

Case Reports - Year 2011 - Volume 26 -
Fingertip replantation and revascularization: literature review and a case report of fingertip amputation of the fifth finger of a one-year-old child
Reimplante e revascularização da ponta do dedo: revisão de literatura e relato de caso de amputação da ponta do dedo mínimo na criança de um ano de idade
ABSTRACT
The distal phalanx has important functions and must be replanted in case of accidental amputation. Microsurgery is the preferred technique; however, the necessary vein anastomosis can be very difficult or even impossible, especially in small children. This paper reports a case of microsurgical replantation of the distal phalanx of the fifth finger of a one-year-old male child who suffered a crush-type amputation of the fifth fingertip in a house door. The fingertip was replanted eight hours after the amputation, with anastomosis of a very thin artery and vein. The region exhibited congestion, which persisted for more than one week without necrosis; no other procedure was required after the replantation. This paper presents a literature review of the difficulty of restoring venous return in children. Several techniques for restoring venous return in difficult cases, as well as determinants of survival of the amputated part, are reviewed and presented; however, there are no specific studies on procedures for the age group in question. Children probably have better functional recovery or adaptation than do adults, but the amputated part has the same chance of survival, and some of the techniques used in adults are not applicable in children. The literature on this topic is scant, and a study on the most practical and efficient method for fingertip replantation in small children is warranted.
Keywords: Finger phalanges. Replantation. Child.
RESUMO
A falange distal é funcionalmente importante e deve ser reimplantada em casos de acidente. A técnica de eleição é microcirúrgica, porém a anastomose da veia pode ser extremamente difícil ou impossível, principalmente em crianças pequenas. Este artigo reporta um caso de reimplante microcirúrgico da falange distal do dedo mínimo em uma criança de sexo masculino, de um ano de idade, que sofreu amputação da falange distal do dedo mínimo tipo "guilhotina", na porta residencial. A falange foi reimplantada 8 horas após a amputação, com anastomose de uma artéria e uma veia extremamente finas. A região apresentou congestão, que durou mais de uma semana, porém sem necrose, não necessitando condutas coadjuvantes. Neste artigo, que também faz revisão bibliográfica da conduta no retorno venoso difícil em crianças dessa faixa etária, várias técnicas foram revistas e apresentadas na solução de retorno venoso difícil, assim como os fatores que influenciam a sobrevivência da parte amputada, porém não há um estudo específico de conduta para essa faixa etária. A criança, provavelmente, tem melhor recuperação ou readaptação funcional, porém a parte amputada tem as mesmas chances de sobrevivência no reimplante, e algumas técnicas possivelmente não sejam aplicáveis. A literatura é escassa, sendo necessária a realização de um estudo para determinar uma conduta prática e eficiente especificamente para essa faixa etária.
Palavras-chave: Falanges dos dedos da mão. Reimplante. Criança.
The replantation of an amputated fingertip by microsurgical technique is accepted as the most functionally and aesthetically effective approach as well as that with the greatest success rate. Difficulties in establishing venous return are responsible for most of the replantation failures and constitute a challenge for the microsurgeon due to the small caliber or absence of veins, especially in crush amputations.
Several microsurgical and non-microsurgical techniques have been developed and applied successfully; however, there are few useful literature reports on techniques applicable to one-year-old patients.
This study presents a case of finger replantation after a crush-type zone I amputation in a one-year old-child, in which the very small vessel caliber caused great technical difficulty. The relevant literature is reviewed and discussed.
CASE REPORT
YLO, male, one year old, suffered incomplete amputation of the right fifth fingertip due to crushing in a house door. The child was assessed at the emergency service of a pediatric hospital, where surgical amputation and repair of the stump was recommended.
The patient's family contacted the authors to explore the possibility of replantation or revascularization. At the initial examination, the fingertip was ischemic and almost totally amputated; the deep flexor tendon was the sole structure connected to the proximal finger. As the tendon lacks circulatory function, the lesion was considered and treated as a complete amputation.
Radiography indicated a fracture in the distal extremity of the middle phalanx, adjacent to the distal interphalangeal joint. The amputation could be classified as in zone III of the Yamano scheme, according to the vascular pattern, or as immediately proximal to zone II in the Tamai classification.
Replantation was indicated as the injury was a simple finger amputation in zone I (anatomical classification based on the tendon) and in a pediatric patient. The family was informed of the surgical risks and the possibility of failure, and the procedure was initiated. An initial exploration by magnification with a surgical microscope (Vasconcelos), with ischemia maintained by a pneumatic tourniquet on the arm, was conducted under general anesthesia 8 hours after the accident. The amputated part was maintained under "hot" ischemia during this time. A single artery amenable to anastomosis, approximately 0.6 mm in diameter, was found, along with a partially intact ulnar collateral nerve. The bone was fastened with two needles, one longitudinal and the other crossed, as there was no Kirchner wire of sufficiently small caliber available at the time of surgery. Anastomosis of the artery was performed with 4 simple sutures with 10-0 wire (there was no 11-0 or 12-0 wire available) and a 75-micron-caliber needle, and the ischemia was relieved in order to search for the vein. However, identification of the vein was not possible due to the abundant and diffuse bleeding of the rearterialized fingertip. Under ischemia, a single vein 0.3 mm in diameter was found lateral to the nailbed and anastomosed with 3 simple sutures. The extensor tendon was macerated, and its manipulation was therefore avoided to minimize iatrogenic trauma to the vascular anastomosis. The skin was closed by a few simple sutures of 6-0 nylon to allow for drainage, and a loose occlusive dressing was applied.
The surgery lasted 4 hours, and no anticoagulant regimen or systemic antiplatelet treatment was used in the postoperative period.
During the first postoperative day, there was a small amount of blood visible on the dressing, and the fingertip was largely congested with, however, a small area of pink color in the digital pulp. Over the following days, the congestion progressively decreased and, at the end of 7 days, the finger exhibited no area of necrosis.
The bone fixation needles were removed after two weeks of progress in order to avoid infection. Due to lack of repair of the extensor tendon, the patient exhibited "hammer finger;" however, the joint was freely movable. The patient was sent for physiotherapy, with future plans for secondary surgery (Figure 1).
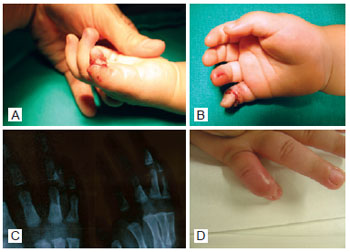
Figure 1 - In A and B, subtotal amputation with continuity maintained only by the deep flexor tendon of the finger. In C, radiography with diagnosis of distal juxta-articular bone amputation of the mid phalanx. In D, replanted finger 3 weeks after surgery, with "hammer finger."
DISCUSSION
Restoration of an amputated body part is defined as replantation when the amputation was complete and revascularization when the amputation was incomplete with some structures remaining and contributing to circulation. In the case presented, the deep flexor tendon and the partially severed collateral nerve made insignificant or null contributions to the circulation of the amputated finger, so the lesion was considered and treated as a complete amputation, i.e., arterial and venous anastomosis was performed.
The indications for replantation are based not only on the potential survival of the amputated part but also, and more importantly, on its potential for functional recovery1. While the loss of the fingertip may seem irrelevant, it is surprisingly disabling, as the fingertip is a highly specialized tissue containing nerve cell endings and the nail.
When the amputated part is not available or is inadequate for replantation, several methods can be used to close the wound, such as healing by secondary intention, primary synthesis, cutaneous grafting, and flap closures. However, these procedures may result in persistent pain, intolerance to cold, paresthesia, hypoesthesia, hyperesthesia, atrophic alterations, shortening of the finger, and nail deformities, among others2. The replantation of the amputated part with microsurgical vascular anastomosis is the technique of choice for fingertip amputations and is routinely performed. However, the success rate remains low due both to the small caliber of the more distal vessels and because there is frequently no vessel suitable for anastomosis.
In more proximal amputations, the greatest problem is the musculotendinous and articular function, while vascular function is the critical factor in distal amputations.
The classification of the amputation level of the upper limb is made from a combination of the flexor tendon zones, described by Verdan and Michon in 1961 and by Kleiner, Kutz, and Atasoy in 19733, and the vascular anatomy of the hand. The distal finger is divided into zones based on the vascular pattern. In the classification of Tamai4, zone I covers the digital pulp up to the nail base and zone II from the nail base to the distal interphalangeal joint. Yamano5 added zone III, which extends from the distal interphalangeal joint to the metacarpophalangeal joint. The most detailed classification is that of Ishigawa et al.6, who subdivide Tamai zone I into subzones I and II and Tamai zone II into subzones III and IV (Figure 2).
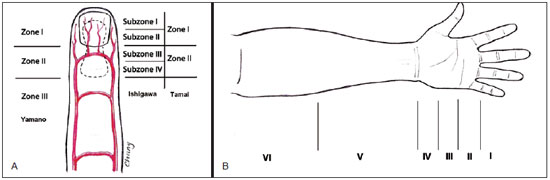
Figure 2 - In A, scheme of the replantation zones of the finger according to the vascular pattern-based classifications of Yamano, Ishigawa, and Tamai. In B, classification based on the flexor tendons. I = distal to proximal interphalangeal joint; II = between the A1 pulley and the insertion of the flexor digitorum superficialis in the middle phalanx; III = palm of the hand; IV = carpal tunnel; V = tendinious portion of the flexor muscles; VI = muscular portion of the flexor muscles.
Insufficient or absent venous drainage is responsible for most fingertip replantation failures. Several techniques have been developed to address the frequent situations in which there is no vein suitable for anastomosis, such as in crush-type or very distal lesions. The synthesis of the amputated part with a compound graft is successful only for small children with a level of amputation distal to the lunula; the results in adults are disastrous. The sutured, deepithelized, and "buried" compound graft in a subcutaneous "pocket" has been successful to a certain extent; however, most hand surgeons do not have confidence in this technique. Kim et al.2 described a technique of arterial microanastomosis with venous drainage supplied by suturing the deepithelized extremity into the deep abdominal fascia, which has considerably greater vascularization than does the subcutaneous tissue, and reported a high rate of success. Akyürek et al.7 reported distal replantations at zone I by arterial anastomosis alone, with venous drainage by bleeding through an incision in the shape of a "fish mouth" for 7 days or by leech application for 10 to 12 days, with 76% success. Many authors consider leeches to be the best non-surgical treatment for venous insufficiency; however, this technique is not commonly used in Brazil. The medicinal leech, Hirudo medicinalis, secretes an anticoagulant called hirudin, which has potent local action with minimal systemic effect and effectively relieves congestion. In general, this therapy is performed for 2 to 3 days; however, prolonged use may cause significant blood loss, which is the major complication of this technique. Another potential complication is infection caused by Aeromonas hydrophila, which may occur in 7% to 20% of cases1,8. A subdermal "pocket" based on the subdermal plexus was described by Lin et al.9 for amputations distal to zone I and is performed in conjunction with arterial anastomosis when possible or with a compound graft when the artery cannot be found. These authors reported only one case of failure in their series; the failed case had been a trauma due to crushing, which significantly worsens the prognosis9. However, Hattori et al.10 achieved considerably superior results when a venous anastomosis was performed and advocate that at least one anastomosis or vein graft should be attempted whenever possible, in spite of the prolonged surgical time.
The technique of late venous drainage was described by Koshima et al.11, who re-explored cases that developed congestion in the days following replantations performed with ultra-microsurgical techniques. A new anastomosis is achieved more easily with veins dilated by congestion. Ito et al.12 carried out a retrospective study aimed at identifying at which levels replanted digits may survive with only arterial anastomosis. These authors found that replantations at Ishigawa subzone I may succeed without venous anastomosis, while those at subzones II and III require some type of procedure for venous drainage by continuous bleeding and venous anastomosis is essential for those at subzone IV12. For zone I amputations, Hsu et al.13 described successful proximal venous and arterial anastomosis in the division of the digital pulp central artery bifurcation, which restored the distal finger venous drainage via the artery. Li et al.14 analyzed 17 factors that determine the survival of the replanted fingertip, including age, gender, dominance, platelet count, finger preservation, ischemia time, tobaccoism, position of the finger, amputation zone, trauma mechanism, type of anesthesia, repair of one or two arteries, creation of none, one, or two venous anastomoses, vein grafting, bone shortening, neurorrhaphy, and tobaccoism after replantation. Gender, age, dominance, position of the finger, level of amputation, and history of tobaccoism did not influence the survival of the replant. Trauma by avulsion or crushing minimizes the chance that the replant will survive, and preservation of the amputated part by inappropriate means also tends to increase the probability of failure. Platelet count greater than 300 × 109 has a strong negative effect on replant survival. The type of anesthesia, number of arterial repairs, presence of bone shortening, and number of venous anastomoses do not influence replant survival, while arterial and venous grafts do increase replant survival. Smoking after the replantation leads to replantation failure14.
CONCLUSIONS
Although vascular calibers are considerably smaller in small children, this fact does not preclude arterial and venous microvascular anastomosis, and the prolonged surgical time is justified. Children have greater capacities for adaptation and functional recovery but apparently similar prognoses for replant survival. The most important determinant of the success of replantation seems to the type of trauma. One of the safer and more practical techniques for establishing venous return in difficult cases must be adapted for this age group.
REFERENCES
1. Pederson WC. Replantation. Plast Reconstr Surg. 2001;107(3):823-41.
2. Kim KS, Eo SR, Kim DY, Lee SY, Cho BH. A new strategy of fingertip reattachment: sequential use of microsurgical technique and pocketing of composite graft. Plast Reconstr Surg. 2001;107(1):73-9.
3. Gallico III GG. Replantation and revascularization. In: McCarthy JG, ed. Plastic surgery: the hand. Philadelphia: WB Saunders; 1990. p. 4355-83.
4. Tamai S. Twenty years' experience of limb replantation: review of 293 upper extremity replants. J Hand Surg Am. 1982;7(6):549-56.
5. Yamano Y. Replantation of the amputated distal part of the fingers. J Hand Surg Am. 1985;10(2):211-8.
6. Ishigawa K, Ogawa Y, Soeda H. A new classification at or distal to the nail for the distal part of the finger. J Jpn Soc Reconstr Microsurg. 1990;3:54-62.
7. Akyürek M, Safak T, Keçik A. Fingertip replantation at or distal to the nail base: use of the technique of artery-only anastomosis. Ann Plast Surg. 2001;46(6):605-12.
8. Weinfeld AB, Yuksel E, Boutros S, Gura DH, Akyurek M, Friedman JD. Clinical and scientific considerations in leech therapy for the management of acute venous congestion: an updated review. Ann Plast Surg. 2000;45(2):207-12.
9. Lin TS, Jeng SF, Chiang YC. Fingertip replantation using the subdermal pocket procedure. Plast Reconstr Surg. 2004;113(1):247-53.
10. Hattori Y, Doi K, Ikeda K, Abe Y, Dhawan V. Significance of venous anastomosis in fingertip replantation. Plast Reconstr Surg. 2003;111(3):1151-8.
11. Koshima I, Yamashita S, Sugiyama N, Ushio S, Tsutsui T, Nanba Y. Successful delayed venous drainage in 16 consecutive distal phalangeal replantations. Plast Reconstr Surg. 2005;115(1):149-54.
12. Ito H, Sasaki K, Morioka K, Nozaki M. Fingertip amputation salvage on arterial anastomosis alone: an investigation of its limitation. Ann Plast Surg. 2010;65(3):302-5.
13. Hsu CC, Lin YT, Moran SL, Lin CH, Wei FC, Lin CH. Arterial and venous revascularization with bifurcation of a single central artery: a reliable strategy for Tamai Zone I replantation. Plast Reconstr Surg. 2010;126(6):2043-51.
14. Li J, Guo Z, Zhu Q, Lei W, Han Y, Li M, et al. Fingertip replantation: determinants of survival. Plast Reconstr Surg. 2008;122(3):833-9.
1. Full member of the Brazilian Society of Plastic Surgery (SBCP), member of the Brazilian Society of Reconstructive Microsurgery, surgeon in the Reconstructive Microsurgery Service of Hospital Federal dos Servidores of the State of Rio de Janeiro, and head of the Medical Residency and coordinator of the Microsurgery Service and of the Center of Studies and Research of the Plastic Surgery Service of Hospital Federal Andaraí of Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
2. Full member of the SBCP, full member and former president of the Brazilian Society of Reconstructive Microsurgery, and head of the Reconstructive Microsurgery Service of Hospital Federal dos Servidores of the State of Rio de Janeiro, Rio de Janeiro, RJ, Brazil.
Correspondence to:
Chang Yung Chia
Av. Lúcio Costa, 3.360 - bloco 8 - ap. 2.402 - Barra da Tijuca
Rio de Janeiro, RJ, Brazil - CEP 22630-010
E-mail: changplastica@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: February 28, 2011
Paper accepted: October 31, 2011
Study conducted at author's private clinic, Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter