INTRODUCTION
Cleft lip and palate is the most common congenital craniofacial malformation, with
an estimated prevalence of 1 case in every 700 live births. Feeding difficulties,
speech changes, and hearing disorders are common in these patients, making appropriate
multidisciplinary treatment generally involving plastic surgery, otorhinolaryngology,
speech therapy, physiotherapy, orthodontics, nursing, and psychology. The need for
different specialties makes it difficult to create and maintain specialized services
in this condition1,2.
The diversity of classifications and the large number of surgical techniques used
in primary surgeries (cheiloplasty and palatoplasty) make it difficult to compare
epidemiological data between specialized services and assess the incidence of complications
associated with these surgeries.
Although many studies have evaluated the incidence of complications in patients undergoing
cheiloplasty and palatoplasty, there is little work carried out in specialized centers
with shorter creation times3-9.
OBJECTIVE
The objective of this work was to evaluate the epidemiological profile and the incidence
of complications in patients with cleft lip and palate undergoing surgical correction
at the Hospital de Clínicas of the Universidade Federal de Uberlândia (HC-UFU), in
Uberlândia-MG, during the initial years of structuring the treatment service for patients
with cleft lip and palate (composed of a plastic and craniomaxillofacial surgeon,
otorhinolaryngology team, speech therapist, dentist and residents in craniomaxillofacial
surgery and otorhinolaryngology).
MATERIALS AND METHODS
A prospective cohort study was carried out with patients diagnosed with cleft lip
and palate who underwent primary surgical procedures, by the same surgeon, accompanied
by residents in cranio-maxillofacial surgery, at HC-UFU, from July 2017 to February
2017. 2023.
Patients under 18 years of age who underwent primary surgical procedures (cheiloplasty
and/or palatoplasty) and who had postoperative follow-up of at least 3 months during
the analyzed period were included.
Patients aged 18 years or older and undergoing other surgical procedures were excluded
from the study.
The following data was collected: date of birth, date of surgery, classification of
the type of cleft lip and palate (using Veau’s classification), type(s) of surgery(s)
performed, and complications associated with the procedures. Parents or guardians
signed an informed consent form before surgery, agreeing with the surgical procedures
and authorizing the use of data. This study was approved by the institution’s Research
Ethics Committee, under number 57032022.5.0000.5152.
Exclusively descriptive statistics were used for epidemiological characterization
and determination of the incidence of complications.
RESULTS
During the period analyzed, 79 patients diagnosed with cleft lip and palate were monitored
and underwent 115 primary surgeries (54 cheiloplasties and 61 palatoplasties).
Among the patients followed, 15 patients (18.98%) had Veau classification type I,
12 patients (15.18%) had type II, 31 patients (39.24%) had type III, and 21 patients
(26.58%) type IV (Table 1).
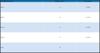
Table 1 - Epidemiological data on patients with cleft lip and palate.
| Classification (Veau) |
Number of cases |
Percentage |
| Type 1 |
15 |
18.98% |
| Type 2 |
12 |
15.18% |
| Type 3 |
31 |
39.24% |
| Type 4 |
21 |
26.58% |
| Total |
79 |
|
Table 1 - Epidemiological data on patients with cleft lip and palate.
The techniques used in cheiloplasty were Fisher in 35 cases (64.81%), Mulliken (bilateral)
in 2 cases (3.70%), and lip adhesion in 15 cases (27.78%) (Table 2).
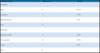
Table 2 - Types of surgeries performed.
| Techniques surgical |
Number of cases |
Percentage |
| Cheiloplasty |
|
|
| Fisher |
35 |
64.81% |
| Lip adhesion |
17 |
27.78% |
| Mulliken (bilateral) |
2 |
3.70% |
| Total |
54 |
|
| Palatoplasty |
|
|
| Bardach (two flaps) |
38 |
62.29% |
| Von Langenbeck |
20 |
32.78% |
| Furlow |
3 |
4.92% |
| Total |
61 |
|
Table 2 - Types of surgeries performed.
The techniques used in palatoplasty were: Bardach (two flaps) in 38 patients (62.29%),
Von Langenbeck in 20 patients (32.78%), and Furlow in 3 patients (4.92%). In 5 patients
(8.19%) the vomer flap was associated (Table 2).
Eleven complications were reported in this period: 2 dehiscences in cheiloplasty (3.70%),
1 hypertrophic scar in cheiloplasty (1.85%), 6 fistula in palatoplasty (9.83%), and
2 dehiscences in palatoplasty (3.28% ) (Table 3).
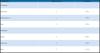
Table 3 - Incidences of complications.
| Complications |
Number of cases |
Percentage |
| Cheiloplasty |
|
|
| Dehiscence |
2 |
3.70% |
| Hypertrophic scar |
1 |
1.85% |
| Total |
3 |
5.55% |
| Palatoplasty |
|
|
| Fistula |
6 |
9.83% |
| Dehiscence |
2 |
3.28% |
| Total |
8 |
13.11% |
Table 3 - Incidences of complications.
The incidence of complications was 9.56% when analyzing the total number of surgeries,
5.55% in patients undergoing cheiloplasty, and 13.11% in patients undergoing palatoplasty.
DISCUSSION
This work evaluated the epidemiological profile and the incidence of complications
in patients with CLP undergoing primary surgery in the initial years of structuring
the cleft lip and palate service at HC-UFU.
The comparison of the incidence of total complications is limited in the literature
because studies consider different occurrences as complications (some studies consider,
for example, the presence of fever in the postoperative period as a complication).
Despite the difference in criteria, our incidence of 9.56% is lower than the work
carried out by Gatti et al.10, which presented an incidence of 14.16%.
Regarding cheiloplasty, recent studies show the presence of complications ranging
between 4.4% and 40%, while we present 5.55%3,6,7,11. The presence of dehiscence in cheiloplasty varies between 3.2% and 15.4% of patients,
while we observed it in 3.70%3,11. Hypertrophic scarring in 14.9%, while in our patients it was 1.85%11.
In palatoplasty, the total incidence of complications varies greatly in recent literature
(15.8% to 70%); our incidence was 13.11%5-7. Fistula development occurs in 2.4% to 28% of patients and, in our service, the incidence
was 9.83%4,5,11-17. The presence of dehiscence in palatoplasty varies between 0.7% and 4%, while we
present 3.28%5,12,18.
Recent studies show that surgical volume (above 25 surgeries/year) as well as the
surgeon’s experience influence the reduction of complications in patients with cleft
lip and palate18,19.
Our work has important limitations (number of patients due to the recent structuring
of the service, only one surgeon with experience in cleft lip and palate, difficulty
in comparing with other studies due to the variation in diagnostic criteria and complications,
and variability of surgical techniques used in each service) and, despite these limitations,
the incidence of complications was similar to studies in already consolidated centers.
CONCLUSION
Our study showed an incidence of complications similar to that of other established
centers and long-term follow-up is necessary to assess the possibility of reducing
complications with increased surgical volume and greater experience.
REFERENCES
1. Hlongwa P, Levin J, Rispel LC. Epidemiology and clinical profile of individuals with
cleft lip and palate utilising specialised academic treatment centres in South Africa.
PLoS One. 2019;14(5):e0215931.
2. Baigorri M, Crowley CJ, Sommer CL, Moya-Galé G. Barriers and Resources to Cleft Lip
and Palate Speech Services Globally: A Descriptive Study. J Craniofac Surg. 2021;32(8):2802-7.
3. Schönmeyr B, Wendby L, Campbell A. Early Surgical Complications After Primary Cleft
Lip Repair: A Report of 3108 Consecutive Cases. Cleft Palate Craniofac J. 2015;52(6):706-10.
4. Deshpande GS, Campbell A, Jagtap R, Restrepo C, Dobie H, Keenan HT, Sarma H, et al.
Early complications after cleft palate repair: a multivariate statistical analysis
of 709 patients. J Craniofac Surg. 2014;25(5):1614-8.
5. Schönmeyr B, Wendby L, Campbell A. Surgical Complications in 1408 Primary Cleft Palate
Repairs Operated at a Single Center in Guwahati, Assam, India. Cleft Palate Craniofac
J. 2016;53(3):278-82.
6. Park E, Deshpande G, Schonmeyr B, Restrepo C, Campbell A. Improved Early Cleft Lip
and Palate Complications at a Surgery Specialty Center in the Developing World. Cleft
Palate Craniofac J. 2018;55(8):1145-52.
7. Ruslin M, Dom L, Tajrin A, Hajrah Yusuf AS, Arif SK, Tanra AH, et al. Establishing
cleft services in developing countries: Complications of cleft lip and palate surgery
in rural areas of Indonesia. Arch Plast Surg. 2019;46(6):511-7.
8. Li F, Wang HT, Chen YY, Wu WL, Liu JY, Hao JS, et al. Cleft relapse and oronasal fistula
after Furlow palatoplasty in infants with cleft palate: incidence and risk factors.
Int J Oral Maxillofac Surg. 2017;46(3):275-80.
9. Schoenbrunner AR, Dalle Ore CL, Lance S, McIntyre J, Jones M, Gosman A. Effect of
Surgeon Volume and Craniofacial Fellowship Training on Cleft Palate Complication Rates.
Ann Plast Surg. 2017;78(5 Suppl 4):S229-32.
10. Gatti GL, Freda N, Giacomina A, Montemagni M, Sisti A. Cleft Lip and Palate Repair.
J Craniofac Surg. 2017;28(8):1918-24.
11. Navarro CE. CIRPLAST: Cleft Lip and Palate Missions in Peru. J Craniofac Surg. 2015;26(4):1109-11.
12. Abulezz TA. Cleft Lip and Palate: An Experience of a Developing Center in Egypt. J
Craniofac Surg. 2017;28(8):e731-e4.
13. Lin KY, Black JS, Wang JS, Kerpelman J, Ho TV, Borowitz K. An outcome study of a 2-flap
pushback palatoplasty used in the treatment of wide cleft palates. J Craniofac Surg.
2015;26(3):620-4.
14. Salimi N, Aleksejuuniene J, Yen E, Loo A. Time Trends and Determinants of Fistula
in Cleft Patients at BC Children’s Hospital, Canada: A Retrospective 18-Year Medical
Chart Audit. Cleft Palate Craniofac J. 2018;55(7):1013-9.
15. Smyth AG, Wu J. Cleft Palate Outcomes and Prognostic Impact of Palatal Fistula on
Subsequent Velopharyngeal Function-A Retrospective Cohort Study. Cleft Palate Craniofac
J. 2019;56(8):1008-12.
16. Tse RW, Siebold B. Cleft Palate Repair: Description of an Approach, Its Evolution,
and Analysis of Postoperative Fistulas. Plast Reconstr Surg. 2018;141(5):1201-14.
17. Rodrigues HLR. Incidência de fistula após palatoplastia à Von Langenbeck com veloplastia
intravelar estendida. Rev Bras Cir Plást. 2015;30(4):597-602.
18. Menegazzo MR, Montoya CG, Gobetti L, Cano AC, Evensen AO, Saldanha O. Palatoplastia
primária pela técnica de Von Langenbeck: experiência e resultados morfológicos obtidos
em 278 casos operados. Rev Bras Cir Plást. 2020;35(1):16-22.
19. Swanson MA, Auslander A, Morales T, Jedrzejewski B, Magee WP 3rd, Siu A, et al. Predictors
of Complication Following Cleft Lip and Palate Surgery in a Low-Resource Setting:
A Prospective Outcomes Study in Nicaragua. Cleft Palate Craniofac J. 2022;59(12):1452-60.
DOI: 10.1177/10556656211046810
1. Hospital das Clínicas da Universidade Federal de Uberlândia, Uberlândia, MG, Brazil
Corresponding author: José Mauro de Oliveira Squarisi Rua Francisco Sales, 86, Osvaldo Resende, Uberlândia, MG, Brazil., Zip code: 38400-440,
E-mail: josemauroeu@yahoo.com.br
Article received: September 14, 2023.
Article accepted: February 4, 2024.
Conflicts of interest: none.