

Original Article - Year 2011 - Volume 26 -
Breast reconstruction using latissimus dorsi muscle flap: a novel surgical technique with reduced scarring
Reconstrução de mama usando o músculo grande dorsal: descrição de uma nova técnica com cicatriz reduzida
ABSTRACT
BACKGROUND: The latissimus dorsi muscle flap is one of the most commonly used surgical options for breast reconstruction. The donor area scar on the back, although sometimes hidden beneath the bra strap, is often extensive and enlarged or hypertrophic. The aim of this study is to describe the dissection and rotation of the latissimus dorsi muscle using 2 reduced vertical incisions.
METHODS: Twelve female patients underwent unilateral breast reconstruction with latissimus dorsi muscle flap. Ten patients had Poland's syndrome, and their breast reconstruction was performed with a tissue expander at the first instance, with subsequent latissimus dorsi muscle flap rotation to cover the silicone prosthesis. Two patients experienced volume decrease, irregularities, and breast retractions after adenomastectomy; their prosthesis were also covered by a latissimus dorsi muscle flap. The surgical procedure consisted of a 5-cm longitudinal incision on the lateral border of the latissimus dorsi muscle and another on the inframammary fold. Dissection, section, and rotation of the muscle were performed through skin retraction.
RESULTS: The final extension of the scar at follow-up averaged 6.2 cm. The mean surgical time for flap rotation and synthesis of the donor area was 80 minutes. No postoperative complications were observed in any of the cases.
CONCLUSIONS: The reduced incision for dissection of the latissimus dorsi flap for breast reconstruction proved to be feasible and safe; this method provides aesthetic advantages without increasing cost or surgical time.
Keywords: Breast/surgery. Poland syndrome. Mammaplasty. Plastic surgery/methods.
RESUMO
INTRODUÇÃO: O retalho de músculo grande dorsal (MGD) é uma das opções cirúrgicas mais usadas nas reconstruções mamárias. A cicatriz da área doadora no dorso, embora por vezes situada sob a alça do sutiã, frequentemente é extensa e pode ser de qualidade ruim (alargada ou hipertrófica). O objetivo deste trabalho é descrever a dissecção e rotação do MGD através de duas incisões reduzidas.
MÉTODO: No total, 12 pacientes do sexo feminino foram submetidas a reconstrução mamária unilateral com retalho de MGD isolado (sem pele). Dessas pacientes, 10 eram portadoras de síndrome de Poland e tiveram suas mamas reconstruídas com expansor tecidual num primeiro tempo, com posterior rotação do retalho de MGD para cobrir a prótese de silicone definitiva; e outras 2 pacientes tinham evoluído com diminuição do volume, irregularidades e retrações da mama após adenomastectomia, e tiveram sua prótese coberta pelo MGD. O procedimento cirúrgico consistiu de incisão longitudinal de 5 cm sobre a borda lateral do MGD e no sulco inframamário. Realizou-se dissecção, secção e rotação do músculo somente com a retração da pele.
RESULTADOS: Em seguimento ambulatorial, a extensão da cicatriz apresentou média de 6,2 cm. O tempo cirúrgico médio para rotação do retalho e síntese da área doadora foi de 80 minutos. Não foram observadas complicações pós-operatórias nesta série.
CONCLUSÕES: A incisão reduzida para dissecção do MGD nas reconstruções mamárias mostrou-se bastante factível e segura, com vantagem estética e sem aumento dos custos e do tempo cirúrgico.
Palavras-chave: Mama/cirurgia. Síndrome de Poland. Mamoplastia. Cirurgia plástica/métodos.
The latissimus dorsi muscle flap is one of the most commonly used surgical options for breast reconstruction. The donor area scar on the back, although sometimes hidden beneath the bra strap, is often extensive (15 cm to 25 cm) and enlarged or hypertrophic. Therefore, minimally invasive techniques have been developed and are being used more frequently.
For breast reconstruction, exclusive muscular coverage of the silicone prosthesis may be required. Adenomastectomies, previously handled by direct placement of prosthesis below the pectoralis major muscle and serratus anterior, may have very thin cutaneous coverage, leaving the prosthesis palpable and requiring muscular overlap of the latissimus dorsi. For patients with Poland's syndrome and agenesis of the pectoralis major and pectoralis minor, it is essential to reconstruct the armpit's anterior pillar; this reconstruction can be more suitably achieved through transposition of the latissimus dorsi muscle1. The endoscopic approach, in spite of the device's cost, typically uses 3 incisions: a 1- to 2-cm port incision or an axillary incision (5 cm to 6 cm) and 2 other port incisions.
Therefore, the aim of this study is to describe the dissection and rotation of the latissimus dorsi muscle through 2 reduced incisions and provide measurements of the resulting thoracic scars.
METHODS
Twelve female patients underwent unilateral breast reconstruction with latissimus dorsi muscle flap. Ten of these patients had Poland's syndrome, and their breasts were first reconstructed with tissue expansion and posterior replacement by silicon prosthesis followed by latissimus dorsi muscle flap for coverage. The 2 other patients developed volume decrease, irregularities, and breast retraction after adenomastectomy; surgical reconstruction was required to correct these deformities. These patients received a silicone implant with latissimus dorsi flap surgery.
Surgical Procedure
The surgical procedure began with the patient in the lateral decubitus position. A 5-cm longitudinal incision was performed over the lateral edge of the latissimus dorsi muscle (Figure 1). We dissected, sectioned, and rotated the muscle by retracting the skin with surface retractors and pulling the muscle toward the incision, without endoscopic assistance (Figure 2). In the first 2 cases, another incision with the same extension at the axillary region was used to assist pedicle dissection and flap rotation. The dissection started on a plane between the subcutaneous tissue and the latissimus dorsi, between the rib cage and the latissimus dorsi muscle. After dissection was completed, an inferior and medial incision was performed between the latissimus dorsi and trapezius muscles. Langenbeck retractors were used for assistance during the procedure.

Figure 1 - A 5-cm longitudinal incision over the lateral edge of the latissimus dorsi muscle.
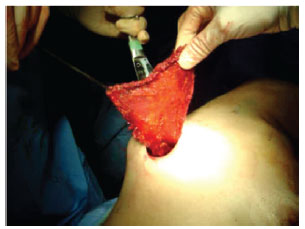
Figure 2 - Dissection, section, and rotation of the muscle by only retracting the skin with surface retractors and pulling the muscle towards the surgical incision.
For breast molding and flap transposition of the latissimus dorsi, a new incision in the receiving area was required. All patients had a previous incision as a result of a previous adenomastectomy or the placement of a skin expander. The flap was rotated towards the thorax, and absorbable sutures were used at the donor site, with the intention of reducing dead space and decreasing the risk of hematomas and seromas. Vacuum closed drainage was used in all cases. After suturing the donor area and placing the patient in a supine position, synthesis was performed in the receiving area.
RESULTS
Twelve surgical procedures were performed using the latissimus dorsi transposition for breast reconstruction. During the follow-up period, no complications such as hematomas, seromas, wound dehiscence, impairment of flap viability, or aesthetic loss of the reconstructed breast were observed.
The average extension of the scar was 6.2 cm during the outpatient follow-up, ranging from 4.4 cm to 7 cm (Figure 3).
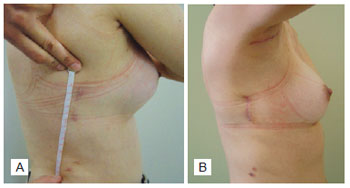
Figure 3 - A patient with Poland's syndrome who underwent breast reconstruction with latissimus dorsi muscle flap with reduced incisions. In A, outpatient measurement of the scar extension. In B, the presence of the axillary scar is observed in the first two cases in this study.
The average time required to perform the entire surgical procedure, including flap rotation and synthesis of the donor and receiving areas, was 80 minutes.
Figures 4 and 5 show 2 patients who underwent breast reconstruction using the latissimus dorsi flap.
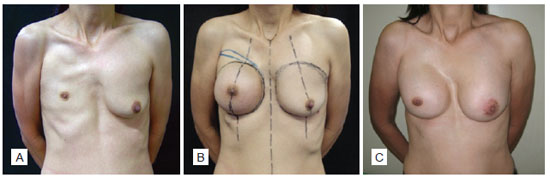
Figure 4 - Patient with Poland's syndrome. In A, preoperative aspect. In B, appearance after placing the expander. In C, appearance after breast reconstruction.
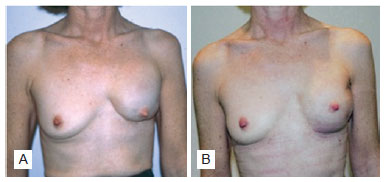
Figure 5 - Patient who underwent breast reconstruction after adenomastectomy, with placement of subpectoral breast prosthesis. In A, pre-transposition aspect of the latissimus dorsi muscle. In B, post-transposition aspect of the latissimus dorsi muscle.
DISCUSSION
The latissimus dorsi flap is a versatile flap that can be employed in a wide range of reconstructions for correcting thoracic deformities. The muscular anatomy is generally predictable, and the muscle has good vascularization and flexibility for transposition to several areas, based on its rotation arch. The flap can be transferred with a skin island, enabling long-lasting thoracic coverage, associated with or without expanders and breast implants for reconstruction2,3. Although the latissimus flap has all of the aforementioned technical advantages, the chance of minor complications is approximately 25%, including hypertrophic scar, contractures, seromas, hematomas, and infections4.
The major indication for the use of a latissimus dorsi flap is breast reconstruction after cancer and congenital defects of the thoracic wall, such as in Poland's syndrome. The latissimus dorsi is also used for reconstructions in the head and neck (after trauma or tumor exeresis), lower limbs, and thorax (other acquired thoracic defects).
With the recent advances in diagnostic modalities, diagnosis of breast cancer occurs earlier; this has led to the development of more conservative and less mutilating therapeutic alternatives5. The latissimus flap was used for the first time in 1906 by Tanzini for coverage of the mastectomy area in a patient with breast cancer. Later, in the 1990s, this use was popularized both after quadrantectomies and in broad resections6. Poland's syndrome has a spectrum of clinical presentations that range from hypomastia to amastia, with absence of the sternal and clavicular portion of the latissimus dorsi in almost all cases7. In minor cases, breast reconstruction may simply require implants; however, in serious cases, it is necessary to associate the prosthesis with a latissimus dorsi flap for suitable coverage of the implant.
Minimally invasive techniques are desirable in all surgery fields. Breast surgery, because of a tumor or malformation, would most benefit from this concept due to its special characteristics of reduced surgical aggression and scarring. There are several techniques for obtaining the latissimus dorsi flap through small incisions, with the intention of using it as a flap for breast reconstruction. Although the latissimus dorsi flap scar is easily hidden by clothes, patients complain about sensitivity and wound retraction.
The latissimus dorsi flap generated through the endoscopic route enables the most accurate visualization and mobilization of the vascular pedicle, as well as faster postoperative recovery1,5,8,9. The surgery is performed with a lateral incision or with multiple, typically 3, orifices for instruments usage. An optical cavity is required for suitable visualization, and space is required for surgical dissection. Manual retraction and dissection with instruments were initially used for this surgery. However, more recently, a transparent cannula (optical dissector) is used to create multiple tunnels, which can be interconnected with endoscopic dissection to create the optical cavity. Other authors have developed a method in which a dissection balloon is placed in the epimuscular and submuscular fascial planes, thus creating an optical cavity; this cavity, in association with carbon dioxide insufflation, further simplifies latissimus dorsi collection10. As the axillary route has evolved for use in the introduction of breast prosthesis, the endoscopic technique for removing the latissimus dorsi has also evolved in a similar manner. This technique is more expensive, more technically difficult, and requires the use of special materials for suitable performance of the surgery; however, its results tend to last longer11.
Other minimally invasive techniques use 3 incisions ("S"-shaped dorsal, axillary, and anterior) for breast reconstruction in Poland's syndrome12. The authors believe that these incisions are well positioned, with a positive aesthetic result. However, other authors have used 2 incisions: a dorsal "S"-shaped incision and an axillary incision, thus eliminating the anterior incision12. In more conservative studies, an axillary incision was used for tumor removal in the breast and flap rotation of latissimus dorsi, the advantage being the absence of a visible scar in the breast. However, from an oncological viewpoint, this procedure would be restricted to cases where breast skin is preserved13.
Therefore, there are several therapeutic options for correcting thoracic deformities using a latissimus dorsi flap. Currently, many of these techniques are less aggressive and have lower complication rates. The technique of using a vertical incision is a conservative option that should be considered at the time of planning treatment because of its low morbidity, technical ease, and good aesthetic result.
CONCLUSIONS
Reducing the number of incisions for dissecting the latissimus dorsi during breast reconstruction is a very feasible and safe technique. In addition to the aesthetic advantages in the donor area, this technique does not increase cost or surgical time.
REFERENCES
1. da Silva Freitas R, Tolazzi ARD, Santos ALR, Graf RM, Cruz GAO. Poland syndrome. In: Shiffman MA, ed. Breast augmentation: principles and practice. Vol. 1. Berlin: Springer-Verlag; 2008. p. 345-57.
2. Moelleken BR, Mathes SA, Chang N. Latissimus dorsi muscle-musculocutaneous flap in chest-wall reconstruction. Surg Clin North Am. 1989;69(5):977-90.
3. Hammond DC. Latissimus dorsi flap breast reconstruction. Clin Plast Surg. 2007;34(1):75-82.
4. Lin CH, Wei FC, Levin LS, Chen MC. Donor-site morbidity comparison between endoscopically assisted and traditional harvest of free latissimus dorsi muscle flap. Plast Reconstr Surg. 1999;104(4):1070-7.
5. Guemes A, Sousa R, Cachón R, Valcarreres P, Rufas M, Gonzalo A, et al. Cirugía mamaria mínimamente invasiva: reconstrucción mamaria mediante colgajo muscular puro del gran dorsal. Cir Es. 2008;83(1):85-8.
6. Dixon JM, Venizelos B, Chan P. Latissimus dorsi mini-flap: a technique for extending breast conservation. Breast. 2002;11(1):58-65.
7. Freitas RS, Tolazzi AR, Martins VD, Knop BA, Graf RM, Cruz GA. Poland's syndrome: different clinical presentations and surgical reconstructions in 18 cases. Aesthetic Plast Surg. 2007;31(2):140-6.
8. Missana MC, Pomel C. Endoscopic latissimus dorsi flap harvesting. Am J Surg. 2007;194(2):164-9.
9. Martinez-Ferro M, Fraire C, Saldaña L, Reussmann A, Dogliotti P. Complete videoendoscopic harvest and transposition of latissimus dorsi muscle for the treatment of Poland syndrome: a first report. J Laparoendosc Adv Surg Tech A. 2007;17(1):108-13.
10. Van Buskirk ER, Rehnke RD, Montgomery RL, Eubanks S, Ferraro FJ, Levin LS. Endoscopic harvest of the latissimus dorsi muscle using the balloon dissection technique. Plast Reconstr Surg. 1997;99(3):899-903.
11. Pomel C, Missana MC, Atallah D, Lasser P. Endoscopic muscular latissimus dorsi flap harvesting for immediate breast reconstruction after skin sparing mastectomy. Eur J Surg Oncol. 2003;29(2):127-31.
12. Santi P, Berrino P, Galli A. Poland's syndrome: correction of thoracic anomaly through minimal incisions. Plast Reconstr Surg. 1985;76(4):639-41.
13. Shrotria S. Single axillary incision for quadrantectomy, axillary clearance and immediate reconstruction with latissimus dorsi. Br J Plast Surg. 2001;54(2):128-31.
1. Resident physician of the Plastic and Reconstructive Surgery Department at Hospital de Clínicas of Universidade Federal do Paraná (UFPR), Curitiba, PR, Brazil.
2. Assistant professor IV Plastic and Reconstructive Surgery Department at Hospital de Clínicas of Universidade Federal do Paraná UFPR, plastic surgeon of the Center for Assistance to the Cleft Lip and Palate Patient (CAIF), full member of the Brazilian Society of Plastic Surgery (SBCP), coordinator of the Plastic and Reconstructive Surgery of UFPR, Curitiba, PR, Brazil.
3. Full member of SBCP, plastic surgeon of the Plastic and Reconstructive Surgery Department at Hospital de Clínicas of UFPR, Curitiba, PR, Brazil.
4. Medicine student at UFPR, Curitiba, PR, Brazil.
Correspondence to:
Renato da Silva Freitas
Rua General Carneiro, 180 - 9º andar
Curitiba, PR, Brazil - CEP 80060-900
E-mail: dr.renato.freitas@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: October 16, 2011
Paper accepted: December 8, 2011
Study conducted at the Plastic and Reconstructive Surgery Department of Hospital de Clínicas of Universidade Federal do Paraná (UFPR), Curitiba, PR, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter