

Original Article - Year 2011 - Volume 26 -
Comparative study among cleft patients with velopharyngeal insufficiency treated with speech therapy and pharyngoplasty
Estudo comparativo entre pacientes fissurados portadores de insuficiência velofaríngea tratados com fonoterapia e faringoplastia
ABSTRACT
BACKGROUND: Inadequacy of speech and voice due to velopharyngeal insufficiency is a major stigma for cleft patients. Therefore, the study of this clinical condition is essential to improve the development and social relations of children with this ailment. This study aimed to assess alterations in the speech, velopharyngeal sphincter, and larynx of patients with cleft palate and cleft lip and palate who underwent to lip closure, palatoplasty, and speech therapy and developed transitory velopharyngeal insufficiency. Furthermore, these patients were compared with cleft palate and cleft lip and palate patients who developed persistent velopharyngeal insufficiency treated with lip closure, palatoplasty, speech therapy, pharyngoplasty, and complementary speech therapy.
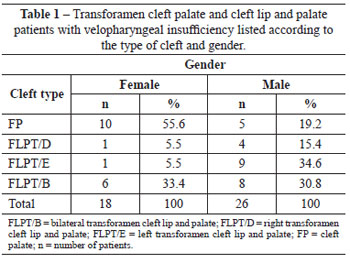
METHODS: From June 1997 to May 2002, 132 cleft palate and cleft lip and palate patients aged between 4 years 11 months and 19 years 3 months with transitory velopharyngeal insufficiency and persistent velopharyngeal insufficiency were assessed. After applying inclusion and exclusion criteria, 44 patients, 18 females and 26 males, were divided into 2 groups: group I, 20 patients who underwent lip closure, palatoplasty and speech therapy; and group II, 24 patients who underwent lip closure, palatoplasty, speech therapy, pharyngoplasty, and complementary speech therapy. Speech therapy consisted of articulatory therapy of oral airflow, myofunctional therapy, rapid phonemic acquisition technique, and voice therapy. Surgical treatment consisted of producing a flap from the pharynx posterior wall of the upper pedicle.
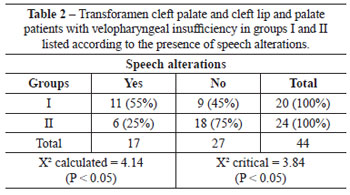
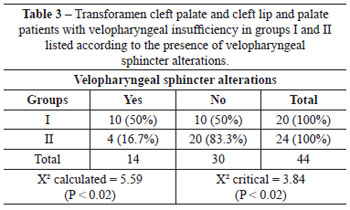
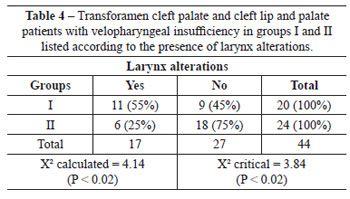
RESULTS: Alterations in speech, the velopharyngeal sphincter, and the larynx were more frequent in group I than in group II.
CONCLUSIONS: Cleft patients with persistent velopharyngeal insufficiency should be treated with pharyngoplasty and complementary speech therapy in order to correct alterations in speech, the velopharyngeal sphincter, and the larynx.
Keywords: Velopharyngeal insufficiency. Larynx. Cleft palate. Humans.
RESUMO
INTRODUÇÃO: A inadequação da fala e da voz decorrente da insuficiência velofaríngea é o principal estigma do paciente fissurado; assim, o estudo dessa condição clínica é fundamental, proporcionando melhor desenvolvimento das crianças e de suas relações sociais. O objetivo do presente estudo é avaliar alterações fonoaudiológicas, do esfíncter velofaríngeo, da laringe de pacientes fissurados palatais e labiopalatais tratados com queiloplastia, palatoplastia e fonoterapia, que desenvolveram insuficiência velofaríngea transitória, e fissurados palatais e labiopalatais, que desenvolveram insuficiência velofaríngea persistente tratados com queiloplastia, palatoplastia, fonoterapia, faringoplastia e fonoterapia complementar.
