

Original Article - Year 2011 - Volume 26 -
Quality of life among children with cleft lips and palates: a critical review of measurement instruments
Qualidade de vida de crianças com fissura labiopalatina: análise crítica dos instrumentos de mensuração
ABSTRACT
BACKGROUND: Multidisciplinary teams that treat patients with cleft lips and palates seek to promote quality of life (QoL) in this population. In this study, we aim to identify instruments in the literature that can be used to assess comprehensive aspects of QoL (related to functionality, aesthetics, and outcomes) for this population.
METHODS: We searched literature on PubMed published between 2001 and 2011 for specific instruments used to evaluate QoL among cleft lip and palate patients using the following keywords: quality of life & oral cleft, quality of life & craniofacial deformities, quality of life & oral cleft speech, voice related quality of life.
RESULTS: We identified 457 papers related to the subject and evaluated the following specific pediatric instruments for assessing QoL among cleft lip and palate patients: Quality of Life Instrument - Craniofacial Surgery (YQOL-CS), Youth Quality of Life Instrument-Facial Differences (YQOL-FD), Child Oral Health Quality of Life Questionnaire (COHQOL), Child Oral Health Impact Profile (COHIP), Pediatric Voice Outcome Surgery (PVOS) and Pediatric Voice-Related Quality of Life Survey (PVRQOL).
CONCLUSIONS: No pediatric QoL instrument exists in the current literature that comprehensively evaluates children with cleft lips and palates, including aspects related to aesthetics, conceptual and perceptual consequences, and functionality (chewing and respiratory systems, and vocal resonance) associated with this important congenital craniofacial anomaly.
Keywords: Quality of life. Cleft palate. Cleft lip. Craniofacial abnormalities.
RESUMO
INTRODUÇÃO: A equipe multidisciplinar que trata crianças portadoras de fissura labiopalatina busca promover qualidade de vida (QV) a essa população. O objetivo do presente trabalho foi identificar, na literatura, instrumentos que possibilitem a avaliação global da QV dessa população, envolvendo aspectos estéticos, funcionais e resposta do indivíduo ao tratamento.
MÉTODO: Foi realizada revisão da literatura disponível no PubMed, no período de 2001 a 2011, em busca de instrumentos específicos para avaliação de QV em crianças portadoras de fissura labiopalatina, com as seguintes palavras-chave (em língua inglesa): quality of life & oral cleft, quality of life & craniofacial deformities, quality of life & oral cleft speech, voice related quality of life.
RESULTADOS: Foram identificados 457 artigos relacionados ao tema. Foram avaliados os seguintes instrumentos específicos para a faixa etária pediátrica utilizados na mensuração da QV de pacientes com fissura labiopalatina: Quality of Life Instrument - Craniofacial Surgery (YQOL-CS), Youth Quality of Life Instrument-Facial Differences (YQOL-FD), Child Oral Health Quality of Life Questionnaire (COHQOL), Child Oral Health Impact Profile (COHIP), Pediatric Voice Outcome Surgery (PVOS) e Pediatric Voice-Related Quality of Life Survey (PVRQOL).
CONCLUSÕES: Não se identificou, na literatura, um instrumento que avaliasse integralmente as crianças com fissura labiopalatina, no que se refere aos aspectos estéticos, às consequências conceituais e perceptuais, bem como a todos os aspectos funcionais (aparelhos mastigatório e respiratório e ressonância vocal) que envolvem essa importante anomalia craniofacial congênita.
Palavras-chave: Qualidade de vida. Fenda palatina. Fenda labial. Anomalias craniofaciais.
Cleft lips and palates are the most prevailing craniofacial deformities; they may affect the lips, nose, alveolar region, and palate. Incidence rates vary according to ethnicity and location of the studied population. In Brazil, it is estimated that one child out of every 1,000 born alive has a cleft lip and palate1. Souza et al.2 studied 12,782 medical records of maternity hospitals and found a prevalence rate for the deformity of 0.47 for every 1,000 children born alive. In the southern part of the country for the period from 1970 to 1974, the prevalence rate was 0.88 for every 1,000 children born alive3.
Currently, the most widely used treatment is lip closure at 3 months of age, and palate closure in a single procedure at 1 year of age. The alveolar bone graft is performed when a patient is between 7 and 9 years old, when the canine teeth are about to erupt. Orthognathic surgery is performed between 13 and 15 years of age. The final surgery for a cleft patient is secondary rhinoplasty, to correct any residual nasal deformity4. A well established treatment protocol may lead to success rates of about 96% in the rehabilitation of cleft patients, and basically depends on three pillars: (a) patient adherence to treatment; (b) severity of the cleft lip and palate; and (c) experience of the multidisciplinary staff.
Failing to take a multidisciplinary approach may lead to a significant reduction in rehabilitation success rates. According to the American Cleft Palate-Craniofacial Association (ACPA) and the Eurocleft Clinical Network (Eurocleft), at a minimum, multidisciplinary staff should be comprised of plastic surgeons, psychologists, odontologists, speech therapists and otorhinolaryngologists5,6. In Brazil, centers dedicated to the treatment of craniofacial diseases should also include two extremely important staff members, a social assistant and a pediatrician, who are responsible for ensuring treatment adherence and providing clinical follow-up services for anemia, undernourishment, or chronic illnesses often associated with cleft lips and palates.
Inadequate treatment may lead to irreversible sequelae, which affect facial function and aesthetic harmony. A hypernasal voice is a serious functional sequela, which may affect a patient's quality of life (QoL). In the same way, facial disharmony and/or facial deformity may lead to psychological and cognitive sequelae. These sequelae can cause stigma and discrimination among peers, and may affect QoL for both patients and their families7.
Methods for measuring treatment results among cleft patients have been presented by numerous authors in recent decades, ranging from visual inspection of the results by peers to anatomical measurement using two-dimensional, and more recently, three-dimensional photographs. Peer verification of surgical results is a subjective method, but has great scientific acceptance when performed following predetermined criteria8,9.
Verifying results using two- or three-dimensional photographs is an objective method of results analysis, although proper equipment and photographic standardization techniques are required10,11. In the same way, instruments for voice and hearing assessment vary from perceptual methods to more objective methods such as nasal-video-endoscopy, Glatzel's mirror, and videofluoroscopy12,13. However, these methods do not record or measure patient self-perceptions; therefore, it is possible for a surgical result to be evaluated as excellent based on measurements and objective scales, yet be deemed poor and insufficient by the patient14. Ultimately, what determines rehabilitation success is a patient's self-perception and evaluation of the treatment result, as well as patient QoL post treatment14.
QoL can be defined as an individual's perception about his or her own position in life from a cultural perspective based on the prevailing system of values, considering objectives, expectations, patterns and concerns15. The goal of this study was to identify instruments in the literature that could enable comprehensive QoL assessment for patients with cleft lips and palates, including aesthetics, functionality, and individual responses to multi-stage treatment.
METHODS
We searched for literature identifying specific QoL assessment instruments for children with cleft lips and palates on the PubMed website for the period from 2001 to 2011 using the following keywords: quality of life & oral cleft, quality of life & craniofacial deformities, quality of life & oral cleft speech and voice related quality of life. This search included QoL measurement instruments that prioritized - together or separately - functionality (vocal resonance assessment) and facial harmony as well as its sequelae and psychological and cognitive consequences.
All papers related to stigma suffered by this pediatric population without the use of QoL measurement instruments were excluded. All studies including the word QoL without measurement instruments were excluded, as well as papers that exclusively assessed the legal guardians, without adequate participation of the children who have this craniofacial deformity. Additionally, we excluded all instruments used in other diseases that may affect the pediatric population (asthma, epilepsy, and cancer).
RESULTS
We identified 457 papers related to the topic. The most widely used questionnaires for assessing QoL in cleft patients were the Generic Children's Quality of Life (KINDL), initially published in German, and the Health-Related Quality of Life (HRQoL)16-19. However, since we aimed to identify specific instruments, such instruments were not subjected to critical review.
Only two specific questionnaires were used for measuring QoL among children with cleft lips and palates: the Youth Quality of Life Instrument - Craniofacial Surgery (YQOL-CS), which aims to assess, from an individual perspective, the impact of surgery on an individual's life20; and the Youth Quality of Life Instrument - Facial Differences (YQOL-FD), which includes six domains that assess the negative consequences of facial deformity on an individual's life (self-image, discrimination, and stigmas that the facial deformity may possibly generate, in addition to the capacity for addressing possible problems associated with the facial deformity)21.
We also identified questionnaires that assess the status of the oral system in addition to perceptual self-assessment that can be used to measure QoL for children with cleft lips and palates. The Child Oral Health Quality of Life Questionnaire (COHQOL) includes five domains that assess a child from his or her own perspective with regard to oral symptoms stemming from chronic or congenital diseases that affect the oral cavity (the other domains cover functional and emotional aspects and self-esteem, as well as an individual's relationship with society and the environment)22. Finally, the Child Oral Health Impact Profile (COHIP) incorporates the domains presented by COHQOL and adds two domains that assess a child's perspective on his or her school environment, primarily in terms of self-image23.
Questionnaires that assess QoL among children with vocal resonance deficits may also be useful for measuring QoL among children with cleft lips and palates; such instruments include the Pediatric Voice Outcome Survey (PVOS)24 and the Pediatric Voice-Related Quality of Life Survey (PVRQOL)25. QoL measurement instruments for patients with cleft lips and palates should include domains that assess both anatomical harmony of the face and chewing and speech function. Congenital and acquired anatomical changes that alter facial anatomy may impact self-perception and perceptions of social and school environments. Speech and chewing difficulties, occasionally identified in cleft patients, may generate significant cognitive sequelae. Therefore, instruments that aim to measure the QoL of these patients should try to identify, by means of their respective domains, the negative impact that the craniofacial deformity may cause the individual in personal, social, and school contexts. The instruments described and mentioned in this study assess, in an independent manner, the negative impact of the craniofacial deformity on the individual either globally and specifically for various factors that may cause dissatisfaction with certain situations and/or anatomical conditions.
DISCUSSION
QoL measurement instruments have been expanded and popularized over the last 10 years. Scientific acknowledgment that QoL measurement instruments may be used to assess the results and effectiveness of certain therapies or surgical techniques made knowledge of this tool essential for multidisciplinary staff. Questionnaires that assess QoL among children with cleft lips and palates should try to measure three basic aspects of their lives:
1. Functionality, including chewing; breathing; and vocal resonance (i.e., identify problems caused by hypernasal voice);
2. Aesthetics, including individual responses to peers in either social or school environments, as well as individual responses to disease-related stigma and discrimination; and
3. Individual responses to multi-stage treatment, with the objective being to detect treatment response and adherence and potential for treatment discontinuation.
The QoL measurement instruments identified in this study take these three pillars into consideration, which are essential for verifying an individual's satisfaction with his or her life. Cleft lips and palates are the most frequent craniofacial congenital deformities. It is interesting to note that the majority of craniofacial deformities also have shape and functional deficits. Rare Tessier cleft and syndromic craniosynostosis are examples of diseases whose populations may have difficulties with speech, hearing, neurocognitive development, and facial and body harmony. Hand deformities are the most frequent anomalies associated with craniofacial deformities. These instruments will be able to help plastic surgeons who work in this field to identify anatomical variables that may influence QoL for a portion of the population with congenital craniofacial deformities, in either the preoperative or postoperative period, and ultimately contribute to enhancing techniques that may help improve an individual's satisfaction with surgical results.
We did not identify a single instrument in the literature that could comprehensively assess (using the three aspects mentioned earlier) QoL for individuals with cleft lips and palates. The YQOL-FD includes six domains and evaluates the consequences of craniofacial deformity in terms of the interactions and reactions of an individual to herself and her peers. The domains of this questionnaire aim to assess feelings related to the craniofacial deformity, including anger, reluctance, stigma, isolation, intimacy, confidence, positive outcomes, self-image, and negative outcomes. This questionnaire, although still in the validation stage, was not developed to assess functional aspects of, and individual responses to, multi-stage treatment21. The YQOL-CS aims to assess acceptance and benefits of plastic surgery among individuals with craniofacial deformities20,21.
The COHIP was developed to measure the well-being and QoL of children with any deformity that may affect chewing function, and the deleterious consequences and effects of missing teeth or an anatomically abnormal smile23. Among the congenital deformities that most frequently affect chewing function, the most prevalent is cleft lip and palate. Missing teeth are observed in 70% of those with completely cleft lips and palates, which may affect both function and appearance26-28. This instrument, which has five domains, might be the most complete assessment for children with cleft lips and palates, since it evaluates chewing function, feelings about the face, interactions with peers, well-being and self-image. However, this instrument does not assess vocal resonance and acceptance, adherence to, and benefits of treatment to the individual23.
The COHQOL questionnaire was developed by revising a survey for individuals with specific diseases affecting the chewing system, but who are otherwise considered normal, and using it to measure QoL among patients with a wide array of orofacial deformities22. Several versions of the questionnaire exist. One version is answered by the legal guardians of children between 6 and 14 years old, and two others are answered by the children themselves, one by 8- to 10-year-olds, and one by 11- to 14-year-olds22,29,30. The main questionnaire has 35 items divided into five domains, and assesses oral health, functional well-being, social/emotional well-being, responses to the school environment, and self-image. This questionnaire does not assess an individual's adherence to treatment satisfaction with surgery and the functional and aesthetic benefits achieved in the immediate and late postoperative periods22,29,30.
Vocal resonance is an essential item for comprehensive rehabilitation of patients with cleft lips and palates. It is believed that success rates in the treatment of cleft patients may reach 96% when treatment is performed in a multidisciplinary manner and in compliance with well-established treatment protocols. However, patients who are not taken to specialized centers often have irreversible sequelae. One of the most serious sequelae is a hypernasal and unintelligible voice, which invariably leads to a fear of speaking and communicating, which results in social isolation problems. The PVOS and PVRQOL questionnaires, initially developed and validated for administration among the adult population, aim to assess and measure social, emotional, physical, and functional aspects of the changed voice. These measures were subsequently validated and adapted for a pediatric population to measure well-being and QoL among children with otorhinolaryngologic diseases24,25. These questionnaires may be applicable for measuring vocal resonance among patients with cleft lips and palates, cleft palates or other syndromes where cleft palate is part of the clinical spectrum of the disease (e.g., Apert syndrome and Pierre Robin sequence). Both questionnaires were developed to be answered by parents or legal guardians. However, parents may evaluate the problem differently than their children, a difference that may directly affect the accuracy and trustworthiness of these questionnaires. The authors of these questionnaires obviously disagree with this statement, stating that parental assessment of the functional status of the vocal resonance of their children is quite trustworthy and directly correlates with their assessment of the problem14,24,25.
CONCLUSIONS
Vocal resonance is the most important element in the rehabilitation of children with cleft lips and palates. Resonance alteration may directly affect QoL among this population. Questionnaires that directly assess children's opinions about their voices may yield important data to help multidisciplinary staff members rehabilitate and socially integrate this population.
We did not identify a single instrument in the literature that could comprehensively assess perceptions of children with cleft lips and palates, including: aesthetics and associated conceptual and perceptual consequences; functional deficits in chewing, breathing, and vocal resonance; and treatment benefits, which would certainly and directly impact patient adherence to treatment and satisfaction with multidisciplinary staff performance. Therefore, new comprehensive QoL questionnaires and measurement instruments must be developed to assess all these aspects using a single instrument.
All QoL questionnaires mentioned in this manuscript can be useful for preoperative planning. Therefore, we propose an algorithm for deciding among these questionnaires, which may also be used for patients with other craniofacial deformities in which speech, hearing, and chewing ability are impaired. We emphasize the need to use all three instruments to measure self-perceptions, functionality, and interactions with peers in social and school environments, and to verify possible variables that may interfere with patient adherence to proposed treatments among individuals with craniofacial deformities. The algorithm presented in Figure 1 may be used to help plastic surgeons decide which QoL measurement instruments to use for patients with cleft lips and palates and/or craniofacial deformities, based on the respective priorities of facial harmony, self-image, functionality/functional deficits, adherence to treatment, interactions with peers in social and school environments, and related impacts and consequences.
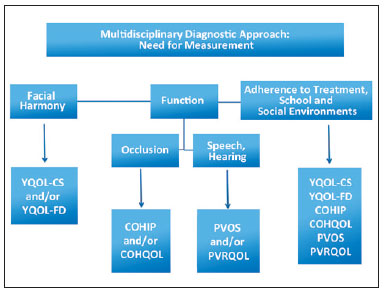
Figure 1 - Algorithm for deciding which QoL measurement instruments to use for patients with cleft lips and palates.
REFERENCES
1. Nagem-Filho H, Moraes N, Rocha RGF. Contribuição para o estudo da prevalência das más formações congênitas lábio-palatais na população escolar de Bauru. Rev Fac Odontol São Paulo. 1968;6(2):111-28.
2. Souza JMP, Buchalla CM, Laurenti R. Estudo da morbidade e da mortalidade perinatal em maternidades. III - Anomalias congênitas em nascidos vivos. Rev Saúde Pública. 1987;21(1):5-12.
3. Cândido TT. Epidemiologia das fendas de lábio e/ou palato: estudo de recém-nascidos em dois hospitais de Porto Alegre, no período de 1970 a 1974 [tese de doutorado]. Porto Alegre: Universidade Federal do Rio Grande do Sul; 1978.
4. Alonso N, Tanikawa DYS, Lima Junior JE, Rocha DL, Sterman S, Ferreira MC. Fissuras labiopalatinas: protocolo de atendimento multidisciplinar e seguimento longitudinal em 91 pacientes consecutivos. Rev Bras Cir Plást. 2009;24(2):176-81.
5. Shaw WC, Semb G, Nelson P, Brattström V, Mølsted K, Prahl-Andersen B, et al. The Eurocleft project 1996-2000: overview. J Craniomaxillofac Surg. 2001;29(3):131-40.
6. Strauss RP. Cleft palate and craniofacial teams in the United States and Canada: a national survey of team organization and standards of care. The American Cleft Palate-Craniofacial Association (ACPA) Team Standards Committee. Cleft Palate Craniofac J. 1998;35(6):473-80.
7. Broder HL. Psychological research of children with craniofacial anomalies: review, critique, and implications for the future. Cleft Palate Craniofac J. 1997;34(5):402-4.
8. Bearn DR, Sandy JR, Shaw WC. Photogrammetric assessment of the soft tissue profile in unilateral cleft lip and palate. Cleft Palate Craniofac J. 2002;39(6):597-603.
9. Tanikawa DYS, Alonso N, Rocha DL. Modificação na rinoqueiloplastia primária do paciente com fissura labial unilateral. Rev Bras Cir Plást. 2010;25(1):30-7.
10. Raposo-do-Amaral CE. Avaliação do percentual de assimetria labial e nasal em pacientes com fissura labiopalatina submetidos a queiloplastia primária. Rev Bras Cir Plást. 2010;25(1):38-48.
11. Arantes HL, Silva RFP, Mélega JM. Simetria nasal após a realização de rinoplastia associada à queiloplastia em crianças com fissura labial e labiopalatal. Rev Bras Cir Plast. 2011;26(1):48-53.
12. Okazaki K, Satoh K, Kato M, Iwanami M, Ohokubo F, Kobayashi K. Speech and velopharyngeal function following maxillary advancement in patients with cleft lip and palate. Ann Plast Surg. 1993;30(4):304-11.
13. Dotevall H, Lohmander-Agerskov A, Ejnell H, Bake B. Perceptual evaluation of speech and velopharyngeal function in children with and without cleft palate and the relationship to nasal airflow patterns. Cleft Palate Craniofac J. 2002;39(4):409-24.
14. Klassen AF, Stotland MA, Skarsgard ED, Pusic AL. Clinical research in pediatric plastic surgery and systematic review of quality-of-life questionnaires. Clin Plast Surg. 2008;35(2):251-67.
15. Fleck MP, Louzada S, Xavier M, Chachamovich E, Vieira G, Santos L, et al. Application of the Portuguese version of the instrument for the assessment of quality of life of the World Health Organization (WHOQOL-100). Rev Saúde Pública. 1999;33(2):198-205.
16. Sagheri D, Ravens-Sieberer U, Braumann B, von Mackensen S. An evaluation of Health-Related Quality of Life (HRQoL) in a group of 4-7 year-old children with cleft lip and palate. J Orofac Orthop. 2009;70(4):274-84.
17. Sinko K, Jagsch R, Prechtl V, Watzinger F, Hollmann K, Baumann A. Evaluation of esthetic, functional, and quality-of-life outcome in adult cleft lip and palate patients. Cleft Palate Craniofac J. 2005;42(4):355-61.
18. Kramer FJ, Gruber R, Fialka F, Sinikovic B, Hahn W, Schliephake H. Quality of life in school-age children with orofacial clefts and their families. J Craniofac Surg. 2009;20(6):2061-6.
19. Bressmann T, Sader R, Ravens-Sieberer U, Zeilhofer HF, Horch HH. Quality of life research in patients with cleft lip and palate: preliminary results. Mund Kiefer Gesichtschir. 1999;3(3):134-9.
20. Edwards TC, Patrick DL, Topolski TD, Aspinall CL, Mouradian WE, Speltz ML. Approaches to craniofacial-specific quality of life assessment in adolescents. Cleft Palate Craniofac J. 2005;42(1):19-24.
21. Patrick DL, Topolski TD, Edwards TC, Aspinall CL, Kapp-Simon KA, Rumsey NJ, et al. Measuring the quality of life of youth with facial differences. Cleft Palate Craniofac J. 2007;44(5):538-47.
22. Jokovic A, Locker D, Stephens M, Kenny D, Tompson B, Guyatt G. Validity and reliability of a questionnaire for measuring child oral-health-related quality of life. J Dent Res. 2002;81(7):459-63.
23. Broder HL, Wilson-Genderson M. Reliability and convergent and discriminant validity of the Child Oral Health Impact Profile (COHIP Child's version). Community Dent Oral Epidemiol. 2007;35 Suppl 1:20-31.
24. Boseley ME, Cunningham MJ, Volk MS, Hartnick CJ. Validation of the pediatric voice-related quality-of-life survey. Arch Otolaryngol Head Neck Surg. 2006;132(7):717-20.
25. Hartnick CJ, Volk M, Cunningham M. Establishing normative voice-related quality of life scores within the pediatric otolaryngology population. Arch Otolaryngol Head Neck Surg. 2003;129(10):1090-3.
26. Harper DC. Children's attitudes to physical differences among youth from Western and non-Western cultures. Cleft Palate Craniofac J. 1995;32(2):114-9.
27. Mulliken JB. The changing faces of children with cleft lip and palate. N Engl J Med. 2004;351(8):745-7.
28. Aizenbud D, Camasuvi S, Peled M, Brin I. Congenitally missing teeth in the Israeli cleft population. Cleft Palate Craniofac J. 2005;42(3):314-7.
29. Jokovic A, Locker D, Guyatt G. Short forms of the Child Perceptions Questionnaire for 11-14-year-old children (CPQ11-14): development and initial evaluation. Health Qual Life Outcomes. 2006;4:4.
30. Jokovic A, Locker D, Tompson B, Guyatt G. Questionnaire for measuring oral health-related quality of life in eight- to ten-year-old children. Pediatr Dent. 2004;26(6):512-8.
1. Plastic surgeon, full member of the Brazilian Society of Plastic Surgery (SBCP), head of the Chapter of Craniofacial Surgery of SBCP, full member of the Brazilian Association of Craniomaxillofacial Surgery (ABCCMF), vice-president of the Hospital de Crânio e Face SOBRAPAR, Campinas, SP, Brazil.
2. Pediatrician, psychiatrist of Childhood and Adolescence, PhD from the School of Medicine of Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil.
3. Full professor, head of the Craniofacial Surgery Group of the Discipline of Plastic Surgery at Hospital das Clínicas of FMUSP, full member of SBCP and ABCCMF, São Paulo, SP, Brazil.
Correspondence to:
Cassio Eduardo Raposo do Amaral
Av. Dr. Moraes Salles, 2.655 - Nova Campinas
Campinas, SP, Brazil - CEP 13092-111
E-mail: cassioraposo@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: August 21, 2011
Paper accepted: October 10, 2011
Study conducted at Hospital de Crânio e Face SOBRAPAR, Campinas, SP, Brazil, and at Hospital das Clínicas of the School of Medicine of Universidade de São Paulo (HCFMUSP), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter