ABSTRACT
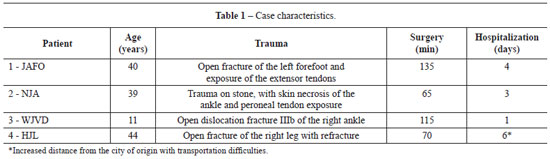
The distal regions of the lower limbs, including the lower third of the legs and feet, are very prone to soft tissue loss due to trauma and trophic lesions. The anterior part of the tibia with its slightly thick, vulnerable cover and large number of tendons, which cannot remain exposed, requires fast and complex skin coverage. The blood-flow direction, lack of muscle bellies for flaps, and inelastic skin for viable randomized flaps complicate this situation. In the past, intermediate-transfer flaps and cross-legged flaps were used for skin coverage, with drawbacks: they require more than one surgery, cause great discomfort to the patient, and are not always effective. Microsurgery is an option that greatly helps to cover lesions at this site; however, it requires a team with specialized training and equipment. Donor areas that are larger, may cause functional impairment, and use larger vascular trunks. Fasciocutaneous flaps with reverse flow may help to cover small and medium lesions at this location, with minor aesthetic and functional sequelae, and less surgical time. They are an effective surgical option because of their ease, safety, and versatility. The aim of this paper is to demonstrate the use of reverse-flow supramalleolar flaps in 4 different situations and discuss their advantages and applications.
Keywords:
Surgical flaps. Leg injuries. Ankle injuries. Lower extremity/surgery.
RESUMO
As regiões distais do membro inferior, incluindo o terço inferior da perna e os pés, são áreas muito propensas a perda de partes moles por trauma e lesões tróficas. A posição anterior da tíbia, com sua cobertura pouco espessa e vulnerável, além da grande quantidade de tendões, que não podem permanecer expostos, exigem uma cobertura cutânea rápida e, ao mesmo tempo, complexa. A situação em relação à direção do fluxo sanguíneo, a escassez de ventres musculares para retalhos e pele pouco elástica para retalhos randomizados viáveis complicam esta situação. No passado, retalhos com transferência intermediária foram utilizados; assim como os de perna cruzada, "cross leg", ainda são, com desvantagens importantes: dependem de mais de um tempo cirúrgico, geram muito desconforto ao paciente e nem sempre são eficazes. A microcirurgia tornou-se uma opção que contribui muito para cobertura de lesões neste aspecto, porém, depende de equipe com treinamento e material especializado. As áreas doadoras são maiores, podem causar relativo déficit funcional e utilizam troncos vasculares maiores. Os retalhos fasciocutâneos de fluxo reverso podem contribuir para a cobertura de lesões pequenas e médias nesta localização, com sequelas funcionais e estéticas menores; e menor tempo cirúrgico. Constitui eficiente opção cirúrgica por sua facilidade, segurança e versatilidade. Neste estudo, temos o objetivo demonstrar o retalho supramaleolar de fluxo reverso utilizado em 4 casos, com aplicações em situações diferentes, com resultados satisfatórios de fácil execução e reprodução.
Palavras-chave:
Retalhos cirúrgicos. Traumatismos da perna. Traumatismos do tornozelo. Extremidade inferior/cirurgia.