MÉTODO: No período de junho de 1997 a maio de 2002, foram avaliados 132 fissurados palatais e labiopalatais que desenvolveram insuficiência velofaríngea transitória e insuficiência velofaríngea persistente, com idade entre 4 anos e 11 meses e 19 anos e 3 meses. Observando-se os critérios de inclusão e exclusão, 44 pacientes, sendo 18 do gênero feminino e 26 do gênero masculino, foram divididos em 2 grupos: grupo I, 20 pacientes submetidos a queiloplastia, palatoplastia e fonoterapia; e grupo II, 24 pacientes submetidos a queiloplastia, palatoplastia, fonoterapia, faringoplastia e fonoterapia complementar. O tratamento fonoaudiológico consistiu de terapia articulatória de fluxo aéreo bucal, terapia miofuncional, técnica de aquisição fonêmica rápida e terapia de voz. O tratamento cirúrgico consistiu de confecção de retalho da parede posterior da faringe, de pedículo superior.
RESULTADOS: As alterações fonoaudiológicas, do esfíncter velofaríngeo e da laringe foram mais frequentes nos pacientes do grupo I, quando comparados aos do grupo II.
CONCLUSÕES: Pacientes fissurados que evoluíram para insuficiência velofaríngea persistente devem ser tratados com faringoplastia e fonoterapia complementar para correção das alterações fonoaudiológicas, do esfíncter velofaríngeo e da laringe.
Palavras-chave: Insuficiência velofaríngea. Laringe. Fissura palatina. Humanos.
The inadequacy of speech and voice arising from velopharyngeal insufficiency is a major stigma for cleft patients. Therefore, the study of this clinical condition is essential to treat the disease, thereby improving the development of children with this ailment and improving their relations with family, friends, in school and in the community.
In order to carry out treatment, it is important to set up a multispecialty team consisting of a plastic surgeon, speech therapist, dental surgeon, and otorhinolaryngologist. Furthermore, pediatric, nutritional, and psychological follow-up are required. The entire team should be oriented with the treatment protocols.
The anatomical structures of the velopharyngeal sphincter will remain unchanged in approximately 20% of patients treated for cleft palate and cleft lip and palate, resulting in total or partial impairment of function, regardless of the correct performance of lip closure, palatoplasty, and speech therapy1.
Nasofibroscopy is an important exam for diagnosing velopharyngeal insufficiency, making it possible for the patient to use speech therapy for correction of voice and speech changes by direct visualization of the movements of the velopharyngeal sphincter2,3.
The first assessment of the velopharynx by means of rhinoscopy was performed in 18694. It was verified that complete closure did not always occur during the pronunciation of /a/, /o/, and /u/. Furthermore, the formation of a crease in the posterior wall of the pharynx was observed in individuals with cleft palate and cleft lip and palate. This structure was subsequently called the Passavant crease.
In 1973, the velopharyngeal space received was recognized as a real sphincter5.
Laryngeal alterations in patients with cleft palate and cleft lip and palate were studied in 1969, revealing implications for future studies. Children with a moderately suitable velopharyngeal mechanism may produce compensatory movements during speech to counterbalance velopharyngeal insufficiency, causing laryngeal alterations6.
In 1961, the velopharyngeal sphincter was studied in normal patients by means of cineradiographies, and synchronized speech was studied by means of spectrography. The author of this study considered 20 mm2 as the maximum area for velopharyngeal competence7.
In 1973, a pharyngoplasty technique that used a myomucosal flap of the upper pedicle of the pharynx upper wall was described8. The control of spaces lateral to the flap was possible with the aid of a vesical probe Nº 14 introduced in each nostril, generating a hole in each side of the flap and the lateral wall of the pharynx with an area of 10 mm2, totaling 20 mm2. Therefore, wide flaps were obtained in patients whose velopharyngeal space diameter was large whereas narrow flaps were obtained in patients with small diameters. Flaps from the nasal plane of the uvula and soft palate were associated for coverage of the pharyngeal flap open area.
In 2005, a technique that associated the intravelar veloplasty9,10 to the inclusion of the upper part of the posterior pillars of amygdalin cavities and of the palatopharyngeal muscles11 was published. New techniques continue to be developed for velopharyngeal insufficiency correction12.
This paper aimed to assess phono-articulatory alterations of the velopharyngeal sphincter and larynx in cleft patients with velopharyngeal insufficiency treated with speech therapy and who underwent lip closure and palatoplasty. Furthermore, the results from these patients were compared with results from patients who developed persistent velopharyngeal insufficiency treated with pharyngoplasty and complementary speech therapy.
METHODS
In the period from June 1997 to May 2002, 132 patients with transforamen cleft palate and cleft lip and palate were assessed. The patients in this group ranged in age from 4 years 11 months to 19 years 3 months and consisted of 54 females and 78 males. The patients had velopharyngeal insufficiency and were from the outpatient service of the Plastic Surgery of Hospital Municipal Infantil Menino Jesus (São Paulo, SP, Brazil).
Inclusion Criteria
The study included patients who underwent surgical treatment for cleft closure according to the following techniques:
a) in cases of unilateral transforamen cleft lip and palate, lip closure was performed by advancement and rotation of flaps in a single procedure13;
b) in cases of bilateral transforamen cleft lip and palate, lip closure was performed in three procedures14;
c) in cases of unilateral and bilateral transforamen cleft lip and palate, palatoplasty15 was associated to the vomerine flap16 in the hard palate and to intravelar veloplasty9,10 in the soft palate;
d) in cases of isolated cleft palate, palatoplasty15 was always associated with intravelar veloplasty9,10.
Exclusion Criteria
The following patients and conditions were excluded from the study:
a) patients who underwent secondary palatoplasty and/or the presence of a fistula was detected;
b) patients with palatal or lip and palate fistula associated with a genetic syndrome;
c) other malformations and facial trauma;
d) associated diseases;
e) low intelligence quotient according to age;
f) loss of or altered hearing function.
After observing the inclusion and exclusion criteria, 44 patients were selected of which 18 were female and 26 were male (Table 1).
Patient assessment was performed according to the sequence described below.
1) Speech assessment:a) assessment was performed through spontaneous and stimulated speech;
b) voice assessment was performed through hearing-perceptual analysis;
c) assessment of the soft palate at rest and at motion was performed during the pronunciation of the vowel /a/.
In voice and speech assessments, which were performed by two speech therapists, the presence or absence of hypernasality, nasal air escape, and articulatory disorders was verified.
Instrumental Assessment of the Velopharyngeal Sphincter and Larynx
Velopharyngeal sphincter assessment was performed by observing the following protocol17: the patients slowly pronounced the vowels /a/, /e/, /i/, /o/, and /u/ and the consonant /s/ and slowly counted from 1 to 10. Furthermore, the patients pronounced the following sentences: "papai fez a pipa" (daddy made the kite), "Kiki gosta de chá" (Kiki likes tea), "Juju saiu cedo" (Juju left early), and "o cachorro chegou da chuva" (the dog arrived from the rain).
The patients were asked to produce the sound of long /i/ and /é/ while the larynx was examined.
All examinations were recorded on VHS tapes.
The examinations were carried out at the Institute of Otorhinolaryngology and at the Discipline of Pediatric Otorhinolaryngology of UNIFESP/EPM (São Paulo, SP, Brazil).
The following aspects were assessed in the velopharyngeal sphincter examination: closure in deglutition, extension of lateral wall movements, the presence of a crease in the posterior wall of the pharynx and its level against the velar closure, and adenoid hypertrophy in relation to the velopharyngeal space.
In the larynx examination, we sought to observe the presence of anteroposterior or median constriction, triangular and fusiform glottic apertures, and the presence or absence of vocal nodules.
For comparison purposes, the studied population was divided in two groups:
group I, consisting of 20 patients, included 8 with cleft palate who underwent palatoplasty and speech therapy and 12 with transforamen cleft lip and palate who underwent lip closure, palatoplasty, and speech therapy - the speech treatment for the correction of hypernasality and articulatory disorders involved articulatory therapy of buccal air flow18, myofunctional therapy19, the fast phonemic acquisition technique18, and voice therapy; and group II, consisting of 24 patients, included 7 with cleft palate who underwent palatoplasty and speech therapy and 17 with transforamen cleft lip and palate who underwent lip closure, palatoplasty, and speech therapy and developed persistent velopharyngeal insufficiency treated with pharyngoplasty and complementary speech therapy.
The surgical treatment performed for correcting hypernasality involved the production of a flap of the pharynx posterior wall of the upper pedicle while observing the control of spaces between the flap and the lateral walls of the pharynx7,20,21 (Figures 1 to 10).
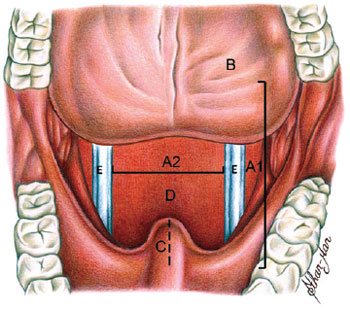
Figure 1 - Marking the width and length of the pharyngeal flap. A1 = flap length; A2 = flap width; B = tongue; C = uvula; D = posterior wall of the pharynx; E = catheter.
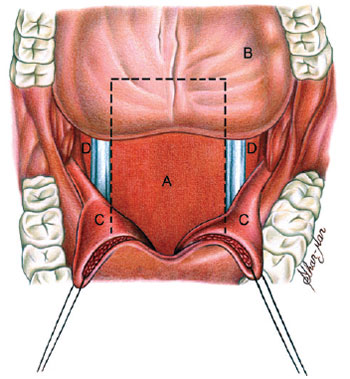
Figure 2 - Layout of the pharyngeal flap. A = flap; B = tongue; C = uvula; D = posterior wall of the pharynx.
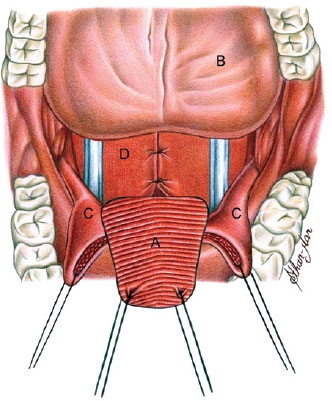
Figure 3 - Incision of the uvula and soft palate and pharyngeal flap raising. A = flap; B = tongue; C = uvula; D = posterior wall of the pharynx.
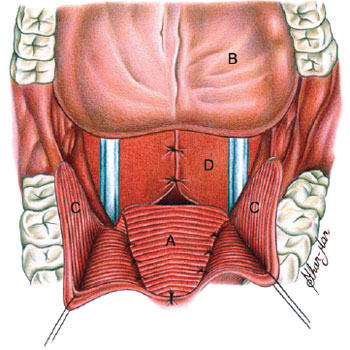
Figure 4 - Suture of the pharyngeal flap in the soft palate. Production of flaps of the nasal plane of the uvula. A = flap; B = tongue; C = uvula; D = posterior wall of the pharynx.
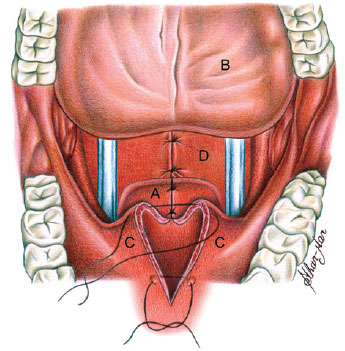
Figure 5 - Suture of uvula flaps over the pharyngeal flap. A = flap; B = tongue; C = uvula; D = posterior wall of the pharynx.
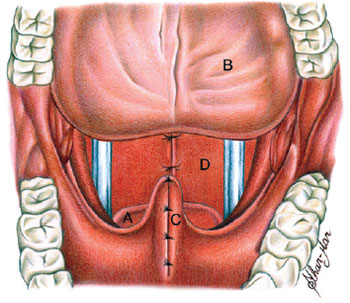
Figure 6 - Suture of the oral plane of the uvula. A = flap; B = tongue; C = uvula; D = posterior wall of the pharynx.
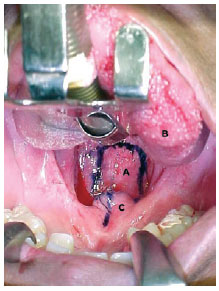
Figure 7 - Surgical procedure. Marking the flap of the pharynx posterior wall. A = marked pharyngeal flap, where length corresponds to the distance marked from the soft palate to the posterior wall of the pharynx; B = tongue; C = marked uvula and soft palate.
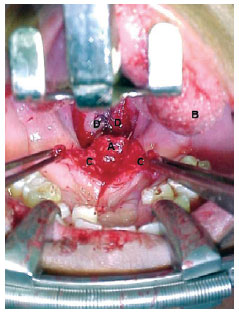
Figure 8 - Surgical procedure. Suture of the pharyngeal flap in the soft palate. A = pharyngeal flap sutured in the soft palate; B = tongue; C = flaps of the nasal plane of the uvula; D = posterior wall of the reconstructed pharynx.
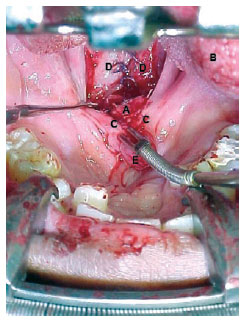
Figure 9 - Surgical procedure. Coverage of the open area of the pharyngeal flap. A = pharyngeal flap sutured in the soft palate; B = tongue; C = flaps of the nasal plane of the uvula, sutured over the open area of the pharyngeal flap; D = posterior wall of the reconstructed pharynx; E = oral plane of the uvula.
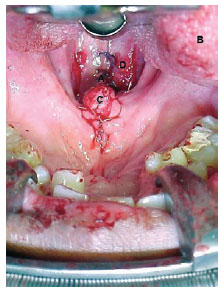
Figure 10 - Surgical procedure. Reconstruction of the uvula oral plane. A = pharyngeal flap covered by flaps of the uvula nasal plane; B = tongue; C = reconstructed uvula; D = posterior wall of the reconstructed pharynx.
Groups I and II were compared by means of speech and pharyngolaryngoscopic assessment with the purpose of observing possible improvements in hypernasality, nasal air escape, articulatory disorders, alterations of the velopharyngeal sphincter, and glottic alterations that were observed before the treatment.
The research plan was submitted and approved by the Ethics Committee of UNIFESP/EPM, and an informed consent form was signed by a parent or guardian.
For analysis, we used the chi-square test or the exact test of Fisher22 for 2×2 tables, with the purpose of comparing both groups with regard to the presence of each of the mentioned alterations.
In all tests, the significance level was established at 0.05 or 5%, and the significant values are marked with an asterisk.
RESULTS
The chi-square test22 demonstrated significantly larger frequencies of alterations of speech, the velopharyngeal sphincter, and the larynx in group I (Tables 2 to 4).
DISCUSSION
It is difficult to identify the incidence of cleft palate and cleft lip and palate in Brazil because there is no adequate census. It is important to highlight that the incidence tends to increase either by intensification of environmental factors that determine the deformity or by addition of the following factors: (a) decrease of perinatal mortality due to improved puericulture and pediatric techniques that ensure better care for the cleft patient; (b) mortality decrease during the surgical procedures due to better equipment, drugs, and anesthetic techniques; (c) better pre-natal care; and (d) better quality of the surgical technique. These factors result in the integration of cleft patients into society, increasing the possibility that they will marry among themselves and genetically transmit the deformity.
The treatment of cleft lip and palate aims to obtain a result that enables the normal anatomical and functional development of each patient. The inadequacy of speech and voice derived from velopharyngeal insufficiency is a major stigma for cleft patients. Therefore, the study of this clinical condition is essential in order to treat this disease, thereby improving the development of children with this condition and improving their relationships with family, friends, in school, and the community.
Following the description of the anatomical and functional bases of velopharyngeal occlusion by Passavant4 in 1869, and the suggestion that speech can be improved by fixation of the soft palate in the posterior wall of the pharynx, several techniques have been described for this process. In 1973, Hogan8 described a technique that used a myomucosal flap of the upper pedicle of the pharynx posterior wall. The modification introduced by Hogan was important because it achieved control of the spaces between the flap and lateral walls of the pharynx by introducing a vesical probe Nº 14 in each nostril. Therefore, each orifice lateral to the flap generated an area corresponding to 10 mm2, totaling 20 mm2. In 1961, Bjork7 studied the velopharyngeal sphincter of normal patients by means of cineradiographies and synchronized speech and reported that 20 mm2 is the maximum area for velopharyngeal competence. Another modification introduced by Hogan was coverage of the open area of the pharyngeal flap using flaps from the nasal plane of the uvula and soft palate. These modifications allowed obtainment of wide flaps for correction of the velopharyngeal insufficiency in patients with a velopharyngeal space with a large diameter and obtainment of narrow flaps in patients with a small diameter.
The results achieved in several world centers that specialize in the treatment of patients with cleft palate and cleft lip and palate are superior in patients who undergo palatoplasty before 12 years of age. At the Hospital Municipal Infantil Menino Jesus, palatoplasties are frequently carried out after 18 months of age and, in some cases, after 24 months of age. This range is mainly because of the time that elapses between childbirth and the first consultation.
In group I, the results of patients who underwent palatoplasty at up to 2 years of age were modestly better (37.5% success rate) than in patients who underwent palatoplasty after 2 years of age (33.3% success rate). In group II, the results were much better under the same age conditions (80% versus 57.1%). These outcomes could not be analyzed statistically because of the dimension of the sample. We observed an 81.8% success rate in patients that underwent pharyngoplasty between 5 and 10 years of age and a 53.8% success rate in patients that underwent this procedure at more than 10 years of age. Statistical analysis could not be performed because of the dimension of the sample.
At the Hospital Municipal Infantil Menino Jesus, the treatment of cleft patients is carried out by a multispecialty team; this is consistent with the approach of Centers of Cleft Treatment all over the world.
The adaptation of movements of the pharynx lateral wall to the pharyngeal flap was described in 1999. A statistically significant adaptation of adduction of the pharynx lateral walls was observed after the pharyngoplasty23.
In group II, 20 (83.33%) patients had coronal-type closure and 4 (16.67%), had circular type closure. Following treatment, coronal-type closure remained in 14 (58.34%) patients, circular-type closure remained in 5 (20.83%) patients, and circular-type closure with a Passavant ridge was observed in 5 (20.83%) patients. These results are consistent with a study conducted in 198024. Patients who undergo pharyngoplasty are able to change the movement of the lateral walls, and in some cases, the configuration of these movements may be altered.
For the purpose of statistical analysis, the cases that evolved without hypernasality, nasal air escape, articulatory disorders, vocal crease nodules, constriction, and glottic aperture and with suitable closure of the velopharyngeal sphincter were considered successful, whereas the presence of one of these undesired alterations was considered a failure.
The presence of these alterations was compared in both groups and the chi-square test22 revealed that the frequencies of all alterations were significantly smaller in group II.
The incidence of vocal disorders in cleft lip and palate and cleft palate pre-school age patients has been studied. Children with moderate or severe hypernasality were statistically proven to have medium hypernasality or normal resonance, especially those children that produced the coup de glotte more often25.
Laryngeal alterations occurred in both group I and group II patients, indicating the need for larynx examination in all patients with velopharyngeal insufficiency.
Prospective studies will be necessary to determine if there is causal relationship between abnormalities of the velopharyngeal sphincter and laryngeal alterations in individuals.
CONCLUSIONS
Cleft patients who undergo lip closure, palatoplasty, and speech therapy and develop persistent velopharyngeal insufficiency should be treated with pharyngoplasty and complementary speech therapy in order to correct alterations in speech, the velopharyngeal sphincter, and the larynx.
ACKNOWLEDGMENTS
To Professor Márcio Abrahão, full professor of the Discipline of Head and Neck Surgery of the Department of Otorhinolaryngology and Head and Neck Surgery of Universidade Federal de São Paulo - São Paulo School of Medicine, for incentive and enthusiasm in all stages of this work.
To Professor Neil Ferreira Novo, assistant professor of the Discipline of Biostatistic of the Department of Preventive Medicine of Universidade Federal de São Paulo - São Paulo School of Medicine, for guidance in the statistical analysis of the study.
To our colleague Dr. Cristina Kohmann von Glehn, for participating in the fibronasopharyngolaryngoscopies, for incentive to conclude this study, and, above all, for her presence at all moments.
To the speech therapist Regianne Weitzberg Breinis, for being available and participating in the discussion of cases and in the diagnosis of velopharyngeal insufficiency in cleft patients.
To the speech therapist Claudia Brandão Onaga, for participating in the discussion of the cases, which guided the treatment of cleft patients.
To Mr. Sthar-Mar de Vasconcelos Silva, for illustrating the works of this study.
REFERENCES
1. Witt PD, O'Daniel TG, Marsh JL, Grames LM, Muntz HR, Pilgram TK. Surgical management of velopharyngeal dysfunction: outcome analysis of autogenous posterior pharyngeal wall augmentation. Plast Reconstr Surg. 1997;99(5):1287-300.
2. Shelton RL, Beaumont K, Trier WC, Furr ML. Videoendoscopic feedback in training velopharyngeal closure. Cleft Palate J. 1978;15(1):6-12.
3. Yamaoka M, Matsuya T, Miyazaki T, Nishio J, Ibuki K. Visual training for velopharyngeal closure in cleft palate patients; a fibrescopic procedure (preliminary report). J Maxillofac Surg. 1983;11(4):191-3.
4. Passavant G. Ueber die verschliessung des schklundes beim sprechen. Arch J Pathol Anat Physiol. 1869;46:1.
5. Skolnick ML, McCall GN, Barnes M. The sphincteric mechanism of velopharyngeal closure. Cleft Palate J. 1973;10:286-305.
6. McWilliams BJ, Bluestone CD, Musgrave RH. Diagnostic implications of vocal cord nodules in children with cleft palate. Laryngoscope. 1969; 79(12):2072-80.
7. Björk L. Velopharyngeal function in connected speech. Acta Radiol Suppl. 1961;202:1-94.
8. Hogan VM. A clarification of the surgical goals in cleft palate speech and the introduction of the lateral port control (l.p.c.) pharyngeal flap. Cleft Palate J. 1973;10:331-45.
9. Braithwaite F, Maurice DG. The importance of the levator palati muscle in cleft palate closure. Br J Plast Surg. 1968;21(1):60-2.
10. Kriens OB. Fundamental anatomic findings for an intravelar veloplasty. Cleft Palate J. 1970;7:27-36.
11. Henriksson TG, Hakelius M, Andlin-Sobocka A, Svanholm H, Low A, Skoog V. Intravelar veloplasty reinforced with palatopharyngeal muscle: a review of a 10-year consecutive series. Scand J Plast Reconstr Surg Hand Surg. 2005;39(5):277-82.
12. Cheng N, Zhao M, Qi K, Deng H, Fang Z, Song R. A modified procedure for velopharyngeal sphincteroplasty in primary cleft palate repair and secondary velopharyngeal incompetence treatment and its preliminary results. J Plast Reconstr Aesthet Surg. 2006;59(8):817-25.
13. Millard DR Jr. Complete unilateral clefts of the lip. Plast Reconstr Surg. 1960;25:595-605.
14. Spina V, Kamakura L, Lapa F. Surgical management of bilateral cleft lip. Ann Plast Surg. 1978;1(5):497-505.
15. Von Langenbeck B. Die uranoplastik mittelst ablösung des mucös-periostalen gaumenüberzuges. Langenbecks Arch Klin Chir. 1861;2:205-11.
16. Pichler H. Über lippen- und gaumenspalten. Disch Z Chir. 1926;1:2-9.
17. Altmann EBC, Lederman H. Videofluoroscopia da deglutição e do esfíncter velo-faríngico: padronização do exame. Pró-Fono. 1990;2(1):9-16.
18. Altmann EBC, Vaz ACN, Farias RALN, Faria MBSP, Khoury RBF, Marques RMF. Tratamento fonoaudiológico. In: Altmann EBC, ed. Fissuras labiopalatinas. 4a ed. Carapicuíba: Pró-Fono; 1997. p. 376-403.
19. Altmann EB. Myofunctional therapy and orthognathic surgery. Int J Orofacial Myology. 1987;13(3):2-12.
20. Levine PA, Goode RL. The lateral port control pharyngeal flap: a versatile approach to velopharyngeal insufficiency. Otolaryngol Head Neck Surg. 1982;90(3 Pt 1):310-4.
21. Araujo Netto BC. Insuficiência velofaríngea em fissurados: tratamento cirúrgico e fonoaudiológico [tese de doutorado]. São Paulo: Universidade Federal de São Paulo; 2007. p. 23.
22. Siegel S, Castellan Jr NJ. Nonparametrics statistics. 2nd ed. New York: McGraw-Hill; 1988. 399p.
23. Karling J, Henningsson G, Larson O, Isberg A. Adaptation of pharyngeal wall adduction after pharyngeal flap surgery. Cleft Palate Craniofac J. 1999;36(2):166-72.
24. Shprintzen RJ, McCall GN, Skolnick ML. The effect of pharyngeal flap surgery on the movements of the lateral pharyngeal walls. Plast Reconstr Surg. 1980;66(4):570-3.
25. Hardin-Jones MA, Jones DL. Speech production of preschoolers with cleft palate. Cleft Palate Craniofac J. 2005;42(1):7-13.
1. Doctor in Sciences at Universidade Federal de São Paulo - School of Medicine of São Paulo (UNIFESP/EPM), São Paulo, SP, physician at the Family Health Program - SPDM/Mauá, Mauá, SP, Brazil.
2. Full professor, associate professor of the Department of Otorhinolaryngology and Head and Neck Surgery of UNIFESP/EPM, São Paulo, SP, Brazil.
Correspondence to:
Belmino Corrêa de Araujo Netto
Rua Morais de Barros, 277 - Campo Belo
São Paulo, SP, Brazil - CEP 04614-000
E-mail: belmino.can@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: June 12, 2011
Paper accepted: October 3, 2011
Study conducted at the Plastic Surgery Service of Hospital Municipal Infantil Menino Jesus, Department of Otorhinolaryngology and Head and Neck Surgery of Universidade Federal de São Paulo - School of Medicine of São Paulo (UNIFESP/EPM), São Paulo, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter