

Original Article - Year 2011 - Volume 26 -
Evaluation of craniofacial growth in patients with cleft lip and palate undergoing one-stage palate repair
Avaliação do crescimento craniofacial em portadores de fissuras labiopalatinas submetidos a palatoplastia em tempo único
ABSTRACT
BACKGROUND: Primary surgeries such as cheiloplasty and palatoplasty interfere with the morphology and physiology of the maxillofacial complex, causing alterations in its growth and development in unilateral cleft lip and palate (UCLP) patients. The aim of the present study was to perform a preliminary analysis of the effects of surgery on maxillofacial growth through an examination of dental arch relationships.
METHODS: Forty-five patients with UCLP who underwent primary surgery for the repair of cleft lip and palate were evaluated. Comparative analysis of plaster models of dental arches was performed by two orthodontists using the Atack index.
RESULTS: Some patients (44.4%) analyzed showed scores of 1 and 2, representing the most favorable maxillofacial growth conditions. The intermediate score (score 3) was found in 40% of patients, while 15.6% showed unfavorable maxillary growth tendencies (scores 4 and 5). The mean score at 4 years of age was 2.62 + 0.98. A correlation between scores 1 and 2 in the present study with those of previous studies resulted in a significant difference (P = 0.23) in comparison to Bongaarts' series, which obtained the best results. Our results for scores 3, 4, and 5 were similar to those of 3 related studies in terms of the percentages obtained, which were better than those of the first study that used the Atack index for the evaluation of primary surgeries.
CONCLUSIONS: The Atack index enabled the analysis of the effects of primary surgery on maxillofacial growth and a comparison with the results obtained by other centers for the treatment of UCLP.
Keywords: Cleft lip. Cleft palate. Maxillofacial development.
RESUMO
INTRODUÇÃO: As cirurgias primárias, queiloplastia e palatoplastia, interferem na morfologia e na fisiologia do complexo maxilofacial, provocando alterações em seu crescimento nos portadores de fissura transforame incisivo unilateral (FTIU). Este estudo tem por objetivo avaliar precocemente os efeitos das cirurgias sobre o crescimento maxilofacial, por meio da relação dos arcos dentários desses pacientes.
MÉTODO: Foram avaliados 45 pacientes portadores de FTIU submetidos a cirurgias primárias de lábio e palato. Foi realizado estudo comparativo de modelos dos arcos dentários decíduos em que a relação maxilomandibular foi avaliada por 2 ortodontistas, que aplicaram o índice Atack.
RESULTADOS: Dentre os pacientes analisados, 44,4% se encontravam nos escores 1 e 2, apresentando condições mais favoráveis de crescimento maxilomandibular. O escore intermediário (escore 3) correspondeu a 40% da amostra e os escores 4 e 5, a 15,6%, apresentando tendência a crescimento desfavorável. A média obtida aos 4 anos de idade foi de 2,62 + 0,98. Ao relacionar os escores 1 e 2 com outros estudos, houve diferença significativa (P = 0,023) comparativamente à série de Bongaarts, que apresentou os melhores resultados. Nos resultados para os escores 3, 4 e 5, observaram-se proporções semelhantes às de três dos estudos relacionados e melhores em relação ao primeiro a utilizar o índice Atack na avaliação de suas cirurgias primárias.
CONCLUSÕES: A aplicação do índice Atack possibilitou a análise dos resultados de cirurgias primárias sobre o crescimento maxilofacial e a comparação destes com os dados obtidos por centros de referência para tratamento da FTIU.
Palavras-chave: Fenda labial. Fissura palatina. Desenvolvimento maxilofacial.
Lip and palate reconstruction is essential for the treatment of unilateral cleft lip and palate (UCLP) patients. In combination with a multidisciplinary care program, the objective of this procedure is the functional and aesthetic improvement of the patients' faces1.
Primary reconstructions (cheiloplasties and palatoplasties) in patients with UCLP result in the formation of scar tissue at the surgical site. This causes dynamic and static alterations that, in association with the cleft itself, have negative consequences on maxillary growth and development and thus on the whole maxillofacial complex of the child2-5. According to certain studies, the restriction of maxillary growth does not depend on the genetic predisposition associated with the presence of the cleft, but is rather a consequence of the primary surgical repair6-8. Nevertheless, the ability of the surgeon, the width of the cleft, and the surgical technique have an impact on the results and interfere with the growth and development of the facial structures involved5,9.
Initially, the inhibition of maxillary growth affects the growth and development of the midface and the entire maxillofacial complex, and can later affect dental occlusion, speech, and the shape of the nose. Frequently, these alterations can only be corrected by means of complex procedures such as osteotomies and orthognathic surgeries, which are performed after skeletal maturity is reached5,7,10-12.
The early assessment of maxillomandibular growth disorders through the use of prognostic factors is important because it enables the identification of specific surgical alterations related to maxillofacial growth and facilitates inter-center information exchanges concerning treatment protocols for patients with cleft lip and palate13-17.
Among these prognostic factors, the Atack18 index is used as a growth indicator through the assessment of the relationship between the dental arches (maxilla and mandible) of patients with UCLP during the deciduous teething stages and the beginning of mixed teething, between 4 and 7 years of age. This method enables the preliminary detection of alterations derived from primary surgeries affecting maxillary growth before patients undergo secondary palatoplasty, orthodontic treatment, or alveolar bone grafts13,18-23.
The assessment of deciduous dentition allows the follow-up of maxillomandibular relationships during the development of the patient and can help identify the need for early interventions in young children, which is beneficial for the progress of treatment24-26. The index was adapted for deciduous dentition by Atack18,23 based on Goslon Yardstick's index, which was developed by Mars et al.25 for the evaluation of alterations in the growth of dental arches of young permanent teeth in patients with UCLP in European centers that used different techniques and surgical protocols (The Eurocleft Study)12,16,19,20,22,26.
According to this index, the relationships between maxillary and mandibular dental arches were scored on a scale from 1 to 5. Higher scores reflect an unfavorable prognosis with regard to maxillofacial growth23.
Based on these assumptions, in the present study, the Center for Attention to Facial Defects of Instituto de Medicina Integral Prof. Fernando Figueira (CADEFI) applied this method for the treatment of children with UCLP with deciduous dentition. The main objective was to obtain a preliminary assessment of the outcomes of surgeries performed following the protocol established by the center. In this manner, the results achieved in the center were compared with those of other institutes with experience in the care of cleft patients to determine the best treatment method for patients with cleft lip and palate.
METHODS
A total of 45 patients with unilateral cleft lip and palate were selected between 2001 and 2004. After primary cleft lip and palate surgeries performed during the period from 2006 to 2007, dental casts were obtained and the maxillomandibular relationship was evaluated. Dental casts were assessed according to Atack's classification.
The primary surgery protocol followed in the present study included cheiloplasty at 3 months of age using Millard's technique with a modified Mohler rotation-advancement repair27 with columella elongation and nasal floor reconstruction, avoiding vestibular and nasal base incisions. Palatoplasty was performed starting from 9 months of age in a single surgical procedure, using Von Langenbeck's technique with modifications described by Kriens28 and Braithwaite29 as first choice, and resorting to the technique of Veau in situations in which technical difficulties in the closure of the anterior palate were encountered.
Patients were selected based on the following inclusion criteria: children undergoing primary surgery at CADEFI; the presence of complete deciduous dentition without secondary surgical interventions including upper lip revision, pharyngoplasty, and previous orthodontic treatment with facial mask; the absence of genetic syndromes and diseases associated with inborn errors of metabolism.
A total of 60 UCLP patients were identified from May 2006 to February 2007 through a search of the database of the diagnostic staff of the department. Parents and legal guardians were invited to participate in the study by means of letters, telephone calls, or in person during their visits for routine treatment. A total of 52 children were present for the evaluation, of which 5 did not have complete deciduous dentition and 2 had not undergone primary palatoplasty. The final sample consisted of 45 children with UCLP for a transverse type case selection study.
After parents or legal guardians provided informed consent, forms were distributed for sociodemographic data collection. Each child underwent a session of face (frontal and profile) photographs, with a digital camera for personal identification. Moldings of dental arches were obtained using fast-setting alginate for the generation of study molds in type III stone plaster, with posterior duplication and random numbering for assessing the degree of development of deciduous dentition dental arches based on Atack's index30 (Figure 1).
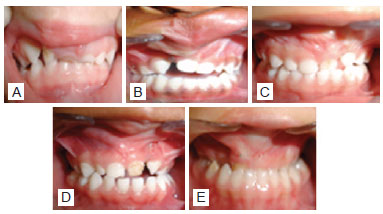
Figure 1 - Representation of categories or scores of the Atack index in deciduous dentition (CADEFI). In A, score 1. In B, score 2. In C, score 3. In D, score 4. In E, score 5.
According to this index classification, scores 1 and 2 represent a good or excellent dental arch relationship and the possibility of reaching a satisfactory maxillomandibular relationship with conventional orthodontic treatment (Figure 1). Score 3 refers to cases that require greater care, including more complex orthodontic treatment compared to the first two situations. Scores 4 and 5 correspond to a more serious discrepancy in the relationship between the maxilla and the mandible, which may indicate future need for osteotomies and orthognathic surgeries for correction23.
The classification of dental arch relationships using the study models was performed by two orthodontists with experience in the treatment of cleft palates. The 45 occlusion models were numbered, randomly distributed for index classification, and classified by both professionals at different times with one week intervals between each assessment.
The assessment of inter- and intra-examiner agreement was performed using the Kappa coefficient. Student's t test and the Marascuillo procedure were used to compare the differences between averages, and values showing P < 0.05 were considered statistically significant. Data were recorded in duplicate using the Epi Info 6.04 software with typing validation and are presented as percentages using measures of central tendency (averages and standard deviation).
The results obtained were compared to those of five studies that were based on primary surgery treatment protocols and evaluated maxillomandibular relationships using a similar method in patients with UCLP (Table 1).
RESULTS
UCLP was more frequent in male patients (76%), and the left side was more frequently affected (62%) than the right. Cheiloplasty was performed at ages between 2 and 12 months, with an average age of 4.7 + 2.7 months using Millard's technique in 100% of the cases. Palatoplasty was performed between the ages of 6 and 24 months (average age of 11.3 + 4.1 months), using the technique of Veau or a modified Von Langenbeck procedure. Evaluation of dental arch relationships was performed in children at an average age of 4 + 0.8 years old. Kappa scores indicated good inter-evaluator agreement (Kappa = 0.66) and excellent intra-evaluator agreement (Kappa = 0.87).
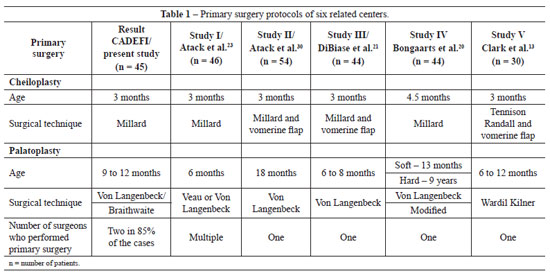
The percentage distribution of the scores of six reference studies that used similar methodology for the evaluation of the results of primary surgeries in patients with UCLP is shown in Table 2. The percentage of patients with a score of 1 or 2, which indicates dental occlusion favoring maxillomandibular growth, was 44.4% (Figure 2); 40% of the children were classified as score 3, which indicates an intermediate situation that may evolve to score 2 or worsen to score 4; 15.6% of the patients had scores of 4 and 5, which indicate an unfavorable condition with respect to maxillomandibular growth (Figure 3).
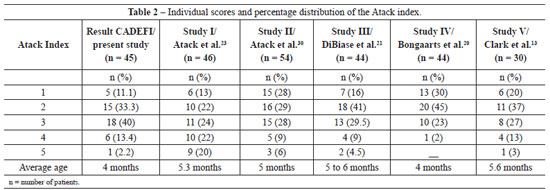

Figure 2 - Representation of the dental arch relationship favorable to maxillomandibular growth (score 2) after primary surgery of the palate. In A, preoperative appearance in a newborn patient with unilateral incisive transforamen cleft. In B, the same patient at 4.5 years of age during the late postoperative period after surgical correction of the palate. In C, dental arch demonstrating inter-arch relationship favorable for maxillofacial growth.

Figure 3 - Representation of a dental arch relationship unfavorable for maxillomandibular growth (score 4) after primary surgery of the palate. In A, preoperative appearance of the patient after primary surgery for unilateral incisive transforamen cleft. In B, the same patient at 4.5 years old during the late postoperative period after surgical correction of the palate. In C, dental arch demonstrating inter-arch relationship unfavorable for maxillofacial growth.
Comparison of the percentages of patients with scores 1 and 2 in the 6 centers revealed that study IV by Bongaarts et al.20 obtained results that were significantly more favorable (P = 0.023) with respect to inter-arch relationships than those of the present study, as evaluated using the Marascuillo test.
DISCUSSION
The anteroposterior development of the maxilla in patients with UCLP has been reported by some authors to be compromised as a consequence of growth disorders caused by primary surgeries8,31.
The Atack index has been applied for the evaluation of different treatment and care protocols and the comparison of results between different centers. This system enabled the monitoring of growth phases and maxillomandibular complex development through longitudinal studies, including the assessment of the results obtained with different surgical techniques9,13,19,20,22,24.
In this institution, the index was used to categorize the growth of dental arches in patients who were 4 years of age, by assessing the degree of maxillary impairment resulting from primary lip and palate surgeries in children with UCLP. Although this method was designed for older children18,23, Clark et al.13 used the same index for the evaluation of dental arches in complete deciduous dentition after primary surgery. In a different study, the same index was applied for the evaluation of patients at 4 and 6 years of age and no statistically significant differences were found between the two results20.
The present study demonstrated the practical use of the index as well as its high reproducibility and capacity for identifying disorders of deciduous dentition in children with UCLP, as confirmed by other authors13,20,22. The present results can be used as a predictive measure of maxillomandibular growth in individuals with UCLP considering the peculiarities of occlusal relationships in deciduous dentition in the assessment of scores32,33. However, the results should be validated in the future with the same children at the young permanent dentition stage32,33.
Facial analysis studies using cephalometric radiographs detected maxillary retrognathism at 5 years of age, which enabled the early diagnosis of maxillary atresia in individuals with UCLP. However, the authors reported difficulties in the identification of maxillary skeleton structures using cephalometric radiographs performed at this age11,15, which makes the method of analysis less invasive and more practical.
In an analysis of the profile of UCLP patients with deciduous dentition and beginning of mixed teething, Gomide et al.34 concluded that although the growth in this age group was satisfactory, the condition worsens with age and causes aesthetically unfavorable modifications, including a straight or concave facial profile during adolescence. Maxillary and mandibular retropositioning, which can be done in cleft patients at the end of the deciduous dentition period (beginning of mixed teething), has resulted in positive inter-maxillary relationships in preliminary assessments26.
In the present study, evaluations were performed by two orthodontists at different times, and good intra and inter-examiner agreement was achieved. This evaluation method was similar to that employed by other studies that used the same index12,13,19,20.
The only difficulties reported in the present study were related to patient recruitment and evaluator calibration, as described previously by other authors19,23,25. To eliminate systematic bias and improve the consistency of the results, all evaluators were trained in the use of the index.
Comparison of the first scores obtained by CADEFI with those of studies found in the literature revealed that each procedure protocol showed specific features aimed at improving the growth results of primary surgeries. This comparison showed that the randomized study with late hard palate closure protocol (closed soft palate at 12/13 months) achieved the best scores20. However, secondary restrictions on maxillary growth after palate closure should be taken into consideration5-9. In addition, studies have shown that organizational changes based on the centralization of primary surgery and the allocation of a greater number of surgeries to a single surgeon can improve the results in terms of maxillomandibular growth13. Although there is at present no single protocol for the treatment of cleft lip and palate patients, multi-center studies conducted by the European Cleft Lip and Palate Research Group (Eurocleft)35 have concluded that factors such as the establishment of an organization center, the centralization of services, number of surgeries performed by a single surgeon, and patient follow-up affect the quality of the results achieved in the treatment of cleft lip and palate patients11,13,19,24,26.
The revision of several treatment protocols based on the analysis of the results of previous studies carried out in different European centers has resulted in obvious improvements in the care of individuals with cleft lip and palate, as shown in subsequent research studies13,20,36, which emphasizes the importance of performing this type of assessment in treatment centers in a systematic and persistent manner.
CONCLUSIONS
The present results show that the Atack index is an important instrument for the preliminary assessment of the effects of primary surgeries on the maxillofacial growth of patients with UCLP, showing ease of use and good reproducibility. The application of this method enabled the comparison of results between different treatment centers, taking into consideration the surgical protocols adopted by each institution, in particular in reference to the phase and timing of palate closure. However, longitudinal studies are essential to monitor craniofacial growth and assess the stability of the results obtained after primary surgeries.
REFERENCES
1. Kuijpers-Jagtman AM, Long Jr. RE. The influence of surgery and orthopedic treatment on maxillofacial growth and maxillary arch development in patients treated for orofacial clefts. Cleft Palate Craniofac J. 2000;37(6):527.
2. Stein S, Dunsche A, Gellrich NC, Härle F, Jonas I. One- or two-stage palate closure in patients with unilateral cleft lip and palate: comparing cephalometric and occlusal outcomes. Cleft Palate Craniofac J. 2007; 44(1):13-22.
3. Friede H. Maxillary growth controversies after two-stage palatal repair with delayed hard palate closure in unilateral cleft lip and palate patients: perspectives from literature and personal experience. Cleft Palate Craniofac J. 2007;44(2):129-36.
4. Rohrich RJ, Love EJ, Byrd HS, Johns DF. Optimal timing of cleft palate closure. Plast Reconstr Surg. 2000;106(2):413-21.
5. Ross RB. Treatment variables affecting facial growth in complete unilateral cleft lip and palate. Part 1: Treatment affecting growth. Cleft Palate Craniofac J. 1987;24(1):5-23.
6. Shetye PR, Evans CA. Midfacial morphology in adult unoperated complete unilateral cleft lip and palate patients. Angle Orthod. 2006;76(5):810-6.
7. Capelozza Filho L, Normando AD, da Silva Filho OG. Isolated influence of lip and palate surgery on facial growth: comparison of operated and unoperated male adults with UCLP. Cleft Palate Craniofac J. 1996;33(1):51-6.
8. Mars M, Houston WJ. A preliminary study of facial growth and morphology in unoperated male unilateral cleft lip and palate subjects over 13 years of age. Cleft Palate J. 1990;27(1):7-10.
9. Shaw WC, Asher-McDade C, Brattström V, Dahl E, McWilliam J, Mølsted K, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: Part 1. Principles and study design. Cleft Palate Craniofac J. 1992;29(5):393-7.
10. Semb G, Brattström V, Mølsted K, Prahl-Andersen B, Shaw WC. The Eurocleft study: intercenter study of treatment outcome in patients with complete cleft lip and palate. Part 1: introduction and treatment experience. Cleft Palate Craniof J. 2005;42(1):64-8.
11. Mølsted K, Asher-McDade C, Brattström V, Dahl E, Mars M, McWilliam J, et. al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: Part 2. Craniofacial form and soft tissue profile. Cleft Palate Craniofac J. 1992;29(5):398-404.
12. Mars M, Asher-McDade C, Brattström V, Dahl E, McWilliam J, Mølsted K, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate. Part 3. Dental arch relationships. Cleft Palate Craniofac J. 1992;29(5):405-8.
13. Clark SA, Atack NE, Ewings P, Hathorn IS, Mercer NS. Early surgical outcomes in 5-year-old patients with repaired unilateral cleft lip and palate. Cleft Palate Craniofac J. 2007;44(3):235-8.
14. Williams AC, Bearn D, Mildinhall S, Murphy T, Sell D, Shaw WC, et al. Cleft lip and palate care in the United Kingdom: the Clinical Standards Advisory Group (CSAG) study. Part 2: dentofacial outcomes and patient satisfaction. Cleft Palate Craniofac J. 2001;38(1):24-9.
15. Mackay F, Bottomley J, Semb G, Roberts C. Dentofacial form in the five-year-old child with unilateral cleft lip and palate. Cleft Palate Craniofac J. 1994;31(5):372-5.
16. Shaw WC, Dahl E, Asher-McDade C, Brattström V, Mars M, McWilliam J, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: Part 5. General discussion and conclusions. Cleft Palate Craniofac J. 1992;29(5):413-8.
17. Roberts CT, Semb G, Shaw WC. Strategies for the advancement of surgical methods in cleft lip and palate. Cleft Palate Craniofac J. 1991;28(2):141-9.
18. Atack NE, Hathorn IS, Semb G, Dowell T, Sandy JR. A new index for assessing surgical outcome in unilateral cleft lip and palate subjects aged five: reproducibility and validity. Cleft Palate Craniofac J. 1997;34(3):242-6.
19. Hathorn IS, Atack NE, Butcher G, Dickson J, Durning P, Hammond M, et al. Centralization of services: standard setting and outcomes. Cleft Palate Craniofac J. 2006;43(4):401-5.
20. Bongaarts CA, Kuijpers-Jagtman AM, van't Hof MA, Prahl-Andersen B. The effect of infant orthopedics on the occlusion of the deciduous dentition in children with complete unilateral cleft lip and palate (Dutchcleft). Cleft Palate Craniofac J. 2004;41(6):633-41.
21. DiBiase AT, DiBiase DD, Hay NJ, Sommerlad BC. The relationship between arch dimensions and the 5-year index in the primary dentition of patients with complete UCLP. Cleft Palate Craniofac J. 2002;39(6):635-40.
22. Sandy JR, Williams AC, Bearn D, Mildinhall S, Murphy T, Sell D, et al. Cleft lip and palate care in the United Kingdom--the Clinical Standards Advisory Group (CSAG) Study. Part 1: background and methodology. Cleft Palate Craniofac J. 2001;38(1):20-3.
23. Atack N, Hathorn I, Mars M, Sandy J. Study models of 5 year old children as predictors of surgical outcome in unilateral cleft lip and palate. Eur J Orthod. 1997;19(2):165-70.
24. Sandy J, Williams A, Mildinhall S, Murphy T, Bearn D, Shaw B, et al. The Clinical Standards Advisory Group (CSAG) Cleft Lip and Palate Study. Br J Orthod. 1998;25(1):21-30.
25. Mars M, Plint DA, Houston WJ, Bergland O, Semb G. The Goslon Yardstick: a new system of assessing dental arch relationships in children with unilateral clefts of the lip and palate. Cleft Palate Craniofac J. 1987;24(4):314-22.
26. Shaw WC, Dahl E, Asher-McDade C, Brattström V, Mars M, McWilliam J, et al. A six-center international study of treatment outcome in patients with clefts of the lip and palate: Part 5. General discussion and conclusions. Cleft Palate Craniofac J. 1992;29(5):413-8.
27. Mohler LR. Unilateral cleft lip repair. Plast Reconstr Surg. 1987;80(4):511-7.
28. Kriens OB. Fundamental anatomic findings for an intravelar veloplasty. Cleft Palate J. 1970;7:27-36.
29. Braithwaite F. Congenital deformities. II. Cleft palate repair. Mod Trends Plast Surg. 1964;16:30-49.
30. Atack NE, Hathorn I, Dowell T, Sandy J, Semb G, Leach A. Early detection of differences in surgical outcome for cleft lip and palate. Br J Orthod.1998;25(3):181-5.
31. Wada T, Mizokawa N, Miyazaki T, Ergen G. Maxillary dental arch growth in different types of cleft. Cleft Palate Craniofac J. 1984;21(3):180-92.
32. Garrahy A, Millett DT, Ayuob AF. Early assessment of dental arch development in repaired unilateral cleft lip and unilateral cleft lip and palate versus controls. Cleft Palate Craniofac J. 2005;42(4):385-91.
33. Mars M, Batra P, Worrell E. Complete unilateral cleft lip and palate: validity of the five-year index and the Goslon yardstick in predicting long-term dental arch relationships. Cleft Palate Craniofac J. 2006;43(5):557-62.
34. Gomide MR, Capelozza Filho L, Tovo AHS, Abdo RCC. Relações maxilomandibulares de portadores de fissura transforame incisivo unilateral na dentadura mista. Rev Odontol Univ São Paulo. 1998;12(4):337-42.
35. Shaw WC, Semb G, Nelson P, Brattström V, Molsted K, Prahl-Andersen B, et al. The Eurocleft project 1996-2000: overview. J Craniomaxillofac Surg. 2001;29(3):131-40.
36. Prahl-Andersen B, Ju Q. Quality improvement of cleft lip and palate treatment. Angle Orthod. 2006;76(2):265-8.
1. Head of the Plastic Surgery Department of Instituto de Medicina Integral Prof. Fernando Figueira (IMIP), Recife, PE, Brazil.
2. Master in Maternal and Child Health, pediatric dentist and maxillary functional orthopedist of the Centro de Atenção aos Defeitos da Face (CADEFI) of IMIP, Recife, PE, Brazil.
3. Doctor in Pediatrics, professor of the Maternal and Child Department and of the Post-Graduate Course of Child and Adolescent Health of Universidade Federal de Pernambuco, Recife, PE, Brazil.
4. Doctor in Dentistry, head of the Dentistry Center of CADEFI - IMIP, Recife, PE, Brazil.
5. Doctor in Dentistry, orthodontist at CADEFI - IMIP, Recife, PE, Brazil.
6. Associate professor of the School of Medicine of Universidade de São Paulo, São Paulo, Brazil.
Correspondence to:
Rui Manuel Rodrigues Pereira
Rua dos Coelhos, 300 - Boa Vista
Recife, PE, Brazil - CEP 50070-550
E-mail: ruipereira@realplastica.med.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: July 9, 2011
Paper accepted: October 25, 2011
Study conducted at Instituto de Medicina Integral Prof. Fernando Figueira (IMIP), Recife, PE, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter