

Original Article - Year 2011 - Volume 26 -
Results of ulnar nerve decompression and anterior transposition at the elbow
Resultados da descompressão e anteriorização do nervo ulnar no cotovelo
ABSTRACT
Introduction: Ulnar nerve compression is the second most frequent compressive neuropathy. It mostly occurs in the cubital tunnel at the elbow, and its surgical treatment is controversial. Here, we aim to describe the results of subcutaneous decompression and anterior transposition of the ulnar nerve performed by the Plastic Surgery Team of the Sarah Brasilia Hospital over a 6-year period. Methods: We assessed the results of decompression and anterior transposition of the ulnar nerve performed in 58 patients between 2001 and 2007 according to the modified McGowan classification. Results: Elbow fracture and leprosy were the most frequent causes of ulnar nerve compression, followed by heterotopic ossification due to spinal cord and/or brain injury. Flexor muscle retinaculotomy, Guyon's canal decompression, and tendon transfer for intrinsic muscles were performed in 57% of the patients. Overall, 80% of the patients demonstrated good or excellent results; the remaining 20%, especially those with diabetes or leprosy, exhibited complications such as neuropathic pain, complex regional pain, and persistence of symptoms. Conclusion: Decompression and anterior transposition of the ulnar nerve at the elbow reduces tension and neuritis. Moreover, it is possible to obtain 80% good or excellent results in patients with Grade II and Grade III compression.
Keywords: Nerve Compression Syndromes. Cubital Tunnel Syndrome. Ulnar Nerve.
RESUMO
Introdução: A compressão do nervo ulnar no cotovelo é a segunda causa mais frequente de neuropatia compressiva no membro superior. Na maioria dos casos, a compressão ocorre no canal cubital, vulnerável à compressão extrínseca, intrínseca ou idiopática. O tratamento cirúrgico é controverso. Método: Os autores descrevem os resultados da descompressão e transposição anterior do nervo ulnar realizadas em 58 pacientes. Resultados: Identificou-se como causa principal a fratura de cotovelo e a hanseníase. Na Rede Sarah, entretanto, têm sido frequente (15%) também as indicações por compressão causada por ossificação heterotópica em casos de lesados medulares e/ou cerebrais. Realizamos 57% de procedimentos associados à retinaculotomia dos flexores, descompressão no canal de Guyon e transferência tendínea para músculos intrínsecos. Obteve-se 80% de bons e excelentes resultados, 20% de complicações, dor neuropática, distrofia simpática reflexa e manutenção dos sintomas, observadas em pacientes diabéticos e portadores de hanseníase.
Palavras-chave: Síndromes de Compressão Nervosa. Síndrome do Túnel Ulnar. Nervo Ulnar.
Ulnar nerve compression is the second most frequent cause of compressive neuropathy. It can occur at the elbow, arcade of Struthers, intermuscular septum, medial epicondyle, medial head of the triceps, cubital tunnel with Osborne's band, aponeurosis of the pronator and flexor muscles, and the arch of the ulnar carpal flexor muscle1-3, resulting in ischemia and chronic neuritis. Its etiology includes bone abnormalities, fractures, tumors, lymph nodes, fascial constriction, subluxation of the nerve at the medial epicondyle during elbow flexion, and heterotopic ossification4,5. The condition is diagnosed clinically, supplemented by electromyographic examination1-3,6.
Conservative treatment can be effective, but decompression of the ulnar nerve at the cubital tunnel is generally performed in the absence of clinical improvement. In 1930, Learmonth7 popularized the technique for decompression and transposition of the ulnar nerve at the elbow. Since then, several procedures have been described, although the best option is still controversial.
The aim of this paper is to describe the results of subcutaneous decompression and anterior transposition of the ulnar nerve at the elbow performed by the Plastic Surgery Team of the Sarah Brasilia Hospital over a 6-year period.
METHODS
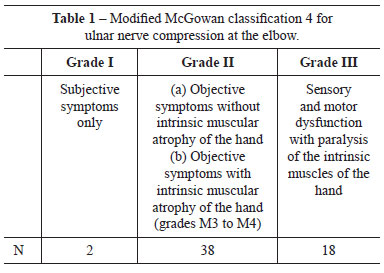
Patients who underwent decompression and anterior transposition of the ulnar nerve at the elbow at the Hospital Sarah Brasília, between 2001 and 2007 were evaluated by age, gender, and etiology. Their sensory, motor, subjective, and objective symptoms and signs were classified preoperatively and postoperatively according to the modified McGowan classification2,4 (Table 1). Epi-Info version 3.4.3 was used for data analysis.
Surgery was indicated for the patients who presented with the following features: persistent symptoms after conservative treatment (protective measures, use of orthosis, and administration of amitriptyline and anti-inflammatory drugs for 4 to 12 months), decreased sensitivity in the Semmes-Weiss test and motor evaluation according to the Medical Research Council, ulnar nerve compromise in the cubital tunnel determined by electromyographic examination, and/or extrinsic compression (e.g., cases of leprosy and heterotopic ossification) evidenced by imaging (Figure 1 and 2).

Figure 1 - Preoperative view of patients with signs of ulnar nerve paralysis, radiologic examination, and intraoperative view presenting caseous abscess due to ulnar leprous neuritis. Decompression and anterior transposition of the ulnar nerve in the cubital tunnel were performed.
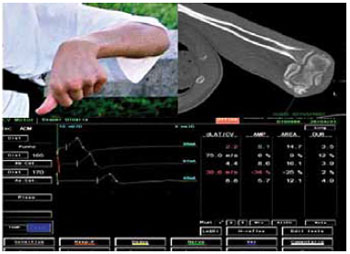
Figure 2 - A patient with cranioencephalic trauma sequelae who presented with flexion deformity of the elbow due to heterotopic ossification associated with ulnar nerve compression in the cubital tunnel, observed by radiologic examination of the elbow and motor conduction study of the ulnar nerve.
Surgical Technique
The patients underwent plexus blocking, axillary or general anesthesia, and emptying of the upper limb with an Esmarch bandage. An incision of 10 to 12 cm was made in the medial portion of the elbow (Figure 3). Dissection of the tissue and proximal and distal nerves was performed while preserving the medial cutaneous branch of the forearm and ulnar nerve branches. After opening the intermuscular septum and Struthers' arcade, we performed subcutaneous anterior transposition while preserving the vasculature. The elbow was flexed to assess possible constraints to movement or dislocation of the nerve. Monocryl 3.0 sutures were placed, and the elbow was immobilized in the flexed position with a posterior splint for 2 to 3 weeks.

Figure 3 - Surgical sequence: marking, decompression, and anterior transposition of the ulnar nerve at the elbow.
The patients underwent a physiotherapeutic and ambulatory program according to McGowan's protocol4 preoperatively and postoperatively. They were restricted from work for at least 8 weeks postoperatively.
RESULTS
Fifty-eight patients underwent subcutaneous decompression and anterior transposition of the ulnar nerve at the elbow between 2001 and 2007; 6 were bilaterally operated. All had compressive neuropathy of the ulnar nerve at the elbow as well as objective and subjective symptoms. Female patients aged between 40 and 60 years were predominantly affected (Figure 4). One patient discontinued the treatment in the third postoperative month. The average follow-up time was 1 year (range = 6 months to 6 years).
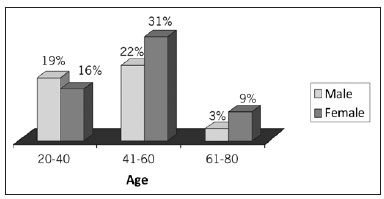
Figure 4 - Distribution of ulnar nerve compression according to gender and age.
The cause of compression was fracture of the elbow in 11 patients, leprosy in 9 patients, heterotopic ossification due to brain and/or spinal cord injury in 9 patients, gout or ganglion extrinsic compression and unidentified causes in 8 patients (Figure 5). Other compressive syndromes such as carpal tunnel syndrome and Guyon's canal syndrome were noted in 18 and 9 patients, respectively.
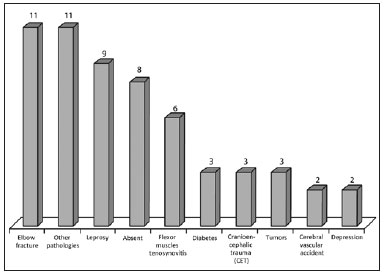
Figure 5 - Associated conditions.
The eligibility criteria for the surgical procedure were based on persistent symptoms of paresthesia and pain despite conservative treatment and/or the duration of evolution of the compression as well as on the objective findings (sensory and motor alterations) and the results of the electromyographic examination. The latter is considered a less important surgical indication, although it is used to confirm the diagnosis of nerve compression at the elbow according to myelinated and/or axonal findings.
Regarding the results of the electromyographic examination between 8 and 12 months postoperatively, 28 patients showed improvement, with 12 showing normalization; 12 patients had no change; 5 patients experienced sequelae; and 3 experienced worsening of the symptoms. The examination was not performed in the remaining patients. The patients who experienced worsening of their symptoms were diagnosed with leprosy.
Biopsy of the epineurium revealed nonspecific inflammatory processes in 38 (64%) patients, fibrosis in 10 patients (17%), leprosy in 3 patients (5%), recent hemorrhage of the nerve in 1 patient, granulomatous processes in 1 patient, tophaceous gout in 1 patient (Figure 6), and ganglion in 1 patient.

Figure 6 - A patient with extrinsic compression of the ulnar nerve at the elbow due to tophaceous gout.
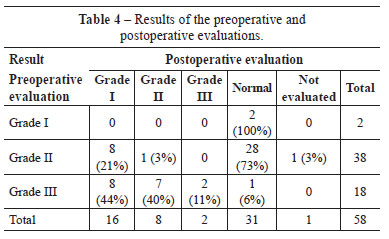
Fifty-six patients were classified preoperatively with McGowan's4 Grade II and Grade III compression (Table 1). These patients presented preoperative sensory and motor objective alterations and constriction of the nerve at the cubital tunnel during surgery. Of 9 patients diagnosed with leprosy, 8 presented with Grade III compression.
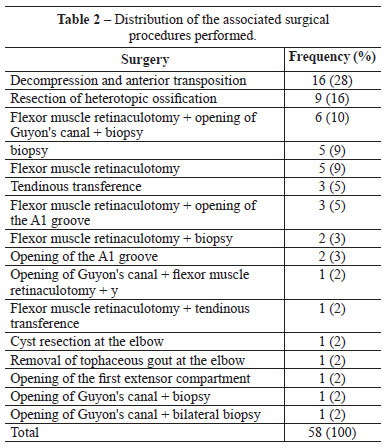
In 28% of the patients, only decompression and anterior transposition were performed, and in 35 patients (57%), the following associated procedures were performed: biopsy of the epineurium, resection of heterotopic ossification, decompression in Guyon's canal and the median nerve in the carpal tunnel, and other procedures (i.e., opening the extensor compartment, opening pulley; Table 2).
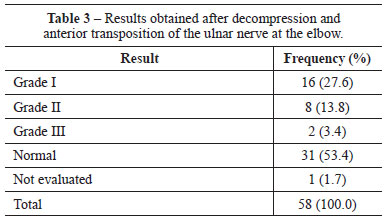
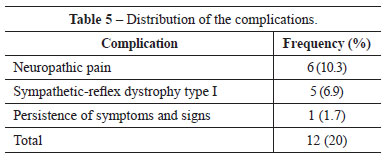
In 53% of the patients, the preoperative symptoms and signs normalized, and in 16 patients (27.6%), we observed improvement compared with the preoperative stage (Grade I). The procedure was effective in 80% of the patients (Tables 3 and 4), but 20% had complications such as neuropathic pain, complex regional pain, and persistence of symptoms (Table 5). In 4 patients with Grade III compression, tendon transfer was performed by using the superficial IV or V flexor tendon according to Zancolli's loop surgery, resulting in improved hand function (Table 6).

DISCUSSION
Surgical treatment of compression neuropathy of the ulnar nerve at the elbow is still controversial and relapses or even failure can occur1,3. The surgical procedures described in the literature are decompression, transposition, and incision of the epicondyle1-3. In a systematic review, Dellon5 reviewed 50 articles, totaling 2000 surgical cases, and noted that the preference of the team remains the main criterion for selecting the surgical procedure. In moderate and severe compression, muscular decompression and transposition give the best results with less recurrence. According to Nathan et al.8, simple decompression is a relatively uncomplicated procedure that preserves the normal anatomy but increases the susceptibility to injury and nerve stretching and the possibility of subdislocation in 2.4% of the patients. In epicondylectomy, Popa and Dubert1 described the advantages of preservation of the blood supply and tissue around the nerve; however, disadvantages include medial instability due to detachment of the anteromedial collateral ligament, loss of protection of the medial epicondyle, pain postoperatively due to osteotomy, nerve subdislocation over the epicondyle, and elbow flexion contracture.
We performed a procedure first described in 19307, with modifications. According to our and other authors' experiences, we performed decompression and transposition of the ulnar nerve in the subcutaneous tissue. This technique has been defended by some authors9 because of the clinical improvement it presents, but it has been criticized by others for causing nerve devascularization10,11 and the possibility of creating a new site of compression. However, preservation of the extrinsic vasculature of the nerve is possible12,13, and appropriate care and technical skills can prevent further compression.
Regarding fibrosis, we consider that all techniques involve some degree of fibrosis due to displacement of the nerve. The quality of the result depends on the time of onset of symptoms and the etiology8,10. We observed neuropathic pain and reflex sympathetic dystrophy as complications, especially in patients with diabetes mellitus and leprosy. Further, we observed 6 cases of dysesthesia without reflex sympathetic dystrophy, possibly due to traction injury of the medial cutaneous branch of the forearm. No patient complained about the more superficial nerve position, but 4 patients presented with continued nerve compression symptoms as described in the literature8,10,11. Of note, among the associated surgical procedures, resection of heterotopic ossification resulted in functional gain of the range of flexion-extension of the elbow and clinical improvement.
Simple decompression would make the nerve more susceptible to compression and trauma and maintain nerve stretching during flexion movements of the elbow. However, decompression and anterior transposition of the ulnar nerve at the elbow reduce the stretch in the groove14, thus reducing tension and neuritis. Moreover, it is possible to obtain 80% good or excellent results in patients with Grade II and Grade III compression.
CONCLUSIONS
Decompression and anterior transposition of the ulnar nerve allowed relief of subjective and objective symptoms and signs of compressive neuropathy of the ulnar nerve in the cubital tunnel in 80% of the patients. Complications were observed in 20% of the patients and were related largely to leprosy.
REFERENCES
1. Popa M, Dubert T. Treatment of cubital tunnel syndrome by frontal partial medial epicondylectomy. A retrospective series of 55 cases. J Hand Surg. 004;29(6):563-7.
2. Lascar T, Laulan J. Cubital tunnel syndrome: a retrospective review of 53 anterior subcutaneous transpositions. J Hand Surg. 2000;25(5):453-6.
3. Hoffmann R, Siemionow M. The endoscopic management of cubital tunnel syndrome. J Hand Surg. 2006;31(1):23-9.
4. McGowan AJ. The results of transposition of the ulnar nerve for traumatic ulnar neurttis. J Bone Joint Surg. 1950;32-B(3):293-301.
5. Dellon AL. Review of treatment results for ulnar entrapment at the elbow. J Hand Surg Am. 1989;14(4):688-700.
6. Paz AC, Carod Artal FJ, Kalil RK. A function of proprioceptors in bone organization: a possible explanation for neurogenic heterotopic ossification in patients with neurological damage. Med Hypotheses. 2007;68(1):67-73.
7. Learmonth JR. A technique for transplanting the ulnar nerve. Surg Gynecol Obstet. 1942;75:792-3.
8. Nathan PA, Myers LD, Keniston RC, Meadows KD. Simple decompression of the ulnar nerve: an alternative to anterior transposition. J Hand Surg Br. 992;17(3):251-4.
9. Lundborg G. Surgical treatment for ulnar nerve entrapment at the elbow. J Hand Surg Br. 1992;17(3):245-7.
10.Manske PR, Johnston R, Pruitt DL, Strecker WB. Ulnar nerve decompression at the cubttal tunnel. Clin Orthop Relat Res. 1992;(274):231-7.
11.Lebreton E, Bourgeon Y, Lascombes P, Merle M, Foucher G. Systematisation de la vaseulartsation de la portton brachmle du neff ulnmre. Annal Chir la Mare. 1983;2:211-8.
12.Rogers MR, Bergfield TG, Aulicino PL. The failed ulnar nerve transposition. Etiology and treatment. Clin Orthop Relat Res. 1991;(269):193-200.
13.Macadam SA, Gandhi R, Bezuhly M, Lefaivre KA. Simple descompression versus anterior subcutaneous and submuscular transposition of the ulnar nerve for cubital tunnel syndrome: a meta-analysis. J Hand Surd Am. 2008;33(8):1314.e1-12.
14.Grewal R, Varitimidis SE, Vardakas DG, Fu FH, Sotereanos DG. Ulnar nerve elongation and excursion in the cubital tunnel after descompression and anterior transposition. J Hand Surg Br. 2000;25(5):457-60.
1. Full Member; MD, plastic surgeon at the Sarah Brasilia Hospital, Brasilia, DF, Brazil.
2. Full Member; MD, plastic surgeon at the Sarah Brasilia Hospital, Brasilia, DF, Brazil.
3. PhD in Orthopaedics, Head Surgeon of the Sarah Network of Hospitals, Brasilia, DF, Brazil.
Corresponding author:
Kátia Torres Batista
SMHS Qd 501, cjto A
Brasília, DF, Brasil - CEP 70335-901
E-mail: katiatb@terra.com.br
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: January 3, 2011
Accepted: February 15, 2011
This work was performed at the Rede Sarah de Hospitais - (Sarah Network of Hospitals), Brasilia, DF, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter