

Original Article - Year 2011 - Volume 26 -
Use of the vermilion myomucosal flap with or without the mentolabial skin flap for lower lip reconstruction
Uso do retalho miomucoso do vermelhão associado ou não ao retalho cutâneo mentolabial na reconstrução do lábio inferior
ABSTRACT
Background: Several techniques that have been described for reconstructing the lower lip often produce microstomia, commissure distortion, functional impairment, and decreased sensitivity. A technique for preserving neuromuscular tissue during a single-stage lip reconstruction is reported in this study. This technique involves the use of the vermilion myomucosal advancement flap with or without the mentolabial skin flap. Methods: This study analyzed 17 male patients with squamous cell carcinoma. The mean patient age was 54.8 years, and incidence of lip defects after resection ranged from 20% to 85%. Results: Infection, nerve damage, or the requirement for surgical revision was not observed in any patient during the follow-up period of three months. Three patients had microstomia with slight posterior enlargement of the lip. All patients had good sensitivity and adequate sphincter continence. Conclusions: The use of the vermilion myomucosal flap with or without the mentolabial skin flap resulted in a minimal risk of microstomia or functional incompetence. This procedure is performed in a single surgical stage and has good aesthetic and functional results for reconstruction of up to 80% of the lower lip.
Keywords: Lip/surgery. Surgical flaps. Reconstructive surgical procedures.
RESUMO
Introdução: Várias técnicas têm sido descritas para a reconstrução do lábio inferior, muitas vezes produzindo microstomia, distorção da comissura, incapacitação funcional ou diminuição da sensibilidade. Neste trabalho, é relatada uma técnica com preservação de tecido neuromuscular para reconstrução labial em um único estágio, através do uso de retalho de avanço miomucoso do vermelhão, com ou sem retalho de pele mentolabial. Métodos: Foram analisados 17 pacientes do sexo masculino, portadores de carcinoma de células escamosas, com média de idade de 54,8 anos, com defeitos labiais pós-ressecção de 20% a 85%. Resultados: Durante um período de 3 meses de seguimento pós-operatório, nenhum paciente apresentou infecção, lesão nervosa ou necessitou de revisão cirúrgica. Três pacientes apresentaram microstomia, com alargamento discreto posterior do lábio. Todos os pacientes apresentaram boa sensibilidade e continência esfincteriana adequada. Conclusões: O uso do retalho miomucoso de vermelhão com ou sem retalho de pele mentolabial resultou em risco mínimo de microstomia ou incompetência funcional, sendo realizado em estágio cirúrgico único, além de demonstrar bons resultados estéticos e funcionais para a reconstrução de até 80% do lábio inferior.
Palavras-chave: Lábio/cirurgia. Retalhos cirúrgicos. Procedimentos cirúrgicos reconstrutivos.
The lips, which represent the most important aesthetic and functional element of the lower third of the face, function in swallowing, articulation, expression of emotion, and especially in oral competence. Lip reconstruction has been described in ancient records, including one report from a Roman surgeon in 25 BC; this report described relaxation incisions on the cheeks of a soldier for primary closure of the lip. These surgical techniques have undergone little variation from that time until the mid-nineteenth century, in which multiple modifications have been suggested. However, the general principles of lip reconstruction have not changed substantially1. Several methods have been proposed for lower lip reconstruction, which may be indicated based on the extent of loss of substance in patients. There are more than 200 surgical techniques related to this theme in the literature2.
Infections, trauma, congenital abnormalities, and tumors are the most common causes of lower lip deformities. Lip cancer is the most common malignant lesion in the oral cavity, with an incidence of approximately 15%. Squamous cell carcinoma is a malignant tumor that is 20 times more prevalent in the lower lip than in the upper lip, with an incidence of regional metastasis ranging from 11% to 18% 3. Malignant lesions with the worst prognosis are represented by tumors of >2 cm; these tumors show little differentiation on anatomical-pathological examination, are located on the upper lip or commissure, and show regional lymphatic involvement or perineural invasion3.
When planning lower lip repair, it is essential to evaluate the extent of loss of the substance to be reconstructed. Wedge resection and primary closure are very common options for repair of up to one-third of the lower lip. However, losses of more than one-third require more complex reconstructions with more elaborate surgical planning and the possibility of using pedicle flaps (local or distant) or free flaps4.
The vermilion is the most apparent cosmetic portion of the lip, and its color is derived from the extensive superficial vascularization in this area5. The following planes from the surface can be identified in the cross-section of the lip: epidermis, dermis, subcutaneous tissue, oral orbicularis muscle, submucosa, and mucosa. The blood supply is provided by the superior and inferior labial arteries, which arise from the facial artery and extend towards the oral commissure. The labial artery can be identified among the planes of the oral orbicularis muscle and the submucosa in the vermilion-mucosal transition. Venous drainage is provided by the anterior facial vein. Sensory innervation of the upper lip is provided by the infraorbital branch from the second division of the trigeminal nerve (cranial nerve V), which emerges through the infraorbital foramen in the jaw. Sensory innervation of the lower lip is provided by the mental nerve, which emerges through the mental foramen. Motor innervation is provided by branches of the facial nerve (VII cranial nerve) through the following branches: the buccal branch, which innervates the oral orbicularis muscle and levator labii; the marginal mandibular branch, which innervates the oral orbicularis muscle; and the lower lip depressor. This last branch is very susceptible to injury in the middle third of the mandibular body, where it is more superficial. In addition to the oral orbicularis muscle, the following muscles are related to the lower lip: buccinator, depressor anguli oris, lower lip depressor, and mentalis6.
The major muscle responsible for closing the lips is the oral orbicularis. The function of the oblique and deep muscle fibers is to cover and contain the dental arch, while the function of the superficial fibers is to advance the lip in relation to the coronal facial plane. The lips are primarily raised through the upper levator muscle of the lip. Although the angle levator and zygomatic muscles have a synergistic action in lip elevation, they also cause posterior traction of the lip. Lip depression is performed through the combined action of the platysma muscles, lower lip depressor, and oral angle depressor. The joint action of these muscles modulates and synchronizes the position of the oral orbicularis muscle, and these muscles, along with the constrictor muscles of the larynx, oral orbicularis, and buccinator, form a functional ring unit. Any disturbance of this unit leads to lip imbalance1.
Physiological reconstruction of the lip requires broad anatomical knowledge and consideration of the muscular lines of the face, which define the aesthetic units of this region. Three units should be evaluated when planning lower lip reconstruction: nasolabial, mentolabial, and chin filter7.
This study describes the authors' experience with lower lip reconstruction in patients with extensive losses of total thickness after tumor resection.
METHODS
This study included 17 patients with labial defects resulting from resection of squamous cell carcinoma. In all cases, closure of the lower lip was accomplished using the vermilion myomucosal advancement flap. All patients were male with an average age of 54.8 years (range, 34 to 77 years). The extent of the resulting defects after tumor excision with clear margins ranged from a minimum of 20% to a maximum of 85% of the lower lip (67% on average), with commissure involvement in 3 patients. The follow-up period ranged from a minimum of 6 months to a maximum of 3 years.
Surgical Technique
The surgeries were performed under general anesthesia. Prior to administration of local anesthetic (solution of 1% lidocaine and epinephrine 1:100,000 units), a preoperative marking was made in which a line was drawn on the mucous-skin transition along the vermilion to the labial commissure bilaterally.
The surgical technique combined the advancement flap of the oral orbicularis muscle and mucosa, with or without the mentolabial skin flap. The muscle plane was reached from the incision in the mucous skin line and was followed caudally over approximately 1 cm (Figure 1). From that point, the incision was completed through the transfixed oral orbicularis muscle in the contralateral direction to the oral mucosa, with the creation of a pedicled myomucosal flap in the lower labial artery (Figures 2 and 3). The oral orbicularis muscle was reapproximated with 5-0 vicryl with the lip closer to the dental arch. The vermilion was reapproximated, aligned, and sutured using 5-0 monofilament nylon in the dry mucosa and 5-0 vicryl in the wet mucosa (Figure 4). The lower edge of the oral orbicularis muscle was subsequently approximated and sutured to the remaining muscles of the mentolabial and mental units using 5-0 vicryl. Thus, the myomucosal flap was reorganized in relation to the other mentolabial muscles. Shortly thereafter, where necessary, a skin flap was marked on the mentolabial unit with a lateral base and a distal end in the midline of the chin. The upper limit of the flap depended on the remaining tissues. In cases where the loss of substance was located strictly in one-half of the lip, the upper limit of the flap was the lower limit of the excision. In the cases with remaining vermilion, the upper limit of the flap was the mucocutaneous transition of the lip to the labial commissure. In this case, the upper limit of the contralateral half was defined solely with the mucocutaneous line of the vermilion up to the labial commissure. In cases where the defect included the two mentolabial halves, the upper limit of both flaps was similar to that in cases of unilateral defect. The lower limit of the flap was defined by a line surrounding the chin unit.

Figure 1 - Schematic drawing of the mucosa and skin incision line: the dissection separates the myomucosal flap from the skin flap.
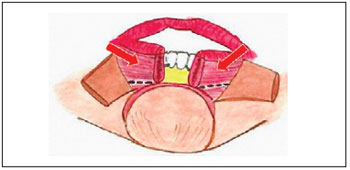
Figure 2 - Schematic drawing of the dissected myomucosal flap.

Figure 3 - Schematic drawing of the dissected bilateral mentolabial skin flap.

Figure 4 - Schematic drawing of the myomucosal flap and closed local muscles in the midline. The skin flaps are not yet positioned.
Flap lifting was performed in the mid-lateral direction up to the projection of a perpendicular line in relation to the lip in the labial commissure on each side. Both flaps were advanced in the superior and medial directions with approximation or up to the distal intersection on the midline of the chin; this depended on the laxity of each patient. Mentolabial longitudinal enlargement occurred where the intersection of skin flaps was possible. The oblique distal end produced a better condition for distal accommodation of the flaps. When the upper limit of the skin flap was asymmetrical, it was possible to rotate the upper segment on the lower, aiming at lengthening the mentolabial unit. The skin was sutured using 5-0 monofilament nylon thread. The vermilion was approximated, aligned, and sutured using 5-0 monofilament nylon in the dry mucosa and 5-0 vicryl in the wet mucosa (Figure 5).

Figure 5 - A 52-year old patient who underwent reconstruction of 70% of the lower lip. In A, preoperative tumoral aspect and marking of areas to be dissected. In B, vermilion myomucosal flaps dissected bilaterally. In C, skin flaps dissected bilaterally. In D, immediate postoperative aspect: the myomucosal advancement flap is associated with the mentolabial skin flap with distal intersection.
RESULTS
Infection, injury to the mental nerve (paresthesia or anesthesia), or locoregional recurrence was not observed in any patient during the follow-up period. Three patients had microstomia with slight posterior enlargement of the lip. All patients had adequate oral competence and minimal changes in lower lip sensitivity, which were clinically evaluated during the postoperative period (Figures 6 to 8). No patient experienced flap necrosis, paralysis, and praxis of the facial nerve or required surgical revision.

Figure 6 - A 42-year old patient with impairment of 80% of the lower lip. In A, preoperative aspect. In B and C, postoperative result demonstrating the neurologically intact oral orbicularis muscle.
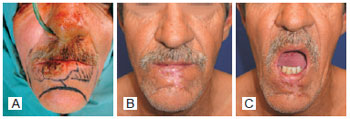
Figure 7 - In A, preoperative aspect. In B and C, postoperative result demonstrating minimal aesthetic and functional changes.

Figure 8 - In A, preoperative aspect. In B and C, postoperative result demonstrating labial containment.

Figure 9 - Indigenous Botocudos and Zoés people.
All patients tolerated their previous diet (using a dental prosthesis, if necessary). The patients who underwent reconstruction of defects affecting the commissure also underwent previously planned commissuroplasty in order to maximize the normal angulation of the region.
DISCUSSION
The main goal in lower lip reconstruction is good coverage of the vermilion and the adjacent skin associated with the reconstruction of oral sphincter competence, with minimal aesthetic and functional changes. Loss of substance in <30% of the lower lip area can be repaired by direct approximation and closure; however, an alternative method is required in cases of major loss of substance, with frequent use of transference flaps between the upper and lower lips. The existence of a defect is generally observed in both the lower lip skin and vermilion after tumor resection, and it is necessary to use adjacent or upper lip tissues in the reconstruction. These repairing methods result in significant microstomia. Moreover, regional skin tissues may cause a functional deficit when transferred to the lip region because they lack a neurologically intact oral orbicularis muscle.
In this technique, first reported by Sabattini in 1838 (Italy), the vermilion and the adjacent skin from the lower lip are transferred to the upper lip. In 1848, Stein, (Denmark) described bilateral transfer flaps from the upper lip to the lower lip. Gordon Buck was the first surgeon to describe the lip transfer flap in the English language in 1864 (United States) during the Civil War. However, the method became known in the medical community only after Abbé demonstrated his technique of flap transference for lip reconstruction in 1898. Abbé flaps, which can be used for medial or lateral defects near the labial commissure, should have a width equal to half the length of loss of substance, and a triangular area is produced based on the vermilion of the opposite lip. Medial losses of the lower lip are repaired by the Abbé flap technique using tissues adjacent to the labial filter; this causes deformity in the aesthetic unit of the filter. On the other hand, lateral labial losses cause more deformities in the labial commissure. Moreover, this flap requires two surgical procedures for the pedicle release and, in certain situations, requires labial commissure reconstruction, as amended in the transfer of the flap. Estlander described a technique that can be defined as an Abbé flap for labial commissure in 1872. According to Smith8, Estlander and Abbé flaps demonstrate normal electromyographic tracing one year after the operation, albeit with 60% to 70% return of muscular function of the oral orbicularis muscle. In addition, major losses of substance may cause changes in the competence of the oral orbicularis muscle8.
In 1845, Dieffenbach (Germany) was the first to suggest lower lip reconstruction using bilateral medial advancement flaps from the cheeks. In 1853, Bernard introduced a technique with bilateral triangular Burow's resection in the nasolabial folds. This procedure has undergone subsequent modifications suggested by Ginestet in 1946, by Freeman in 1958, and by Webster in 1960. According to the Webster technique, the buccinator and orbicularis muscles are laterally incised to the lateral commissure, and this maneuver preserves a few innervated muscle fibers. The Bernard-Webster cheek flap may impair labial sphincter function and consequently cause sialorrhea2,8-10.
In 1920, Guillies advocated a technique using two flaps in a single block by medial advancement of the mentolabial tissues for repairing losses of up to 75% of the lower lip6.
Karapandzic11 described the neurovascular myocutaneous flap in 1974. This technique, which avoids the muscle fiber section of the oral orbicularis muscle and results in minimal sensory and motor damage, may also be used for losses of substance of >60% of the lip. Its main disadvantage is microstomia, which is found in the reconstruction of large losses of lip substance12.
In 1997, Bayramiçli et al.13 (Turkey) reported a technique with V-Y advancement of two myocutaneous flaps on each side of the chin for lower lip reconstruction, with mentolabial muscle reorientation and preservation of mental nerve sensitivity.
In 2002, Wechselberger et al.10 (Austria) recommended preservation of the muscles forming the labial commissure, especially the oral orbicularis, so that the innervation, function, and sensitivity of the lower lip would be only slightly changed.
Ducic et al.1 (United States) (USA) described the use of the myomucosal advancement flap for lower lip reconstruction in 2005. This technique is indicated for 50% to 80% of loss of substance with minimal risk of microstomia or sphincter incompetence.
In 2006, Civelek et al.14 (Turkey) reported results obtained from 31 patients who underwent lower lip reconstruction with innervated flaps (18 patients) or randomized flaps (13 patients). The authors found no difference between the two groups in terms of sphincter competence and electromyographic findings14.
In 2007, Ethunandan et al.12 (United Kingdom) described 7 cases of upper and lower lip reconstruction using the Karapandzic flap. Despite microstomia, no functional problems occurred. This result may be related to the laxity of perioral tissues and the preservation of both motor and sensory innervation.
In 2009, Unsal Tuna et al.2 (Turkey) obtained good results from a proposed technique based on Bernard flap modification. The insertion of commissure muscles is preserved with this technique, resulting in the maintenance of innervation and labial sphincter function.
Indigenous communities in Brazil, such as Zoés and Botocudos, demonstrate great laxity potential of the lower lip. These communities produce oral-facial deformations as forms of socio-cultural differentiation in their communities. When a child reaches 8 years of age, Zoés use a long monkey bone to perforate the mentolabial region and implant a cylindrical timber artifact. The size of the artifact is progressively increased and may reach a length of 15 cm and a width of 4 cm in adulthood. In addition to mandibular alveolar deformation, this artifact causes distension of the soft tissues in the labial and mentolabial units (Figure 9). However, Botocudos are unmatched in the demonstration of great laxity of the lower lip. This community also begins a deforming ritual during the pre-pubescent period by perforating the mentolabial region and implanting a disk-shaped timber artifact. This procedure causes gradual stretching of the vermilion, creating a natural myomucosal flap15.
CONCLUSION
The ideal plan for lip reconstruction should maintain volume, function, and aesthetic features with minimal morbidity at the donor site. The results of this study demonstrate that use of the vermilion myomucosal flap with or without the mentolabial skin flap is the closest we could come to achieving these ideals. The basic principle of this study is based on the greater redundancy in the vermilion tissue compared to the skin portion of the lip. Although skin elasticity is very low in the orolabial region compared to other regions of the face and neck, the vermilion's redundancy is a favorable factor for the reconstruction. Another great advantage is that the myomucosal flap maintains lower lip innervation, reducing the risk of microstomia1,3,9. The defect must be carefully evaluated because a minimum of 20% of remaining lip (unilateral or bilateral distribution) is required to obtain good functional and aesthetic results. The advancement of the myomucosal flap independent from the skin flaps results in a significantly increased transverse dimension of the lip and greater oral competence. Labial volume and aesthetics are maintained because of the recruitment of similar adjacent tissues, and the incision is easily concealed in the vermilion. The flap is reliable, easily produced, and is associated with favorable long-term results. No significant problems were associated with flap production in the studied patients.
REFERENCES
1. Ducic Y, Athre R, Cochran CS. The split orbicularis myomucosal flap for lower lip reconstruction. Arch Facial Plast Surg. 2005;7(5):347-52.
2. Unsal Tuna EE, Oksüzler O, Ozbek C, Ozdem C. Functional and aesthetic results obtained by modified Bernard reconstruction technique after tumour excision in lower lip cancers. J Plast Reconstr Aesthet Surg. 2010;63(6):981-7.
3. Nassif Filho ACN, Shibuto JR, Tarlé RG, Arnoud J, Maestri JEG. Cirurgia reconstrutiva de lábio inferior com recuperação estético-funcional: relato de dois casos. (Lower lip reconstructive surgery with aesthetic-functional recovery: two cases report) Rev Assoc Med Bras. 1998;44(3):256-60.
4. Santos DAOS, Haddad A. Neoplasias cutâneas. In: Ferreira LM, ed. Guia da cirurgia plástica. (Guide for plastic surgery) Barueri: Manole; 2007. p. 259-68.
5. Mutaf M, Bulut O, Sunay M, Can A. Bilateral musculocutaneous unequal-Z procedure: a new technique for reconstruction of total lower-lip defects. Ann Plast Surg. 2008;60(2):162-8.
6. Bailey BJ, Calhoun KH, Friedman N. Atlas of head & neck surgery: otolaryngology. 2nd ed. Philadelphia: Lippincott Williams & Wilkins; 2001.
7. Breitsprecher L, Fanghänel J, Metelmann HR, Mlynski G, Würfel F, Freise K, et al. The influence of the muscles of facial expression on the development of the midface and the nose in cleft lip and palate patients. A reflection of functional anatomy, facial esthetics and physiology of the nose. Ann Anat. 1999;181(1):19-25.
8. Smith JW. The anatomical and physiologic acclimatization of tissue transplanted by the lip switch technique. Plast Reconstr Surg Transplant Bull. 1960;26:40-56.
9. Turgut G, Ozkaya O, Kayali MU, Tatlidede S, Hüthüt I, Baş L. Lower lip reconstruction with local neuromusculocutaneous advancement flap. J Plast Reconstr Aesthet Surg. 2009;62(9):1196-201.
10. Wechselberger G, Gurunluoglu R, Bauer T, Piza-Katzer H, Schoeller T. Functional lower lip reconstruction with bilateral cheek advancement flaps: revisitation of Webster method with a minor modification in the technique. Aesthetic Plast Surg. 2002;26(6):423-8.
11. Karapandzic M. Reconstruction of lip defects by local arterial flaps. Br J Plast Surg. 1974;27(1):93-7.
12. Ethunandan M, Macpherson DW, Santhanam V. Karapandzic flap for reconstruction of lip defects. J Oral Maxillofac Surg. 2007;65(12):2512-7.
13. Bayramiçli M, Numanoglu A, Tezel E. The mental V-Y island advancement flap in functional lower lip reconstruction. Plast Reconstr Surg. 1997;100(7):1682-90.
14. Civelek B, Celebioglu S, Unlu E, Civelek S, Inal I, Velidedeoglu HV. Denervated or innervated flaps for the lower lip reconstruction? Are they really different to get a good result? Otolaryngol Head Neck Surg. 2006;134(4):613-7.
15. Dietze S, Winkelmann D, Garve R, Blens T, Fanghänel J, Proff P, et al. Ritually induced growth disturbances and deformities of the orofacial system: a contribution to cranial morphogenesis. Ann Anat. 2007;189(3):304-8.
1. Master's degree, full member of the Brazilian Society of Plastic Surgery (SBCP), head resident physician of the Plastic Surgery Service of Hospital São Lucas of Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil.
2. PhD, Chief of the Plastic Surgery Service of Hospital São Lucas of Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil.
3. Resident physician at the Plastic Surgery Service of Hospital São Lucas of PUCRS, Porto Alegre, RS, Brazil.
Correspondence to:
Milton Paulo de Oliveira
Av. Guaporé, 441/301 - Petrópolis
Porto Alegre, RS, Brazil - CEP 90470-230
E-mail: miltonpaulo.poa@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: June 26, 2011
Accepted: August 9, 2011
Study conducted at the Plastic Surgery Service of Hospital São Lucas of Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter