

Case Reports - Year 2011 - Volume 26 -
Fasciocutaneous flap of the inner thigh for scrotal reconstruction in Fournier syndrome
Retalho fasciocutâneo de região interna de coxa para reconstrução escrotal na síndrome de Fournier
ABSTRACT
Fournier syndrome is a severe disease that should be treated aggressively with debridement and broad-spectrum antibiotics. It usually causes loss of a large area of tissue and may spread to other areas beyond the perineum such as the abdomen, lower limbs, dorsum, chest, and retroperitoneum. The loss of the scrotum is a common condition in this pathology. Two cases of scrotum reconstruction with the fasciocutaneous flap of the inner thighs with excellent recovery, good aesthetic results, and few complications are reported.
Keywords: Scrotum. Surgical flaps. Fournier gangrene.
RESUMO
A síndrome de Fournier é uma doença grave e que deve ser agressivamente tratada com desbridamentos e antibioticoterapia de amplo espectro. Geralmente causa perda de grande área de tecido, podendo espalhar-se para outras áreas além do períneo, como abdome, membros inferiores, dorso, tórax e retroperitônio. A perda da bolsa escrotal é uma situação frequente nessa doença. São relatados dois casos de reconstrução de bolsa escrotal com retalho fasciocutâneo de região interna de coxas, com excelente recuperação, bom resultado estético e poucas complicações.
Palavras-chave: Escroto. Retalhos cirúrgicos. Gangrena de Fournier.
Fournier syndrome, which is characterized by severe fasciitis of the perineal and genital regions and is caused by various bacterial species, may spread to all regions of the body. This infection causes rapid tissue necrosis and severe toxemia; this condition may lead to death if it is not treated early and aggressively.
In general, the infection occurs in immunosuppressed patients such as diabetic, HIV-positive, alcoholic, and elderly individuals; patients with low socioeconomic levels; and undernourished individuals1,2. The initial focus of the disease is generally due to trauma or infection in the perianal region or urinary tract1.
Often after eliminating the infection and removing the devitalized tissues, extensive open areas, mainly in the pubis, perineum, and genital region, must be covered.
The scrotal region requires high-quality coverage as it is an important gland that produces sperm and is the representative organ of masculinity. In general, the necrosis is restricted to the scrotum and does not reach the testicles or spermatic funiculus1.
CASE REPORTS
Case 1
Patient JGS, 53 years old, had untreated diabetes. He presented with a perianal abscess and was prescribed oral antibiotics. The abscess was also punctured with a needle. He developed edema, blistering, and intense pain in the scrotum, associated with fever and prodromal signs.
Extensive debridement was performed, and broad-spectrum antibiotics were administered (i.e., cephalothin, gentamicin, and metronidazole). After 12 days of treatment, the patient presented with an extensive infected wound, exposing the testicles and spermatic funiculi. The wound was dressed with 1% silver sulfadiazine, and the diabetes was clinically controlled. After 5 days, a double fasciocutaneous flap of the bilateral inner thighs was prepared, and the scrotal defect was closed (Figure 1). The patient was discharged 2 days after the surgery.
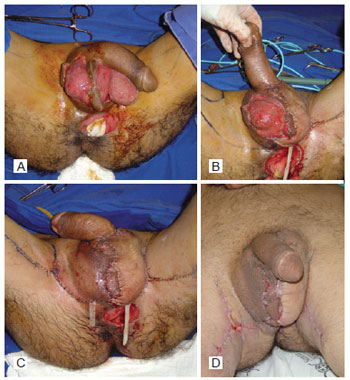
Figure 1 - A, preoperative image of scrotum necrosis due to Fournier fasciitis. B, first flap prepared for coverage of the left testicle. C, immediate postoperative appearance. D, postoperative appearance at 15 days.
Case 2
Patient ABR, 70 years old, was diabetic for 10 years without appropriate treatment. He developed a perianal abscess that evolved with perineal gangrene, quickly expanding to the abdomen and flanks.
Upon admission, he presented with severe sepsis requiring endotracheal intubation. He was treated with debridement and broad-spectrum antibiotics (i.e., oxacillin, metronidazole, and gentamicin) in addition to diabetes control, intensive care, and local dressing with 1% silver sulfadiazine. The patient was discharged from the Intensive Care Unit after 7 days. On the 25th day of hospitalization, he was operated on with the production of a double fasciocutaneous flap of the inner thighs for testicle and pubis coverage, suturing of the abdomen fascia, skin graft in the penis, and approximation of the abdominal flap for closure of the defect (Figure 2). On the 4th postoperative day, the patient was discharged for outpatient follow-up; dehiscence developed in only certain regions of the flap, which were quickly closed with conservative treatment.
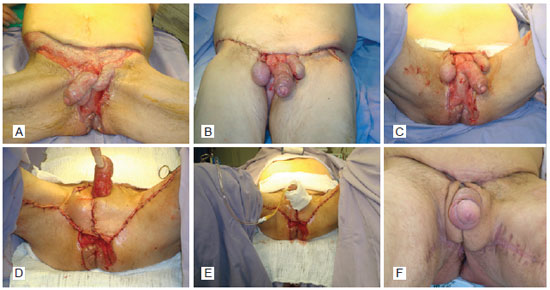
Figure 2 - A, preoperative image of the abdomen, pubis, and scrotum lesion. B, patient right after the abdominal fascia and skin suture, and fat tissue after short detachment. C, open area of the pubis and scrotum ready to be closed with the double fasciocutaneous flap from the inner thighs. D, immediate postoperative period after preparation of the thigh fasciocutaneous flap. E, appearance after partial skin graft in the penis. F, 2-month postoperative appearance.
At the time of discharge, both patients had a perianal fistula and were referred for outpatient follow-up and treatment.
DISCUSSION
Fournier syndrome can be prevented by controlling the underlying diseases of the patient and by early treatment of infections and traumas of the perineum and genitourinary system1,2.
The treatment involves the removal of devitalized tissues in regions where antibiotics do not penetrate. Broad-spectrum antibiotics should be used because several bacterial species are responsible for the disease; the bacteria species in descending order of incidence are: Escherichia coli, Pseudomonas pyocyaneus, Staphylococcus spp., Streptococcus spp., Bacteroides spp., Proteus spp., Clostridium spp., and Klebsiella pneumoniae among others1. Ensuring intensive care while maintaining vital signals and tissue oxygenation, providing mechanical ventilation if necessary, is essential for patients with sepsis.
The resulting wound should be dressed after the infection is treated. Depending on the lesion in the scrotum and surrounding tissues, one of the following reconstruction strategies can be chosen: orchiectomy with spontaneous closure, skin graft, simple burial of the testicles, skin flaps, or fasciocutaneous or musculocutaneous flaps1-3. The fasciocutaneous flap of the inner thighs provides excellent closure for extensive losses of scrotal skin, perineum, and pubis because it is easy to rotate, rarely presents necrosis, and provides excellent aesthetic results3.
The fasciocutaneous flap of the inner thighs has excellent vascularization because of the presence of the branches of the femoral artery (internal and circumflex pudendal), making the flap very safe even in diabetic and vasculopathic patients3.
Loss of fertility is a complication of this technique. Impaired spermatogenesis is a result of the difficulty in maintaining a lower temperature in the testicles (35°C). However, this problem is also seen with other techniques, since none of them allow retraction and relaxation of the scrotum or mimic the function of the specialized vessels of the region4.
CONCLUSIONS
The use of the fasciocutaneous flap of the inner thighs for scrotal reconstruction is safe and results in very good aesthetic outcomes. For patients that wish to have children, we recommend collection and freezing of sperm for future in vitro fertilization. This procedure should be performed within the first 3 months of scrotum reconstruction.
REFERENCES
1. Bhatnagar AM, Mohite PN, Suthar M. Fournier's gangrene: a review of 110 cases for aetiology, predisposing conditions, microorganisms, and modalities for coverage of necrosed scrotum with bare testes. N Z Med J. 2008;121(1275):46-56.
2. Ferreira PC, Reis JC, Amarante JM, Silva AC, Oliveira IC, da Silva PN. Fournier's gangrene: a review of 43 reconstructive cases. Plast Reconstr Surg. 2007;119(1):175-84.
3. Monteiro E, Carvalho P, Costa P, Ferraro A. "Inner thigh lift flap" for Fournier gangrene of the scrotum. Plast Reconstr Surg. 2002;110(5):1372-3.
4. Wang D, Zheng H, Deng F. Spermatogenesis after scrotal reconstruction. Br J Plast Surg. 2003;56(5):484-8.
Full member of the Brazilian Society of Plastic Surgery (SBCP), plastic surgeon of Santa Casa de Misericórdia de Ponta Grossa, Ponta Grossa, PR, Brazil.
Correspondence to:
Victor Mauro
Rua Carlos Osternack, 111 - 1o andar - Vila Estrela - Ponta Grossa, PR, Brazil - CEP 84010-120
E-mail: vicmauro@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: February 16, 2010
Paper accepted: May 2, 2010
Study conducted at Santa Casa de Misericórdia de Ponta Grossa, Ponta Grossa, PR, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter