

Original Article - Year 2011 - Volume 26 -
Gluteoplasty augmentation: the importance of teaching of training residents to meet increasing demand
Gluteoplastia de aumento: a importância do ensino na formação atual do residente frente à demanda crescente
ABSTRACT
Introduction: With the increasing demand for buttock augmentation with implants in recent years, it is important to have trained professionals who can perform this procedure and the associated liposuction/fat grafting to improve the hip contour of patients. Methods: In order to determine whether residency is the appropriate environment for practical learning of buttock augmentation with implants, we studied 20 cases treated by training resident practitioners under supervision. Results: Improved buttock contour was achieved in all patients. In addition, we observed a low complication rate, and 100% of the patients reported a high level of satisfaction. These results are consistent with the literature. A major challenge in learning this procedure is blind intramuscular detachment. The residents were carefully supervised and guided by precise anatomical and technical parameters. This enabled them to perform the surgery in the appropriate intramuscular plane, combining liposuction and fat grafting in some cases, resulting in excellent implant coverage and a natural hip contour. Conclusion: The study demonstrated the wide applicability of practical learning of buttock augmentation with implants among residents. We propose that it is necessary that practitioners have complete training in order to meet the current growing demand for buttock augmentation with implants.
Keywords: Buttocks/surgery. Prosthesis Implantation. Prostheses and Implants. Lipectomy.
RESUMO
Introdução: Frente ao aumento na demanda por gluteoplastia de aumento com implantes nos últimos anos, é importante que haja profissionais treinados e capacitados para realizar tal procedimento e suas associações com lipoaspiração/lipoenxertia, com o intuito final de melhorar o contorno do quadril. Método: Ao ver na residência médica o local de ensino apropriado para tal prática, elaboramos o estudo de 20 casos tratados por médicos residentes em treinamento sob supervisão, a fim de observar a aplicabilidade e exequibilidade do método e seus resultados. Resultados: Alcançamos melhoria do contorno glúteo em todos pacientes, o que foi corroborado pelo nível de satisfação elevado de 100% delas e pequena taxa de complicações, compatíveis com a literatura. Há certo receio no início do aprendizado, devido ao descolamento intramuscular às cegas, mas guiados por parâmetros técnicos e anatômicos precisos e sob supervisão qualificada, conseguiu-se a realização da cirurgia no plano intramuscular adequado, associando a lipoaspiração e lipoenxertia em alguns casos, o que proporcionou ótima cobertura do implante e resultados naturais no contorno final do quadril. Conclusão: O estudo demonstrou a grande aplicabilidade do ensino da gluteoplastia de aumento com implantes ao residente em formação, visto a necessidade de uma formação adequada, completa e segura, para atender à crescente demanda por implantes glúteos observada no mercado atual.
Palavras-chave: Nádegas/cirurgia. Implante de Prótese. Próteses e Implantes. Lipectomia.
Buttock augmentation has become the most requested surgery in recent years in Brazil. Data from the Brazilian Society of Plastic Surgery estimated that, since 2008, the number of procedures has increased by 20%.
The use of implants to augment the gluteal region has presented some interesting choices for the treatment of moderate and severe atrophy of this region1-4. Current techniques, which achieve better results and have considerably reduced complications, have made this surgical procedure a satisfactory option to improve body contour5-8. The technical improvements in these operations have increased the safety of liposuction and associated grafting9-12.
Considering the importance of and growth in demand for this surgery over the past years13, we assessed the practical learning of buttock augmentation among resident practitioners at a public hospital under the supervision of senior specialists. We also assessed the results and complications associated with this procedure.
METHODS
This prospective study evaluated 20 patients undergoing buttock augmentation with silicone prostheses between May and October 2010. These patients were treated by residents of the plastic surgery department.
The XYZ technique, described by Gonzalez14, was used to establish anatomical parameters to determine the ideal plane of detachment within the maximum gluteus muscle.
The procedure started with a straight incision, 7 cm in length was made from the highest point of the intergluteal crease, leaving the dermal island above the sacrocutaneous ligament in 5 cases. The next incision was 7 cm in length, with subcutaneous detachment in an an inverted heart shape. The incision was centered in the intergluteal incision and extended laterally at 45º. The second incision was performed 2 cm from the sacral insertion, followed by blunt dilatation with curved scissors in the direction of the fibers of the gluteus maximus muscle in 6 cm long and 3-5 cm deep, in order to allow the detacher passage. This procedure created space with an appropriate dissector at the intramuscular plane, exactly the size of the implant, as a projection of the previous demarcation on the skin, as recommended by Gonzales14. Prior to dissector removal, retractors were introduced. Compresses with adrenaline solution were placed, and the surgical procedure was repeated on the contralateral side. Following completion of the procedure on the contralateral side, we returned to the first side for hemostasis review without an optical fiber aid. Implants were then inserted and accommodated.
Thirteen pairs of round implants and 7 pairs of oval implants were used. The muscle suture was performed using 3.0 Vicryl thread with simple sutures, encompassing both edges of the muscle, and the suture knots were made only after the implant inclusion. The subcutaneous layer of the detached area was sutured with adhesive sutures tied to the deep fascia with 3.0 Vicryl. To recreate the intergluteal fold and decrease the incision tension, we performed skin synthesis with subdermal sutures on both sides of the intergluteal incision, anchored below the skin island in the sacrocutaneous ligament. The skin was sutured using mononylon 4.0.
Depending on requirement, liposuction in the sacral region, flanks, and outer thighs was performed to harmonize the surrounding areas with the increased region. Liposuction was not performed in all cases. The liposuction fat was used for fat grafting of the trochanteric depression in cases in which it was required.
No drains were used. Antibiotic prophylaxis was performed with 2 gm of Kefzol preoperatively and cephalexin for 7 days postoperatively. The patients were instructed to deambulate early and sleep on their side or stomach for 10 days. Surgical wound care involved bathing with anti-germ solution after urination or excretion, changing the dressing after cleaning with 70% alcohol, and applying a micropore tape linking one buttock to the other. Patients are currently in the eight month of follow-up.
RESULTS
Twenty patients were assessed (women, 19; men, 1). The mean age was 33.9 years (range, 22 to 60 years).
The average implant volume was 307 ml (range, 270 to 350 ml; 7 and 13 pairs of oval and round implants, respectively). Associated liposuction was performed in 6 patients (30%) and fat grafting in 4 patients (20%). Lipodystrophy correction with prosthesis for HIV patients was performed in 1 patient, who had experienced changes in lipid metabolism secondary to treatment with antiretroviral drugs15.
The observed complications were 4 cases of seroma formation, 3 cases of partial skin dehiscence, and 1 case of total dehiscence treated with local collagenase dressing and healing by secondary intention. In 1 case, coagulated hematoma developed on the eighth postoperative day, which necessitated a new surgical procedure for cleaning, hemostasis, and replacement of the implant; the outcome was good.
Figures 1 to 10 illustrate the treatments and outcomes for selected patients.
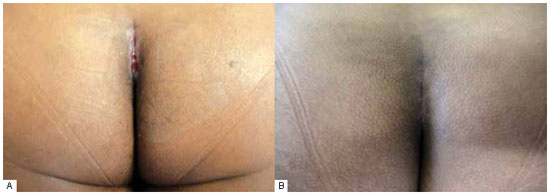
Figure 1 - A: Total dehiscence of the skin treated with local dressing. B: Final appearance of the scar. Patient
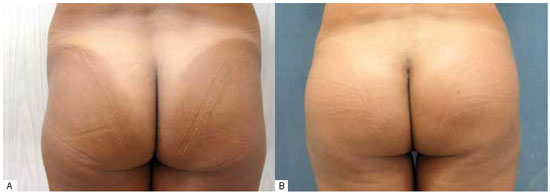
Figure 2 - A: Accentuated trochanteric depression and lipodystrophy of the flanks. B: Postoperative period of 3 months: a 300-ml round gluteal implant and trochanteric fat grafting.

Figure 3 - A: Preoperative aspect, left posterior oblique view. B: Postoperative period of 3 months.

Figure 4 - A: Moderate gluteal atrophy with lipodystrophy of the flanks and trochanteric depression. B: Postoperative period of 4 months: a 300-ml oval gluteal implant and liposuction of the flanks with trochanteric depression fat grafting.
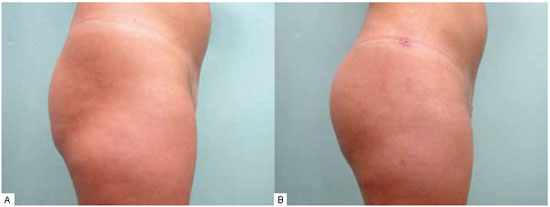
Figure 5 - A: Preoperative, profile view. B: Postoperative, profile view.
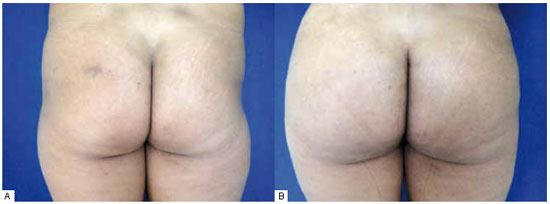
Figure 6 - A: Accentuated trochanteric depression and lipodystrophy of outer thighs and flanks. B: Appearance at 60 days postoperatively after liposuction and fat grafting associated with oblique positioning of an oval gluteal prosthesis implant of 350 ml.
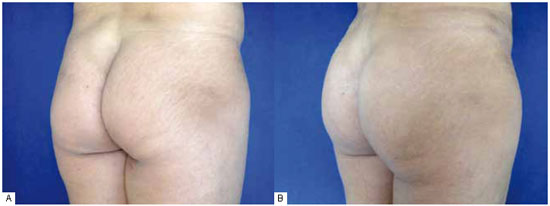
Figure 7 - A: Preoperative right posterior oblique. B: Postoperative period of 3 months.
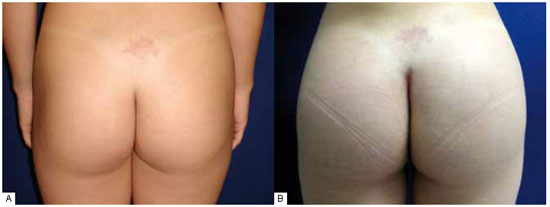
Figure 8 - A: Discrete trochanteric depression with moderate gluteal atrophy. B: An oval prosthesis of 350 ml inserted at angle of 45º to the body midline, with the oblique edge slightly downwards, to fill the mild trochanteric depression.
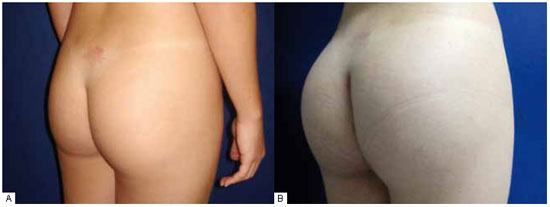
Figure 9 - A: Preoperative period: moderate atrophy of the gluteus. B: Postoperative period of 3 months with satisfactory results only with the gluteal implant.

Figure 10 - A: Preoperative, profile view. B: Postoperative, profile view.
DISCUSSION
We observed that the hesitation while performing blind intramuscular detachment can sometimes inhibit early learning in residents practicing gluteoplasty augmentation. However, guided by precise anatomical and technical parameters and under qualified supervision, the residents were able to perform the surgery in the appropriate intramuscular plane in all cases, which resulted in optimum coverage of the implant and natural results.
The combination of liposuction of flanks and outer thighs with buttock implants improved body contour by correcting sacral lipodystrophy in 30% of the cases, resulting in harmonization between the hip and waist. In 3 cases in which trochanteric depression was accentuated, we placed the oval and oblique implants, at an inclination of 45º in relation to the body midline, with the largest portion of the implant in the upper part and the smallest in the lower part filling the lateral depression. Even in these 3 cases, we obtained remarkable improvement in the trochanteric contour with the new gluteal projection set by the implant with fat grafting in the depression after prosthesis inclusion.
The search for better results raised the possibility of combining these techniques, since the correction of lipodystrophy not only involves the removal of adipose tissue, but also the inclusion of volumes in certain regions. There are few reports on the combination of these techniques in the literature, and surgeons choose, in most cases, to perform only one of the procedures. Correct diagnosis and technical expertise will lead to appropriate treatment of these deformities12.
The coagulated hematoma that developed on the eighth postoperative day in one of the cases was probably attributable to patient non-compliance with prescribed rest. This assumption was corroborated by the patient's information. However, the case had a good outcome.
According to Gonzales7, dehiscence followed by seroma formation is more common than isolated dehiscence. The 3 cases of dehiscence that we observed occurred after seroma formation. It is interesting to note that in all these patients the skin island was left. We emphasize the need for greater care in the preparation of this dermal pedicle so that ischemia does not occur and isolate both sides of placement. It is also important to avoid suture tension. These aspects must be strictly observed when the intention is to leave the dermal island.
It is worth noting that repairing both muscle edges with suture knots using Vicryl 3.0 prior to implant placement made closing the muscle space easier and safer, and reduced the risk of perforating implants with sutures. All patients were satisfied, including those that developed complications, which shows that the residents carried out technique application and postoperative follow-up adequately.
Most patients complained of pain, especially in the first postoperative week, which reduced over time after the surgery as the implant was accommodated.
CONCLUSION
The results demonstrate the wide applicability of practical learning of buttock augmentation as well as the safety of associating this procedure with liposuction of the satellite areas of the buttock. Furthermore, we show that cautious fat grafting of the trochanteric depression in selected cases enhances the aesthetic result of the gluteus prosthesis and provides excellent improvement in body contour. The rates of complication and resolution are acceptable and comparable to those in the literature.
We know that this surgery is not performed and taught in practice at many plastic surgery residency services in Brazil. Thus, it is worth emphasizing the importance of increasing and encouraging practical learning of buttock augmentation with implants for future residents. This learning is especially important, given the observed increase in demand and the need for safety and technical precision. Undoubtedly, such systematic training will enhance the quality of our specialty.
REFERENCES
1. Souza Pinto EB. Novos conceitos em lipoenxertia. Lipoaspiração superficial. Rio de Janeiro:Revinter;1999. p.97-101.
2. Gonzalez R. Prótese para a região glútea. In: Tournieux A, ed. Atualização em cirurgia plástica. São Paulo: Robe Editorial;1994. p.555-70.
3. Pereira LH, Radwanski HN. Fat grafting of the buttocks and lower limbs. Aesthetic Plast Surg. 1996;20(5):409-16.
4. Perén PA, Gómez JB, Guerrerosantos J, Salazar CA. Gluteus augmentation with fat grafting. Aesthetic Plast Surg. 2000;24(6):412-7.
5. Robles JM, Tagliapietra JC, Grandi M. Gluteoplastia de aumento: implante submuscular. Cir Plast Iberolat. 1984;10(4):365-9.
6. Vergara R, Marcos M. Intramuscular gluteal implants. Aesthetic Plast Surg. 1996;20(3):259-62.
7. Gonzalez R. Augmentation gluteoplasty: the XYZ method. Aesthetic Plast Surg. 2004;28(6):417-25.
8. Martins LC. Plastic surgery: foundations and art. São Paulo:MEDSI;2003. p.755-65.
9. Cardenas Restrepo JC, Muñoz Ahmed JA. Large-volume lipoinjection for gluteal augmentation. Aesthetic Surg J. 2002;22(1):33-8.
10. Murillo WL. Buttock augmentation: case studies of fat injection monitored by magnetic resonance imaging. Plast Reconstr Surg. 2004;114(6):1606-14.
11. Roberts TL 3rd, Toledo LS, Badin AZ. Augmentation of the buttocks by micro fat grafting. Aesthetic Surg J. 2001;21(4):311-9.
12. Cárdenas-Camarena L, Paillet JC. Combined gluteoplasty: liposuction and gluteal implants. Plast Reconstr Surg. 2007;119(3):1067-74.
13. de la Peña JA, Rubio OV, Cano JP, Cedillo MC, Garcés MT. History of gluteal augmentation. Clin Plast Surg. 2006;33(3):307-19.
14. Gonzalez R. Buttocks reshaping: posterior contour surgery. A step-by-step approach. Rio de Janeiro:Indexa;2006.
15. Moreno S, Miralles C, Negredo E, Domingo P, Estrada V, Gutiérrez F, et al. Disorders of body fat distribution in HIV-1-infected patients. AIDS Rev. 2009;11(3):126-34.
1. Practitioner aspiring member of the Brazilian Society of Plastic Surgery; 3rd year Resident Physician of Plastic Surgery at Hospital dos Servidores of the State of Rio de Janeiro, RJ, Brazil.
2. Resident Physician in the 2nd year of Plastic Surgery at Hospital dos Servidores of the State of Rio de Janeiro, RJ, Brazil.
3. Resident Physician in the 1st year of Plastic Surgery at Hospital dos Servidores of the State of Rio de Janeiro, RJ, Brazil.
4. Full member of the Brazilian Society of Plastic Surgery; Member of the medical staff at Hospital dos Servidores of the State of Rio de Janeiro, RJ, Brazil.
5. Full Member of the Brazilian Society of Plastic Surgery, Head of Plastic Surgery at Hospital dos Servidores of the State of Rio de Janeiro, RJ, Brazil.
Corresponding author:
Diogo Almeida Lima
Rua Marques de Abrantes, 95/801 - Flamengo
Rio de Janeiro, RJ, Brazil - CEP 22230-060
E-mail: drdiogolima@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: January 30, 2011
Accepted: March 15, 2011
Work performed at the Serviço de Cirurgia Plástica do Hospital dos Servidores do Estado do Rio de Janeiro - (Plastic Surgery Service of Hospital dos Servidores of the State of Rio de Janeiro), Rio de Janeiro, RJ, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter