

Original Article - Year 2011 - Volume 26 -
Correction of prominent ears by the cartilaginous incision technique, definition of the antihelix with Mustardé sutures, and fixation of the ear cartilage at the mastoid
Correção da orelha de abano pela técnica de incisão cartilaginosa, definição da antélice com pontos de Mustardé e fixação da cartilagem conchal na mastoide
ABSTRACT
BACKGROUND: Prominent ear is the most common congenital defect of the ear, with an incidence of 5% in Caucasians. Surgical treatment should correct the auriculocephalic and conchoscaphal angles as well as protrusion of the lobe when present. This paper aims to report the experience of our service in the treatment of prominent ears with a combination of several available techniques.
METHODS: Forty-seven patients operated with a combination of previously described techniques were evaluated, and cartilaginous incision, Mustardé sutures for antihelix definition, and concha-mastoid fixation were performed. Patients less than 15 years of age were operated under general and local anesthesia, while the remaining patients underwent only local anesthesia. All patients were reassessed on the first postoperative day.
RESULTS: The postoperative results were considered satisfactory by both patients and surgical staff, with no stigma development in the operated ear.
CONCLUSIONS: The best treatment of prominent ears is achieved by a combination of techniques. The approach used on the studied patients has produced natural-looking results with low complication rates, satisfying the surgical staff and, most importantly, the patients.
Keywords: External ear/surgery. Plastic surgery/methods. Ear diseases/surgery.
RESUMO
INTRODUÇÃO: A orelha de abano é o mais comum de todos os defeitos congênitos da orelha, com incidência de 5% em caucasianos. O tratamento cirúrgico deve corrigir os ângulos auriculocefálico e escafoconchal, bem como a protrusão do lóbulo, quando presente. O objetivo deste trabalho é demonstrar a experiência de nosso serviço no tratamento da orelha de abano com a combinação de diversas técnicas disponíveis.
MÉTODO: Foram avaliados 47 pacientes, operados com a associação de técnicas já descritas anteriormente, sendo utilizados incisão cartilaginosa, pontos de Mustardé para definição de antélice e fixação da concha na mastoide. Os pacientes com menos de 15 anos de idade foram operados sob anestesias geral e local, e os demais foram submetidos somente a anestesia local. Todos os pacientes foram reavaliados no primeiro dia de pós-operatório.
RESULTADOS: Os resultados pós-operatórios foram considerados satisfatórios pelos pacientes e pela equipe cirúrgica, sem o aparecimento do estigma de orelha operada.
CONCLUSÕES: O melhor tratamento de orelhas proeminentes é obtido com a associação de diversas técnicas. A abordagem empregada nos pacientes avaliados tem apresentado resultados naturais e com baixos índices de complicação, satisfazendo a equipe cirúrgica e, principalmente, os pacientes.
Palavras-chave: Orelha externa/cirurgia. Cirurgia plástica/métodos. Otopatias/cirurgia.
Prominent ear is the most common congenital ear defect. The deformity can be noticed upon birth and generally becomes more pronounced with the passage of time1, with an incidence of 5% in Caucasians2. Although they do cause functional changes, ear deformities may also cause clinically relevant psychosocial disorders3.
For the correction of prominent ears, the anatomical changes must first be correctly diagnosed. The 3 most common causes of prominent ears, which may be present separately or in association, are underdeveloped antihelix, increased conchoscaphal angle, conchal prominence, increased auriculocephalic angle, and lobe protrusion3.
The normal auriculocephalic angle ranges between 25 and 30 degrees; when greater than 40 degrees, it can be considered abnormal. Similarly, the normal conchoscaphal angle is approximately 90 degrees, and more obtuse angles frequently require surgical correction4,5. In addition to those with anatomical alterations in the pavilion itself, patients with significantly asymmetrical ears may also benefit from otoplasty6.
This paper aims to demonstrate the experience of our service in the treatment of prominent ears with a combination of several available techniques.
METHODS
Forty-seven patients, 2 of whom were unilateral cases, were assessed and operated by a combination of techniques described below.
The surgeries were performed between February 2009 and December 2010 by the Plastic Surgery Service of Hospital Federal da Lagoa (Rio de Janeiro, RJ, Brazil).
The operated patients were between 7 and 52 years of age (average of 23 years old) and included 18 females and 29 males.
Patients less than 15 years of age (25.5% of the cases) were operated under general and local anesthesia; the remaining patients (74.5% of the cases) underwent local anesthesia only.
Patients operated under general anesthesia were discharged on the day following the procedure, and those who underwent local anesthesia were discharged that same day. All patients were reassessed on the first postoperative day.
Surgical Technique
1. Marking of the anterior and posterior surfaces of the ear with a demographic pen. The anterior markings refer to the areas for cartilaginous incision and the posterior markings to the resection of the skin island (Figures 1 and 2).

Figure 1 - Anterior marking.

Figure 2 - Posterior marking.
2. Infiltration of 2% lidocaine solution + epinephrine in 1% saline to give a 1:200,000 epinephrine solution, not exceeding 10 mg/kg of local anesthetic.
3. Incision and resection of the posterior skin island according to the previous markings, so that the resulting scar is positioned in the retroauricular crease (Figure 3).

Figure 3 - Resected skin island.
4. Posterior detachment of the ear in the subperichondrial plane until the auricular cartilage is well-exposed and detachment of the mastoid region with resection of the posterior auricular muscle (Figure 4).

Figure 4 - Detachment of the posterior region of the ear and mastoid region.
5. Marking of the cartilaginous incisions by introducing insulin needles according to the previous markings on the anterior surface of the ear.
6. Incision of the cartilage at 4 points: at the external edge of the antihelix, a transverse incision between both, avoiding the first 2 incisions to be joined and, finally, an incision at the external edge of the concha (Figure 5).

Figure 5 - Incisions in the auricular cartilage.
7. Definition of the antihelix with Mustardé sutures using 4.0 nylon suture between the existing incisions. The first suture is placed between the incision at the outer edge of the antihelix and the incision at the inner edge of the upper branch of the antihelix, and 1 or 2 additional sutures are placed between the incision at the outer edge of the antihelix and the incision at the concha to complete the definition of the antihelix (Figures 6 to 8).
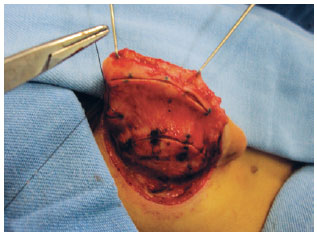
Figure 6 - Mustardé suture.
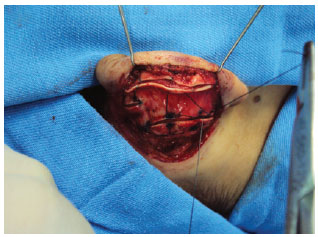
Figure 7 - Mustardé suture.
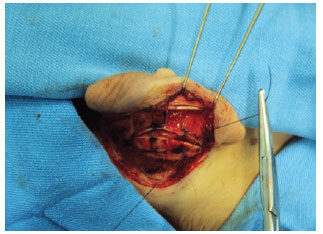
Figure 8 - Mustardé suture.
8. Resection of excess conchal cartilage, when necessary (Figure 9).
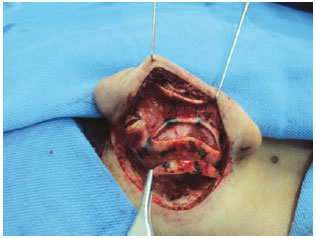
Figure 9 - Resection of excess conchal cartilage.
9. Rotation of the conchal cartilage and its fixation at the mastoid with 3.0 nylon suture (Figure 10). When required, the upper and lower poles of the ear can be fastened at the mastoid region using 4.0 nylon suture.

Figure 10 - Fixation of the concha at the mastoid.
10. Skin closure with the Greek suture technique using 4.0 nylon suture (Figure 11).

Figure 11 - Final closure of the skin.
11. Dressing with damp cotton filling all concavities of the ear, padding with gauze, and placement of crepe bandages, which should remain undisturbed for 24 hours; thereafter, the patient is assessed on the first postoperative day.
Postoperative Follow-up
On the first postoperative day, the surgical dressing was replaced by an elastic bandage for auricular protection; this was maintained for 45 days and was used only at night for the last 15 days.
Antibiotic therapy was maintained for 7 days, and analgesics and non-steroidal anti-inflammatory drugs were prescribed as required.
Outpatient postoperative follow-up consultations were held 1 day, 1 week, 21 days, 45 days, 3 months, and 6 months after the procedure. The sutures were removed at the consultation on the 21st postoperative day.
RESULTS
A total of 47 patients underwent correction of prominent ears by a combination of the techniques presented in this study. The techniques used were cartilaginous incision, Mustardé sutures for antihelix definition, conchal rotation, and, when required, resection of excess conchal cartilage.
The postoperative results were considered satisfactory by both the patients and the surgical staff, with no development of stigma in the operated ear.
Figures 12 to 15 illustrate the results obtained with the described techniques in patients operated by our service.

Figure 12 - A, immediate preoperative period; B, immediate postoperative period.
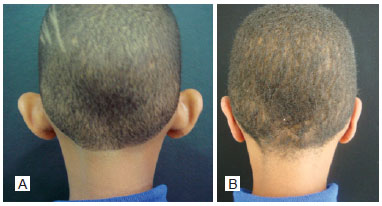
Figure 13 - Patient 1. A, preoperative period, posterior view; B, postoperative period, posterior view.

Figure 14 - Patient 2. A, preoperative image, anterior view; B, postoperative image, anterior view.
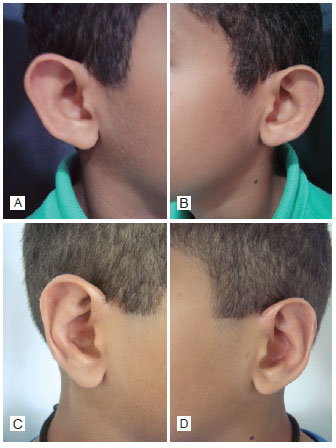
Figure 15 - Patient 3. A, preoperative image, right profile; B, preoperative image, left profile; C, postoperative image, right profile; D, postoperative image, left profile.
DISCUSSION
A surgical procedure for correction of prominent ears was first described in 1845 by Dieffenbach, who suggested a retroauricular skin resection. Since then, several authors have developed and proposed new surgical techniques, always aiming at more natural-looking and long-lasting results7.
A prominent ear is determined by one or more anatomical changes, requiring that the deformities of each part of the ear be considered separately during surgical planning so that treatment of the individual deformities will produce a harmonious and natural result. The ideal result is ears that do not appear to have undergone surgery8.
The cartilaginous incision provides a suitable break of the cartilaginous spring in patients with either thick or thin cartilages, achieving harmonious results without any cartilage break.
For definition of the antihelix, 2 to 4 Mustardé sutures are used, as needed in each case, avoiding excessive tightening of the sutures so as not to cause aesthetic impairment.
Conchal rotation with fixation at the periosteum of the mastoid region was employed in all patients in this study, with care to avoid clinically relevant closure of the external auditory canal9. In some patients with greater hypertrophy, we also performed resection of excess concha.
Complications of otoplasties are very rare9,10. The most common complications are hematoma and immediate postoperative infection1. In the late postoperative period, there may be extrusion of sutures and/or more significant complications such as hypercorrection or contour irregularities3. We observed 1 case of suture extrusion and 2 cases of unilateral hematoma in our selected cases; the latter were promptly resolved by drainage. There was no case of infection.
CONCLUSIONS
The best treatment of prominent ears is achieved by a combination of various techniques. The approach used on the studied patients produces natural-looking results with low complication rates, satisfying the surgical staff and, most importantly, the patients.
REFERENCES
1. Avelar MA. In: Mélega JM, ed. Cirurgia estética. Rio de Janeiro: Guanabara Koogan; 2003. p.271-80.
2. Bardach J. Surgery for congenital and acquired malformations of the auricle. In: Cummings CW, Fredrickson JM, Harker LA, Krause CJ, Schüller DE, eds. Otolaryngology: head and neck surgery. St Louis: Mosby; 1986. p.2861.
3. Thorne CH, Beasley RW, Aston SJ, Bartlett SP, Gurtner GC, Spear SL, eds. Grabb & Smith: Cirurgia Plástica. 6ª ed. Rio de Janeiro: Guanabara Koogan; 2009. p.290-304.
4. Skiles MS, Randall P. The anesthetics of ear placement: an experimental study. Plast Reconstr Surg. 1983;72(2):133-40.
5. Aygit AC. Molding the ears after anterior scoring and concha repositioning: a combined approach for protruding ear correction. Aesthetic Plast Surg. 2003;27(1):77-81.
6. Georgiade GS, Riefkohl R, Georgiade NG. Prominent ears and their correction: a forty-year experience. Aesthetic Plast Surg. 1995;19(5):439-43.
7. Calder JC, Naasan A. Morbidity of otoplasty: a review of 562 consecutive cases. Br J Plast Surg. 1994;47(3):170-4.
8. Ferreira LM. Deformidades auriculares. In: Manual de Cirurgia Plástica. São Paulo: Atheneu; 1995. p.223-8.
9. Spira M. Otoplasty: what I do now. A 30-year perspective. Plast Reconstr Surg. 1999;104(3):834-40.
10. Franco T, Rebello C. Otoplastias. In: Franco T, Rebello C, eds. Cirurgia estética. Rio de Janeiro: Atheneu; 1977. p.181-201.
1. Resident physician in Plastic Surgery at Hospital Federal da Lagoa, Rio de Janeiro, RJ, Brazil.
2. Specialist member of the Brazilian Society of Plastic Surgery (SBCP), former resident physician in Plastic Surgery at Hospital Federal da Lagoa, Rio de Janeiro, RJ, Brazil.
3. Full member of SBCP and of the Brazilian Association of Surgeons, head of the Plastic Surgery Service of Hospital Federal da Lagoa, Rio de Janeiro, RJ, Brazil.
Correspondence to:
Francisco de Oliveira Goulart
Rua Cinco de Julho, 349/906 - Copacabana
Rio de Janeiro, RJ, Brazil - CEP: 22051-030
E-mail: franciscooliveiragoulart@yahoo.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Paper received: June 16, 2011
Paper accepted: October 10, 2011
Study conducted at Hospital Federal da Lagoa - Federal Network of Healthcare at Rio de Janeiro, Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter