follow-ups thereafter. The present patients will be followed-up for 1 year.
Scar evaluation method
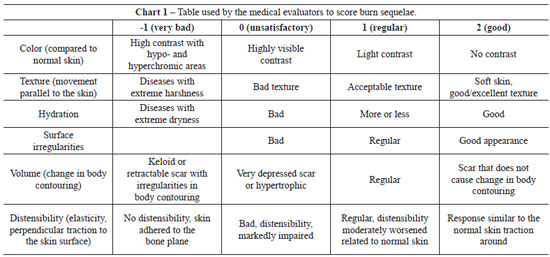
Burns were evaluated by the patients and 3 medical staff members by using a 6-parameter scale, including color, texture, hydration, surface irregularities, volume, and distensibility.
Each parameter was scored from 0 to 3 as follows: 0 = "unsatisfactory," 1 = "regular", and 2 = "good." The medical evaluators were provided with an explanatory table to guide the scoring of each parameter (Chart 1). For some parameters, extreme cases could receive a score of -1, which corresponded to "very bad." The sum of the scores of each parameter was taken as the final score, which ranged from 0 to 12.
The medical evaluation score was obtained by averaging the scores of the 3 medical evaluators.
RESULTS
On a scale from 0 to 10, the average pain reported by patients during laser application was 5.2. The average duration of pain or burning was 19 hours, ranging from 3 hours in 8 patients to 2-3 days in 5 patients.
Facial edema developed in 9 patients, and persisted on an average for 1.3 days. The average time of hyperemia was 6.5 days. The crusts started to fall at 2 days, and all crusts fell between 5 and 36 days (average, 13.4 days).
Three patients reported pruritus during the phase when the crusts were falling off. One patient had an allergic reaction during this period, probably related to the sunscreen used, with good resolution after 15 days. This was the only patient who would not submit to a new session of treatment because she considered the post-treatment very uncomfortable.
Two months after the completion of the session, 5 patients developed hypochromia characterized by the presence of multiple discrete points of hypochromia in a checkerboard pattern corresponding exactly to the points of injury made by the laser. Among the patients who developed hypochromia, 2, 2, and 1 were phototype IV, V, and VI, respectively (Figure 2). One of the patients with phototype IV did not complete the session because hypochromia was observed after a test in a 2-cm2 periauricular area, which is considered an area of high intensity as mentioned earlier.

Figure 2 - Patient with skin phototype VI, with points of hyperchromia after treatment.
The mean evaluation scores of the patients were 7 and 7.6 before and after the treatment, respectively. The average medical assessment score increased from 5.3 to 6.8. Skin surface irregularities, distensibility, and texture improved in 57% of the cases, hydration in 43%, volume in 28%, and color in 14%. The scores of the medical evaluators revealed improved skin surface irregularities and distensibility in 43% of the cases and improvement of skin texture, hydration, color, and volume in 28% of the cases. The rate of subjective satisfaction of the evaluators (i.e., both patients and physicians) with the treatment was 84.6% (Figure 3).

Figure 3 - A 23-year-old patient before and 2 months after fractional CO2 laser treatment.
DISCUSSION
This pilot study revealed important aspects to guide future protocols of burn sequelae treatment. The subjective satisfaction rate of the patients and doctors of 84.6%, especially regarding the improvement in texture, hydration, and distensibility of the post-burn tegument and smoothing of surface irregularities, is emphasized.
However, the scale used in the present study was not sensitive enough to measure satisfaction because "some improvement" in one of the requirements may not be enough to change a score from 1 to 2.
The parameters listed in the manual for the use of the laser on scars and keloids are 30 W power, Sp 600 µm (30% of injury with 70% of skin preserved), and DT ranging from 1.000 µs (phototype I) to 500 µs (phototype V). These parameters were considered to be very aggressive during the design of this study; thus, we opted to widen the Sp to 1.000 µm (ablation of 10% of the treated area) and use a DT of 500 µs (less deep injury); this turned out to be effective. The epithelialization time of 13.4 days is higher than those observed for rejuvenating treatments or acne sequelae; this is due to the smaller number of skin appendages in burn sequelae.
Even though the parameters of ablation were considered to be mild, 35.7% of cases exhibited hypochromia. A previous study reports a hyperchromia rate of 11.1% 6 months after CO2F laser application9.
The patients in the present study will be followed-up for 1 year with topical treatment. The late evolution will determine whether the treatment with the CO2F laser is in fact safe as postulated.
We suggest the use of even milder parameters in patients with phototypes IV to VI as well as the performance of a treatment test on a small area. Even the 4 patients who developed hypochromia expressed satisfaction with the improvement in other skin aspects, including medical evaluation. Punctiform hypochromia was considered to be very discrete by patients and more easily camouflaged than the surface irregularities.
All patients expressed a desire to be part of the full duration of this study, which includes 3 sessions.
The mechanical properties of the burn sequelae are thought to have improved because the CO2 laser modulated tissue repair, resulting in increased basic fibroblast growth factor (bFGF) and suppressed secretion of transforming growth factor β1 (TGFβ1). Thus, CO2 lasers simultaneously promote cell replication and have the potential to balance collagen organization against excessive fibrosis, preventing aberrant tissue repair10,11. Cytokine secretion after CO2F laser treatment was different from the secretory pattern observed after tissue injury. The presence of subsequent bFGF secretion in contrast to TGFβ1 reduction until the 30th day confirms that the injury induced by this laser is much more physiological as compared to that observed in hypertrophic scars3.
CONCLUSIONS
The treatment with the CO2F laser with mild parameters was well tolerated and resulted in high satisfaction rates in patients with facial burn sequelae with apparent improvement in skin texture, distensibility, and surface irregularities. The high incidence of hypopigmentation must be considered when considering this treatment for patients with phototypes IV to VI.
REFERENCES
1. Dematte MF, Gemperli R, Salles AG, Dolhnikoff M, Lanças T, Saldiva PH, et al. Mechanical evaluation of the resistance and elastance of post-burn scars after topical treatment with tretinoin. Clinics. 2011;66(11):1949-54.
2. Salles AG, Gemperli R, Toledo PN, Ferreira MC. Combined tretinoin and glycolic acid treatment improves mouth opening for postburn patients. Aesthetic Plast Surg. 2006;30(3):356-62.
3. Prignano F, Campolmi P, Bonan P, Ricceri F, Cannarozzo G, Troiano M, et al. Fractional CO2 laser: a novel therapeutic device upon photobiomodulation of tissue remodeling and cytokine pathway of tissue repair. Dermatol Ther. 2009;22 Suppl 1:S8-15.
4. Cervelli V, Gentile P, Spallone D, Nicoli F, Verardi S, Petrocelli M, et al. Ultrapulsed fractional CO2 laser for the treatment of post-traumatic and pathological scars. J Drugs Dermatol. 2010;9(11):1328-31.
5. Scrimali L, Lomeo G, Nolfo C, Pompili G, Tamburino S, Catalani A, et al. Treatment of hypertrophic scars and keloids with a fractional CO2 laser: a personal experience. J Cosmet Laser Ther. 2010;12(5):218-21.
6. Cho SB, Lee SJ, Chung WS, Kang JM, Kim YK. Treatment of burn scar using a carbon dioxide fractional laser. J Drugs Dermatol. 2010;9(2):173-5.
7. Weiss ET, Chapas A, Brightman L, Hunzeker C, Hale EK, Karen JK, et al. Successful treatment of atrophic postoperative and traumatic scarring with carbon dioxide ablative fractional resurfacing: quantitative volumetric scar improvement. Arch Dermatol. 2010;146(2):133-40.
8. Whang SW, Lee KY, Cho SB, Lee SJ, Kang JM, Kim YK, et al. Burn scars treated by pinhole method using a carbon dioxide laser. J Dermatol. 2006;33(12):869-72.
9. Chan NP, Ho SG, Yeung CK, Shek SY, Chan HH. Fractional ablative carbon dioxide laser resurfacing for skin rejuvenation and acne scars in Asians. Lasers Surg Med. 2010;42(9):615-23.
10. Nowak KC, McCormack M, Koch RJ. The effect of superpulsed carbon dioxide laser energy on keloid and normal dermal fibroblast secretion of growth factors: a serum-free study. Plast Reconstr Surg. 2000;105(6):2039-48.
11. Manolis EN, Kaklamanos IG, Spanakis N, Filippou DK, Panagiotaropoulos T, Tsakris A, et al. Tissue concentration of transforming growth factor beta1 and basic fibroblast growth factor in skin wounds created with a CO2 laser and scalpel: a comparative experimental study, using an animal model of skin resurfacing. Wound Repair Regen. 2007;15(2):252-7.
1. Doctorate from Faculdade de Medicina da Universidade de São Paulo (Medicine College of São Paulo University), coordinator of the Cosmetic and Laser Group of Plastic Surgery Discipline of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Clinical Hospital of the Medicine College of São Paulo University) - HCFMUSP, full member of the Sociedade Brasileira de Cirurgia Plástica (Brazilian Society of Plastic Surgery) - SBCP, São Paulo, SP, Brazil.
2. Full member of the SBCP, plastic surgeon, contributor of the Cosmetic and Laser Group of Plastic Surgery Discipline of the HCFMUSP, São Paulo, SP, Brazil.
3. Associate member of the SBCP, plastic surgeon, contributor of the Cosmetic and Laser Group of Plastic Surgery Discipline of the HCFMUSP, São Paulo, SP, Brazil.
4. Full member of the SBCP, full professor of Plastic Surgery Discipline of the Medicine College of São Paulo University, head of Plastic Surgeries and Burns Division of HCFMUSP, São Paulo, SP, Brazil.
Alessandra Grassi Salles
Rua Joaquim Floriano, 466 - cj. 2102 - Itaim Bibi
São Paulo, SP, Brazil - CEP 04534-002
E-mail: agsalles@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Article received: July 30, 2011
Article accepted: December 3rd, 2011
Study conducted at the Plastic Surgery and Burns Division of the Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (Clinical Hospital of the Medicine College of São Paulo University), São Paulo, SP, Brazil.
Study presented in the 48th Brazilian Congress of Plastic Surgery held in Goiânia, GO, Brazil, during November 11-15, 2011.
Paper awarded Jussara Personelle 2011 prize.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter