

Original Article - Year 2011 - Volume 26 -
Inclusion of calf implants for the correction of lower limb amyotrophy
Inclusão de implantes de panturrilha na correção das amiotrofias dos membros inferiores
ABSTRACT
Background: Lower limb amyotrophy is a serious deformity that is often disabling and causes esthetic problems such as asymmetries and changes in the shape and contour of the legs. The present study evaluated the use of silicone implants for the correction of lower limb amyotrophy. Methods: Women who underwent surgical correction of lower limb amyotrophy with silicone implants between 2002 and 2009 at the Plastic Surgery Service of Instituto Ivo Pitanguy at the 38th Nursing Service of Santa Casa da Misericórdia, Rio de Janeiro and at their associated services were retrospectively reviewed. Results: Five cases were studied and the results were retrospectively assessed. Follow-up ranged from 3 months to 2 years after surgery until the last postoperative visit. In 4 of 5 patients, the desired result was obtained after a single surgical procedure, and no patient developed capsular contracture, compartment syndrome, circulatory disorders, neurological disorders, or infections. Conclusions: Calf augmentation in patients with lower limb amyotrophy did not correct the associated functional deficit, but resulted in a high level of satisfaction with regard to the esthetic improvement of the limb, thus improving the quality of life of these patients.
Keywords: Muscular atrophy. Leg/surgery. Prostheses and implants. Silicone gels.
RESUMO
Introdução: As amiotrofias dos membros inferiores são deformidades por vezes incapacitantes, mas que trazem aos pacientes problemas estéticos, como assimetrias e alterações da forma e contorno das pernas. Este estudo teve como objetivo avaliar a aplicabilidade do uso de implantes de silicone para correção de amiotrofias de membros inferiores. Métodos: Estudo retrospectivo de pacientes, todas do sexo feminino, submetidas a correção cirúrgica de amiotrofia de pernas com a utilização de implantes de silicone, entre 2002 e 2009, no Serviço de Cirurgia Plástica do Instituto Ivo Pitanguy, na 38ª Enfermaria da Santa Casa da Misericórdia do Rio de Janeiro e em serviços associados. Resultados: Foram analisados 5 casos. A maioria dos resultados foi avaliada de maneira retrospectiva. O tempo de acompanhamento variou de 3 meses a 2 anos, desde a cirurgia até a última consulta pós-operatória. Do total de pacientes, 4 apresentaram resultado desejado em apenas um procedimento cirúrgico e nenhuma paciente apresentou contratura capsular, síndrome compartimental, alterações circulatórias, alterações neurológicas ou infecção. Conclusões: O aumento das panturrilhas em pacientes portadoras de amiotrofias de membros inferiores não proporcionou modificações no tocante ao déficit funcional prévio. Todavia, essas pacientes, geralmente bastante castigadas pela doença de base, apresentam índice de satisfação muito elevado com a melhoria estética do membro, otimizando, dessa forma, a qualidade de vida dessas pacientes.
Palavras-chave: Atrofia muscular. Pernas/cirurgia. Próteses e implantes. Géis de silicone.
Lower limb amyotrophy refers to a series of leg deformities associated with a variety of problems including a thin, bent, asymmetric calf in relation to the opposite leg1. The complications associated with lower limb amyotrophy force patients to seek surgical correction of this problem, which is difficult to conceal.
The possible causes of amyotrophy include polio, post-traumatic sequelae, orthopedic surgery sequelae, clubfoot (varus equine), ablation or tumor treatment by radiation therapy, post-traumatic palsy (lesions in the sciatic nerve or its subdivisions), congenital muscular hypoplasia, sequelae of cerebral palsy and spina bifida, and burn contracture2.
Even though correction of these deformities does not lead to recovery of the function of the affected limb, most patients prefer to correct esthetic deficiency so that the affected leg can appear similar to the normal leg.
Muscle transplant surgery for the correction of this condition is not often possible and is associated with large scars. Omentum transplants or dermal adipose fragments with vascular anastomosis require major interventions and have little predictability in the long-term postoperative period, and they are associated with scars in the removal areas. The technical aspects inherent to muscle transplant surgery make bone augmentation impossible in most cases3. In this context, the use of silicone implants for the correction of lower limb amyotrophy has been gaining popularity and is being considered by many surgeons as the most suitable procedure to replace calf muscle volume and shape.
Few publications in the specialized literature describe the results of correction of lower limb amyotrophy; this may be because the issues associated with this type of corrective surgery are not so common yet. Therefore, studies on a large number of patients2 have not been performed and references regarding methods for correction are few in the literature.
The aim of the present study was to provide comprehensive information on calf implant surgery options via a review of lower limb amyotrophy correction surgeries performed at the Plastic Surgery Service of Instituto Ivo Pitanguy at the 38th Nursing Service of Santa Casa da Misericórdia, Rio de Janeiro, Brazil, and at their associated services during the past 7 years.
Surgical Anatomy of the Legs
The unique anatomical features of the legs determine the particular nature of leg surgery. The normal leg has a single fat layer with dense fibrous septa in its inner structure and a rich lymphatic meshwork1, which contribute to irregularities5 and prolonged edema as a consequence of liposuction in this region. Because the subcutaneous layer is thin, even a slight hematoma or bruising may result in hyper pigmentation that does not resolve for a long time6. Moreover, the effect of gravity exacerbates the edema, which together with the rich lymphatic meshwork and deficient drainage in the region, results in a tendency to form fibrous tissue during the postoperative period; this may progress to intense subcutaneous hardening comparable to wood6.
However, the safe insertion of implants in this anatomical area is not complicated. The medial sural cutaneous nerve is located medially between the gastrocnemius muscles, following the small saphenous vein. The lateral sural cutaneous nerve crosses the lateral head of the gastrocnemius and descends along the lateral part of the muscle. The soleus muscle is located in the deeper portion of the posterior leg, while the gastrocnemius muscles are located superficially. Frequently, the lower edge of the medial gastrocnemius is placed caudally in relation to the lateral gastrocnemius, which should be considered during implant insertion.
The muscles in the region are covered by a thin layer called the epimysium. The ideal dissection plane is located between the fascia (which covers the muscles of the posterior compartment of the leg) and the epimysium, which is a mostly non-vascular area. Glicenstein3 reported the presence of two fascial layers in some patients, in which case the implants should be inserted below the deepest fascia.
Calf implant surgery is not commonly performed in the popliteal fossa below the fascia, and its anatomy will therefore not be described here, as it is beyond the scope of this study.
Aesthetic Aspects of the Legs
The aesthetic ideals of the body and ideal proportions were first established by the ancient Egyptians and were applied in Greek and Renaissance art and architecture. In 1202, the Italian mathematician Filius Bonacci (known as Leonardo de Pisa) studied the mathematical proportions of the body and established a 1 to 1.618 ratio, which was named the golden ratio, and later the "divine ratio" by the mathematician Johannes Kepler7.
Howard8 described the ideal length of the legs and calves, based on Leonardo da Vinci's studies, and determined that 1.618 was the ideal length of the gastrocnemius and 1 was the distance between the ankle and the inferomedial aspect of the muscle and knee, and the super-medial aspect of the muscle (Figure 1).
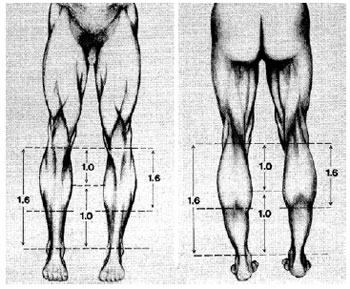
Figure 1 - The divine ratio applied to the aesthetics of the legs (Image from Howard8).
Slazay6 recorded several measurements and determined that a calf circumference between 33 and 36 cm would make female calves more attractive, and a larger or smaller circumference would not be aesthetically acceptable.
In 1997, Martín9 introduced the anatomical conceptualization of the legs and ankles as a rhomboid, whose points would be the front edge of the tibia, the Achilles tendon, and the two malleoli. In this model, fat would tend to accumulate between the lines linking these points, which would conceal these prominences. Thus, fat accumulation may result in a blunt definition of the lower edge of the gastrocnemius muscle, especially in its medial aspect1,2. The medial region between the gastrocnemius and the lower part of the leg is obscured by fat, and may result in an undesirable columnar appearance of the leg.
According to Martín9, "beauty is based on the difference of a region in relation to another. the correction of a simple area may lead to disharmony of the region." Thus, some authors argue that an isolated inspection is not sufficient to accurately assess the region, and examination of the leg component responsible for the disharmony is necessary prior to surgical intervention.
METHODS
The cases of 5 women who underwent correction of leg deformities with silicone implant surgery between September 2002 and September 2009 were retrospectively reviewed.
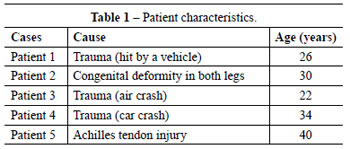
The patients were between 22 and 40 years of age and had impaired function of the lower limb, although they were able to move about without the aid of crutches or a wheelchair. Three patients had post-traumatic deformities, 1 had a clubfoot deformity (varus equine), and the other had post-traumatic muscle atrophy in the Achilles tendon (Table 1).
Four patients were operated at the 38th Nursing Service of Santa Casa de Misericórdia, and 1 was operated at a service associated with Instituto Ivo Pitanguy.
Patient Preparation
Preoperatively, patients were photographed while standing on a podium or platform to provide the photographer with a direct perspective from which to capture the image of the calves, thus preventing distortion and facilitating postoperative comparisons. The patients were instructed to keep their legs slightly apart and their legs were photographed from the front, the back, the back along with the toes, and the sides.
Surgical marking was performed with the patient in a standing position and by defining the lower edges of the gastrocnemius muscles and the midline. The incision line and dissection limits for the cavities of the implants were marked on the skin. The distal end was drawn to extend from 3 to 4 cm below the implant, in accordance with a maximum distance of 5 to 7 cm above the medial or lateral malleolus, and thereby create a smooth transition from the thinnest part of the leg 2, located right above the ankles.
Because the present cases were related to reconstructive surgery and each defect was different, the assessment parameters included the size of the defect; precise parts impaired; needs of the patients; and quality of skin, muscle, fat, and bone in relation to the contralateral limb. The implants were selected on the basis of this information, the measurements obtained in each case, and the experience and esthetic judgment (sensibilitus) of the surgeon. In cases of correction in 1 leg, the contralateral leg was used as a reference. The main objective of this type of surgery is to achieve a contour of the calf resembling a normal leg, and this aim is different from those of other calf augmentation surgeries such as those preferred by bodybuilders and patients seeking to increase the volume of the calf region.
In patients with amyotrophy and post-traumatic deformity of the lower limbs, leg asymmetry is even more apparent because of compensatory hypertrophy in the unaffected side. In these cases, in addition to the placement of implants in the affected side, liposuction can be performed on the normal side to improve symmetry, and this procedure should be part of the preoperative planning. However, in the cases selected herein, liposuction in the calf region was not performed.
Surgical Technique
Patients were operated under low epidural anesthesia associated with sedation, although the procedure can also be performed under spinal anesthesia. Local infiltration of a solution containing anesthetic or vasoconstrictor substances was not performed. A variation of the dry technique was chosen, with the aid of Esmarch bandages from the toes to the thigh for exsanguination of the limb to be operated9,10 (Figure 2).

Figure 2 - Detail of the limb (patient 5) with proximal compression after applying an Esmarch bandage.
The patient was positioned in the surgical bed in the prone position after the administration of anesthesia, and antisepsis was performed. In regions devoid of scars, an incision was made in the area previously marked, corresponding to the lowest natural popliteal sulcus. The most common incision in these cases is a cross-section 4 to 5-cm long in the most central area of the popliteal fossa, as the most common correction is in the medial portion of the region.
A skin incision was made and extended into the subcutaneous tissue, and dissection was performed in the caudal direction. Ideally, an incision in the fascia at 3 cm caudal to the skin incision should be made if the intention is to have a subfascial insertion. In subcutaneous implants, the dissection is made in the subcutaneous plane, resulting in a visible implant. In the subfascial plane, the cavity is prepared by blunt dissection between the fascia and the thin layer of epimysium covering the gastrocnemius muscle. This dissection can be aided by blunt, fingertip, heart-shaped, or duckbill retractors or other similar instruments. In cases in which lateral and medial cavities are prepared for the placement of 2 implants, the preservation of a fascial connection between the cavities is recommended, ensuring that the implants are not joined and that the medial sural cutaneous nerve and the small saphenous vein are not compromised.

Figure 3 - Patient 5. Before (left pictures) and 3 months after (right pictures) silicone implant insertion, 120 ml medially located and only in the left leg.

Figure 4 - Patient 4. Detail of implant herniation in the postoperative period.

Figure 5 - Patient 4. Before and after silicone implant insertion (120 ml), showing the medial gastrocnemius of the left leg.
Most implants have a small Silastic pouch on the posterior surface to support their introduction, which is achieved with the help of an instrument equipped with a flat surface that is in contact with the implant and an end that is attached to the implant pouch. However, many surgeons use a common liposuction cannula for this surgical procedure. The incision is closed in layers.
Auxiliary procedures were not performed, such as liposuction of the contralateral leg or fat grafting in the affected leg.
Postoperative Aspects
The patients remained on bed rest for 12 hours. They were discharged the day after the procedure, and a week of relative rest was prescribed. The patients were instructed to walk in the first 15 days with crutches if necessary.
The surgical wound was occluded with Steri-Strip skin closures (3M do Brazil), and the sutures were removed after 3 weeks.
RESULTS
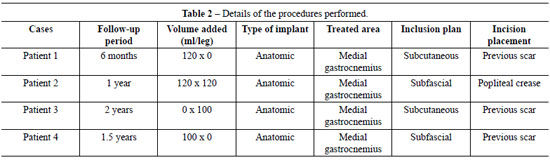
The present results were obtained via a retrospective assessment of patient data. Follow-up periods ranged from 3 months to 2 years after surgery until the last postoperative visit. The study included 5 women who underwent calf implant surgery for augmentation of the medial gastrocnemius. Four patients obtained the desired result after a single surgical procedure. Four patients received 1 implant and 1 received implants in both legs. The volume and type of implant as well as other technical details of the procedures performed are presented in Table 2.
The type of incision depended on the reason for implant surgery: in 2 (40%) patients without scarring, the popliteal crease was used; in the remaining patients, who had prior scars from trauma, the existing scar was used for the incision and insertion of the implant. Scar hypertrophy was observed in the 2 patients in whom the popliteal crease was used. No patient developed compartment syndrome or capsular contracture; however, 1 patient suffered herniation of the implant in the cavity, requiring surgery after 1 month to reposition the implant. No circulatory or neurological changes, infections, or other complications were observed.
DISCUSSION
In addition to the scarcity of the literature on amyotrophy correction, the existing studies on implant surgery describe the treatment of patients with polio sequelae. Case selection in the present study is therefore different as it includes patients with previous scars and fibrosis in the region to be operated.
The subcutaneous plane was used for the insertion of the implant in 3 patients because in them, the subfascial plane could not be accessed owing to prior trauma, which had caused changes in the fascial plane, and different degrees of muscle injury. Glicenstein3 advocated the insertion of implants in direct contact with the atrophied muscle in patients with amyotrophy, as subcutaneous placement could be associated with complications such as skin damage and a visible and palpable implant7,8,11,12.
Medial belly of gastrocnemius atrophy correction is the most common procedure, and was performed in 100% of the present cases. One patient in the present study required a second surgical procedure for the insertion of an implant for correction of the lateral belly of gastrocnemius. In this case, a 2-stage surgery was performed, as the patient did not have adequate skin coverage to receive both implants simultaneously.
With respect to the anesthetics used in this study, all patients received regional anesthesia associated with sedation, and a dry technique, to avoid infiltrating any solution in the cavity to be dissected, was used. An Esmarch bandage was used for exsanguination of the limb to be operated. The Esmarch bandage, which is used in lower limb surgery mostly for liposuction, minimizes the edema and bruising commonly associated with this type of surgery; the edema and bruising can be influenced by the anatomy of the region and the trauma of the surgery itself9,10. Most authors describe the use of infiltration of a local anesthetics solution associated to vasoconstrictors, and mention the importance of the infiltration to maintain the surgery within a single surgical plane.
The patients included in the present study had a good postoperative response with only intravenous analgesia during the first 24 hours. However, after this period, patient number 4, who had severe sequelae from trauma and deviation of the leg axis due to a fracture, had severe pain during the first week, and was therefore treated with analgesics and anti-inflammatory drugs. The complications in this patient are believed to be the result of the intense fibrosis that permeated all anatomical planes.
In 3 patients, the existing scars were used for the insertion of the implant, as they were in the upper third of the leg. Glicenstein3, the first author to propose the treatment of amyotrophy with silicone implants, argued that in the presence of scarring from previous interventions, the incision should be 6 to 8 cm long in the upper third of the leg. In the remaining 2 patients, who had no previous scars, although several access routes were possible, the incision was made in the popliteal crease. This type of incision is preferred by most surgeons2,7,12 because it provides an adequate surgical field, even with a small scar, and it follows the natural crease of the leg. However, hypertrophic scarring may occur as a consequence of the traction exerted on the scar; this was observed in 2 cases in the present study. In patient 5, the post-operative follow-up period was limited to 3 months, and therefore, the long-term outcome of this complication could not be assessed. This patient is currently under conservative treatment.
One patient developed implant herniation, with migration of the implant to a higher position. Niechajev13 reported the importance of reaching the most distal portion of the cavity and filling it completely during implant surgery. A failure in this surgical procedure might cause herniation of the implant. This author argues that this surgical step can be facilitated by the use of proper instruments for dissection and introduction of the implant (the author suggests the use of a blunt introducer of his own design), and stresses the importance of implant and cavity lubrication for the introduction and control of the distal positioning of the implant. Patient 4 in the present study had this type of complication as a result of intense fibrosis in the distal third of the leg; this complication interfered with the extensibility of the tissue and placement of the distal pole of the implant. Four months after the initial surgical procedure, a surgical revision was performed to distally expand the cavity, breaking down the fibrous tissue and correcting the proximal herniation. Capsular contracture does not seem to be a problem for implants in this region, as is the case with breast implants6.
Most of the studies reporting complications associated with this procedure were conducted by its pioneers, 2 or 3 decades ago. The recent improvements in the design and manufacture of implants, instrumentation, antisepsis and analgesia, have significantly decreased the incidence of complications. However, the lack of studies on a sufficiently large number of patients undergoing surgery for the correction of amyotrophy makes it difficult to accurately evaluate the incidence of complications from this surgery.
The review of previous studies also revealed, with few exceptions, that the photographic evaluation of the calves was performed from photographs of the entire leg. This practice, which was used in the initial cases selected in this study, was found to be abandoned by the more recent cases, and evaluation in those studies was performed by photographing the leg at a straight angle7,14. This practice allows for a more accurate comparison of recent pictures and for standardization of the evaluation methodology.
CONCLUSIONS
Calf reconstruction or calf augmentation via the use of implants has evolved in the recent decades as a safe and efficient procedure, providing esthetically satisfactory results. Calf augmentation in patients with lower limb amyotrophy does not improve limb function. However, implant surgery is associated with a high level of satisfaction with regard to the esthetic improvement of the limb. The present literature review was intended to provide deeper insights into the anatomy of amyotrophic lower limbs to optimize implant surgery techniques and to meet the rise in the demand for surgeries from patients with these deformities.
REFERENCES
1. Novack BH. Alloplastic implants for men. Clin Plast Surg. 1991;18(4):829-55.
2. Niechajev I. Calf augmentation and restoration. Plast Reconstr Surg. 2005;116(1):295-305.
3. Glicenstein J. Correction of amyotrophies of the limbs with silicone prosthesis inclusion. Rev Bras Cir. 1979;69:117-22.
4. Lemperle G, Kostka K. Calf augmentation with new solid silicone implants. Aesthetic Plast Surg. 1993;17(3):233-7.
5. Carlsen LN. Calf augmentation: a preliminary report. Ann Plast Surg. 1979;2(6):508-10.
6. Szalay LV. Twelve years' experience of calf augmentation. Aesthetic Plast Surg. 1995;19(5):473-6.
7. Aiache AE. Calf implantation. Plast Reconstr Surg. 1989;83(3):488-93.
8. Howard PS. Calf augmentation and correction of contour deformities. Clin Plast Surg. 1991;18(3):601-13.
9. Martín MC. Comprehensive liposuction of lower limbs: basic concepts. Aesthetic Plast Surg. 1996;20(1):49-52.
10. Watanabe K. Circumferential liposuction of calves and ankles. Aesthetic Plast Surg. 1990;14(4):259-69.
11. Niechajev I, Sevcuk O. Long-term results of fat transplantation: clinical and histologic studies. Plast Reconstr Surg. 1994;94(3):496-506.
12. Aiache AE. Calf contour correction with implants. Clin Plast Surg. 1991;18(4):857-62.
13. Niechajev I. Mammary augmentation by cohesive silicone gel implants with anatomic shape: technical considerations. Aesthetic Plast Surg. 2001;25(6):397-403.
14. Carlsen LN, Voice SD. Calf augmentation. In: Vistnes LM, ed. Procedures in plastic surgery: how they do it. Boston: Little, Brown; 1991. p.281-94.
1. Specialist member of the Brazilian Society of Plastic Surgery (SBCP), Plastic Surgeon of Hospital Universitário of Universidade Federal de Campina Grande, Campina Grande, PB, Brazil.
2. Patron of the SBCP, Member of the National Academy of Medicine and Brazilian Academy of Letters, Full Professor at the Medical Post-Graduation Course of Plastic Surgery at Pontifícia Universidade Católica do Rio de Janeiro (PUC-RJ) and at Instituto de Pós-Graduação Médica Carlos Chagas, Rio de Janeiro, RJ, Brazil.
3. Full-time member and 2nd Vice-president of the SBCP, Assistant Professor at the Medical Post-Graduation Course of Plastic Surgery at PUC-RJ and at Instituto de Pós-Graduação Médica Carlos Chagas, Rio de Janeiro, RJ, Brazil.
4. Doctoral candidate at the Medicine Course of Universidade Federal de Campina Grande, trainee at the Plastic Surgery Service of Hospital Universitário Alcides Carneiro of Universidade Federal de Campina Grande, Campina Grande, PB, Brazil.
Correspondence to:
Thiago Oliveira Lopes de Cavalcanti
Av. Edson Ramalho, 883 - Manaíra
João Pessoa, PB, Brazil - CEP 58038-10
E-mail: t-cavalcanti@uol.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: June 13, 2011
Accepted: September 6, 2011
Study conducted at Instituto Ivo Pitanguy, at the 38th Nursing service of Santa Casa da Misericórdia, Rio de Janeiro and at their associate services in Rio de Janeiro, RJ, Brazil.
Study conducted as a thesis for the Post-Graduation Course in Plastic Surgery at Instituto Ivo Pitanguy, Rio de Janeiro, RJ, Brazil, and was submitted in January 2010.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter