

Original Article - Year 2011 - Volume 26 -
Transareolopapilar incision for breast augmentation: 10-year experience at the Ivo Pitanguy Institute
Incisão transareolopapilar para mamoplastia de aumento: experiência dos últimos 10 anos do Instituto Ivo Pitanguy
ABSTRACT
BACKGROUND: There are numerous access routes for inserting implants during breast augmentation surgery. In 1966, Pitanguy described the transareolopapilar route. The aim of this study was to assess the use of transareolopapilar incision during breast augmentation surgery at the Ivo Pitanguy Institute (Rio de Janeiro, RJ, Brazil), over the past 10 years.
METHODS: Retrospective analyses of the size of the implants used, indications for transareolopapilar incision, postoperative complications, and postoperative scarring were performed.
RESULTS: Fifty-three patients with a mean age of 33.54 years were included, and the mean follow-up period was 11.6 months. Most (60.4%) of the implants were <200 ml. Twelve patients required a second operation due to a breast lump (1 case); infection (1 case); capsular contracture (1 case); and dissatisfaction with breast shape (4 cases), volume (4 cases), and unilateral scarring (1 case). Sixteen (30.2%) patients developed some form of minor postoperative complication; 13 (24.5%) had one or more scarring issues, including hypochromia (18.9%), hypertrophy (1.9%), scar retraction (1.9%), and areola bifida (1.9%). Twenty (37.7%) patients underwent postoperative follow-up for more than one year and were satisfied with the postoperative scar.
CONCLUSIONS: The transareolopapilar incision facilitates the insertion of small-to-moderate size implants with a low rate of postoperative complications and a low incidence of scarring, provided the correct surgical technique is used.
Keywords: Mammaplasty. Breast implants. Breast implantation. Silicone gels. Hypopigmentation.
RESUMO
INTRODUÇÃO: Várias vias de acesso foram criadas para a inclusão de implantes na cirurgia de aumento das mamas. Em 1966, Pitanguy descreveu a via de acesso transareolopapilar. O objetivo do presente estudo é avaliar as mamoplastias de aumento realizadas no Instituto Ivo Pitanguy (Rio de Janeiro, RJ, Brasil), nas quais se utilizou a incisão transareolopapilar, nos últimos 10 anos.
MÉTODO: Realizado estudo retrospectivo, analisando-se os seguintes parâmetros: tamanho dos implantes, indicação da incisão transareolopapilar e complicações pós-operatórias, como alterações cicatriciais.
RESULTADOS: Foram incluídas no estudo 53 pacientes, com média de idade de 33,54 anos e tempo médio de seguimento de 11,6 meses. A maioria (60,4%) dos implantes possuía menos de 200 ml. Doze pacientes foram submetidas a reintervenções pelas seguintes razões: nódulo mamário (1 caso), infecção (1 caso), contratura capsular (1 caso), e insatisfação com a forma das mamas (4 casos), com o volume (4 casos) e com a cicatriz unilateral (1 caso). Dezesseis (30,2%) pacientes desenvolveram alguma complicação menor no pós-operatório e 13 (24,5%) apresentaram alguma alteração cicatricial no pós-operatório: hipocromia (18,9%), hipertrofia unilateral (1,9%), retração cicatricial unilateral (1,9%), e aréola bífida (1,9%). Vinte (37,7%) pacientes realizaram seguimento pós-operatório superior a um ano e relataram satisfação com a cicatriz.
CONCLUSÕES: A incisão transareolopapilar permite a inclusão de implantes de tamanho pequeno a moderado, com baixo índice de complicações pós-operatórias e cicatriciais, desde que seguida a correta técnica cirúrgica.
Palavras-chave: Mamoplastia. Implantes de mama. Implante mamário. Géis de silicone. Hipopigmentação.
The breasts are organs of singular importance for a woman's sexuality. They are also associated with female psychosocial wellbeing. Developments in technologies for manufacturing breast implants as well as in surgical techniques have led to the increasing incidence of breast augmentation surgery in Brazil and the world.
Breast augmentation surgery dates back to 1889, when Gersuny performed breast augmentation via paraffin injection1. Since then, the materials for performing this procedure have changed significantly and have included ivory prostheses, dermal-adipose grafts, sponges of different compositions, silicone liquid or gel, and silicone receptacles inflated with different liquids1. In 1962, Cronin and Gerow introduced the first silicone gel implant for breast augmentation, radically modifying this surgical procedure and helping to increase its popularity1.
The development of different access routes for inserting implants was as important as the evolution of breast augmentation surgery. Dufourmentel and subsequently, Webster, Sinder, and Stewart proposed different types of incisions, always approaching the areola and avoiding the upper poles of the breasts2. Other routes, such as the periareolar route associated with horizontal incisions and the submammary and total periareolar routes have also been proposed (Figure 1)2.

Figure 1 - Types of incisions for mammary gland access. (Reproduced from Camargos et al.2)
In 1966, Pitanguy3 described the transareolopapilar approach, advocating it as an excellent access route for gynecomastia correction procedures. The same author advocated the use of a referred incision for breast augmentation procedures, subcutaneous mastectomies, and correction of inverted or hypertrophied nipple4. Subsequently, recent studies advocated the use of this access route, stipulating the advantages of performing an incision in the areolar-papillary complex5-7.
The transareolopapilar approach is not restricted to surgery for gynecomastia correction or breast augmentation and can also be used for procedures such as the removal of benign tumors from the breasts8. The advantage of this approach is the ease of access it provides to all breast quadrants.
However, the referred access route has historically been unpopular for breast augmentation surgery with implants since it is associated with difficult lactation, greater rates of capsular contracture, visible scarring, and alterations in the sensitivity of the areolar-papillary complex9. Other authors have advocated the use of this access route exclusively for patients with an areola diameter of > 3.5 cm and pronounced breast ptosis8.
The present study aimed to retrospectively evaluate breast augmentation surgery with implant insertion performed using the transareolopapilar incision at the Ivo Pitanguy Institute over the past 10 years, assessing the quality of scarring and the incidence of postoperative complications.
METHODS
Patients who underwent breast augmentation surgery performed via the transareolopapilar access route according to the original technique of Pitanguy3 at the Ivo Pitanguy Institute (Rio de Janeiro, RJ, Brazil) over the preceding 10 years were retrospectively analyzed (Figures 2 and 3).
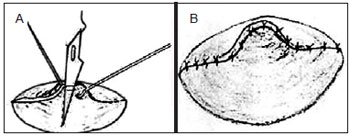
Figure 2 - In A, technique for transareolomammilary incision. In B, result after closure. (Reproduced from Pitanguy et al.10)
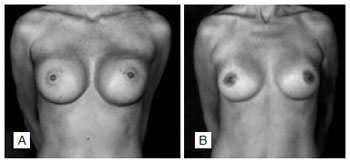
Figure 3 - In A, patient with a polyurethane implant (285 ml) in the second postoperative month. In B, patient with a textured implant (245 ml) in the third postoperative month.
The study consisted of:
analyses of medical records with data collection and; comparative analyses of preoperative and postoperative photographs taken by two plastic surgeons at different time points. The following patients were excluded from the study: patients who received a transareolopapilar incision for procedures other than breast augmentation; patients who developed keloids; patients with incomplete data.
RESULTS
Over the past 10 years, 53 patients had undergone breast augmentation surgery at the Ivo Pitanguy Institute with implants inserted using the transareolopapilar route; 52 patients were white and one was black. Their age ranged from 16-57 years, with an average of 33.54 years. The postoperative follow-up period ranged from 2 months to 9 years, averaging 11.6 months.
Twelve patients required repeat surgery, two of whom underwent more than two repeat surgeries. The major causes of repeat surgery were development of a unilateral breast lump (1.9%); infection (1.9%); unilateral capsular contracture (1.9%); and dissatisfaction with breast shape (7.6%), volume, (7.6%), and scarring (1.9%).
A total of 16 patients (30.2%) developed some form of postoperative complication. However, there was no evidence of severe complications. We identified 8 (15%) cases in which there was a report of slight maceration of the skin at the moment of implantation, 3 (5.7%) of suture extrusion, 2 (3.8%) of seroma, 2 (3.8%) of breast pain, and 1 (5.9%) case of a cyst forming in the scar (Figure 4).

Figure 4 - Postoperative complications.
Regarding the incision indication, we observed 48 (90.5%) cases in which the incision was indicated as part of routine surgery, 2 (3.8%) cases of inverted nipple, 1 (1.9%) of removal of a breast lump from the superomedial quadrant, 1 (1.9%) of hypertrophic nipple, and 1 (1.9%) case of a preexisting incision (Figure 5).
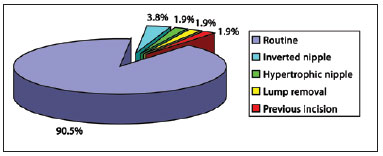
Figure 5 - Incision indications among the studied cases.
With regard to scarring complications, late scarring complications were observed in 13 (24.5%) cases. We considered late scarring complications those identified from the sixth postoperative month onward. The following scarring complications were identified (Figure 6):

Figure 6 - Photographic assessment of scarring complications.
scar hypochromia in 10 (18.8%) cases: 6 (11.3%) bilateral and 4 (7.5%) unilateral; unilateral hypertrophic scarring in 1 (1.9%) case; scar retraction in 1 (1.9%) case; papilla bifida in 1 (1.9%) case.
A relationship between the occurrence of some of the postoperative complications previously described and type of scarring complication was only observed in three cases.
The most common implants used in this study were SILIMED® (46; 86.7%), McGhan® (4; 7.6%), Mentor® (2; 3.8%), and Perthese® (1; 1.9%). The volume of the implants inserted during surgery was 120 ml in 1.9% of the cases, 120-160 ml in 11.3%, 160-200 ml in 47.2%, 200-240 ml in 28.3%, 240-280 ml in 9.4%, and 285 ml in 1.9% of the cases. The smallest implant inserted was a 120-ml Perthese® implant, and the largest was a 285-ml SILIMED® implant.
The patients reported a high rate of satisfaction with the procedure and with scarring in general. A total of 20 (37.7%) patients were followed-up for more than one year postoperatively and all reported satisfaction with the surgical and scarring results.
One patient became pregnant after surgery and successfully breastfed for 8 months.
DISCUSSION
The transareolopapilar incision was described by Pitanguy in 1966 as an alternative to subcutaneous mastectomy in the treatment of gynecomastia3,10. Breast augmentation surgery using this incision was proposed at a later date4. Other authors have also proposed that this surgical route be used for the performance of other surgical procedures8.
However, relatively few authors have advocated the use of this access route, principally because of: changes in the areolar-papillary complex; difficult lactation; increase in infection indices; visible and hypopigmented scarring; need for another access route in the case of breast ptosis in the future; and greater incidence of capsular contracture9.
In the present study, we only observed minor complications in 30.2% of the cases; these were not related to scarring and indeed are common to the majority of breast augmentation surgeries that include the insertion of implants.
Changes relating to scarring were observed in 24.5% of the studied cases after an average postoperative follow-up of 11.6 months. Despite the high percentage of patients with scarring alterations, we only detected two cases in which the patients underwent unilateral procedures for review of scarring.
The major scarring complication observed was scar hypochromia, which was reported in 18.8% of the cases. Other scarring complications, such as papilla bifida, hypertrophic scarring, and scar retraction, were present in 1.9% of the cases each. The great advantage of a complication such as hypochromia in the areolar-papillary complex region is the possibility of benign evolution after the use of adjuvant treatments such as micropigmentation, which tends to have excellent results with high satisfaction rates.
One patient became pregnant after surgery and successfully breastfed her infant. Although this was an isolated case, it constitutes an event that should be mentioned as it was the only pregnancy identified during the postoperative follow-up period.
An interesting finding was the use of this access route for the treatment of other diseases of the areolar-papillary complex concomitant with the procedure for implant inclusion. This incision was indicated for the correction of inverted or hypertrophic nipple in 7.5% of the patients. This type of connection has already been demonstrated by the senior author in other studies4,7.
We observed 12 cases in which it was necessary to perform a repeat surgery, 2 (3.8%) of which were due to capsular contracture. This is a low rate compared with that reported in the literature (11%)4. Other causes of the need for repeat surgery included scarring review in two patients, and replacement of the implants for other reasons in nine cases.
The implants used ranged from 120-285 ml; it was impossible to insert large volume implants in breasts with small areolar-papillary complexes. Usually, at the Ivo Pitanguy Institute, areolar-papillary complexes of <3.5 cm are selected as candidates for other access routes for breast implant insertion; in these cases, the preferential access route is via the inframammary crease. In this study, the majority of the implants had a volume between 160 ml and 240 ml, pointing to possible difficulties in inserting implants of greater volume using this incision, even if the diameter of the areolar-papillary complex was >3.5 cm.
As the transareolopapilar incision access route is a physiological route with minimal impact on the lacteal ducts, it is a preferable approach compared with the lower periareolar access route. However, the acceptance of this access route by some patients tends to be very low, primarily because the scar is placed at the center of the areolar-papillary complex, dividing the papilla in the middle.
However, the transareolopapilar incision should not be totally disregarded as it enables greater access to the mammary gland, facilitating easier bipartition of the breast, and has an acceptable incidence of scarring complications, most of which are reversible with the use of adjuvant treatments such as micropigmentation. The satisfaction rate with this access route was high, and the requirement of scarring review was very low (1.8%) in the current study.
CONCLUSIONS
Transareolopapilar incision enables the insertion of implants of moderate size (120-285 ml), with a low incidence of postoperative complications and an acceptable rate of scarring complications, most of which are reversible with simple adjuvant treatments.
REFERENCES
1. Pitanguy I, Salgado F, Radwanski HN, Stersa RM. Estágio atual dos implantes mamários. Rev Bras Cir. 1991;81(6):291-9.
2. Camargos AG, Ferreira EM, Ferreira FPM, Lima JCSA. Correção de ginecomastia pela via periareolar circular: uma alternativa para ressecção do excesso de pele. Rev Bras Cir Plast. 2007;22(2):107-15.
3. Pitanguy I. Transareolar incision for gynecomastia. Plast Reconstr Surg. 1966;38(5):414-9.
4. Pitanguy I. Aesthetic plastic surgery of head and body. Berlin: Springer-Verlag; 1981. p.50-63.
5. Kompatscher P, Schuler C, Beer GM. The transareolar incision for breast augmentation revisited. Aesthetic Plast Surg. 2004;28(2):70-4.
6. Terino EO. Essential concepts in prosthetic breast surgery. Aesthetic Plast Surg. 1982;6(1):25-32.
7. Pitanguy I. Mamilo invertido. Rev Bras Cir. 1975;64:199.
8. Cardoso AA, Paulinelli RR, Freitas-Júnior R, Rahal RMS, Jacinto TF. Análise comparativa da técnica da incisão em duplo círculo com as técnicas com incisão periareolar e transareolomamilar de correção cirúrgica da ginecomastia. Rev Bras Ginecol Obstet. 2007;29(9):465-9.
9. Tenius FP, da Silva Freitas R, Closs Ono MC. Transareolar incision with geometric broken line for breast augmentation: a novel approach. Aesthetic Plast Surg. 2008;32(3):546-8.
10. Pitanguy I, Muller P, Davalo P, Barzi A, Persichetti P. Trattamento della ginecomastia attraverso una incisione transareolare. Minerva Chir. 1989;44(17):1941-8.
1. General surgeon, post-graduation student of Plastic Surgery at Ivo Pitanguy Institute, Rio de Janeiro, RJ, Brazil.
2. Full member of the Brazilian Society of Plastic Surgery (SBCP), Associate Professor of the Course of Post-Graduation in Plastic Surgery at Pontifícia Universidade Católica do Rio de Janeiro and at Instituto Carlos Chagas, plastic surgeon of the team of Prof. Ivo Pitanguy - Clínica Ivo Pitanguy, Rio de Janeiro, RJ, Brazil.
3. Patron of the SBCP, Member of the National Academy of Medicine and Brazilian Academy of Letters, Full Professor at the Medical Post-Graduation Course of Plastic Surgery at Pontifícia Universidade Católica do Rio de Janeiro and at Instituto Carlos Chagas, Rio de Janeiro, RJ, Brazil.
Correspondence to:
João Paulo Mendes Verbicário
Rua Fonte da Saudade, 126/703 - Lagoa
Rio de Janeiro, RJ, Brazil- CEP 22471-210
E-mail: jpverbicario@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: February 8, 2011
Paper accepted: October 10, 2011
Study conducted at the Ivo Pitanguy Institute, Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter