

Original Article - Year 2011 - Volume 26 -
Geometric analysis of the shapes of beautiful breasts and breast implants based on the golden ratio (Phi): practical application
Análise geométrica da forma da beleza da mama e da forma de prótese baseado na proporção Phi: aplicação prática
ABSTRACT
Introduction: The use of conventional prostheses for hypomastia often yields unsatisfactory and inconsistent results in the final form of the breasts. Considering the number of reported studies on breast and breast-prosthesis forms is negligible, the aim of this study was to optimize the shape results of breast implants on the basis of the Phi ratio, historically known as the golden or divine ratio. Methods: The Phi ratio (1/1.618...) is believed to be registered in the human limbic system as the value of beauty, harmony, and balance of proportions. The three-dimensional anatomy (front, lateral, and vertical views) of beautifully shaped breasts was analyzed geometrically on the basis of the Phi ratio. The various forms of hypomastia were classified. Further, two new forms of polyurethane-covered breast implants were fabricated on the basis of the Phi ratio. The prostheses were chosen by means of vertical measurement of the patient's chest in the frontal view and the hypomastia classification. Results: Ten pairs of prostheses were specially fabricated and implanted in 10 patients. Follow-up for 12 months showed good results for the breast shapes and volumes. Conclusion: Geometric and three-dimensional analysis of beautiful breast shapes and fabrication of breast prostheses based on the Phi ratio are possible to correct hypomastia. In addition to the simple choice of prostheses, the methods provide good and homogeneous results of breast shapes and volumes, reducing subjectivity.
Keywords: Breast Implantation. Prostheses and Implants. Breast/surgery.
RESUMO
Introdução: Os autores observaram resultados insatisfatórios e inconstantes na forma final de mamas após inclusão de próteses de formatos convencionais em casos de hipomastias, havendo poucos estudos a respeito de formas de mamas e de próteses. Método: Descrevem a proporção Phi (1/1.618...), historicamente conhecida como proporção áurea ou divina, e seus conceitos. Argumentam sua importância nas formas em geral, registrada no sistema límbico humano como valor de beleza, harmonia e equilíbrio de proporções. Propõem uma anatomia da beleza da forma da mama em visão tridimensional (visão frontal, lateral e vertical), geometrizada e baseada em Phi. Classificam as mamas quanto à forma incluindo as diferentes formas de hipomastias. Propõem nova forma de prótese mamária, contendo a proporção Phi e coberta com poliuretano. Escolhem as próteses a serem utilizadas por meio de uma medida vertical do tórax da paciente em visão frontal, e da classificação das hipomastias. Resultados: Dez pares de próteses foram especialmente confeccionados e implantados em dez pacientes que foram acompanhadas por 12 meses, apresentando bons resultados finais de forma e volume. Conclusão: É possível estabelecer visão geométrica e tridimensional das mamas bonitas quanto à forma, baseada na proporção Phi, e próteses com a forma também confeccionadas sob a mesma proporção para corrigir as hipomastias. Além de maneira simples de escolha das próteses, o método proporciona a obtenção de resultados bons e homogêneos de formas e volumes mamários, reduzindo subjetividade.
Palavras-chave: Implante Mamário. Próteses e Implantes. Mama/cirurgia.
In addition to their basic function of lactation, breasts have been analyzed from a sexual and esthetic perspective over the centuries. Their exposure and prudish guard have also been going through cultural phases in different parts of the world. It has gathered features never known before, from silicone prosthesis development to resolution of shape and volume problems in a high percentage of women dissatisfied with the disproportions of their breasts.
In plastic surgery, the receptivity of these procedures has never stopped increasing because of the cost and benefits they provide.
The diversity of breast shape and volume, related to genetics, pregnancy, body weight change, and glandular-adipose structures, has continually motivated patients to seek surgery for proper esthetic correction.
Over the decades, breast surgery has evolved into a large collection of techniques, and not a single one can be applied in all cases.
Sometimes, the breasts do not have a beautiful shape and their volumes are insufficient, and therefore, breast implants are needed and requested. Volume, shape, and ptosis have different diagnoses and must be corrected individually via breast implants. At present, patients indicate unsatisfactory shape results after breast augmentation, such as the absence of the upper pole, common in thin patients. The upper pole remains empty after prosthesis implantation and the plastic surgeon cannot improve the breast shape when the prosthesis shape is inadequate.
Historically, there are not many publications containing sufficient information about the shapes of breast prostheses. They have been discussed only by Vázquez1. Other authors have studied prosthesis profiles2,3 or their anatomical profiles4,5. Understanding breast and prosthesis shapes is important to obtain good final results, which are admired by observers. The results of breast augmentation depend on the breast volume and shape as well as the prosthesis volume and shape. In breast reconstruction, the final shape and volume depend only on the breast prosthesis used.
What are the causes of ugly or beautifully shaped breasts? For this, it is necessary to understand the features of beautiful breasts. Further, how can the plastic surgeon identify beautiful anatomical shapes of the breasts and reproduce them in breast implants? Unfortunately, studies of breast-prosthesis shapes have been the priority only in the beauty industry, with few scientific suggestions by surgeons.
If a standard of beauty for breast shape is established, it can be reproduced in breast implants of any volume to avoid bad esthetic results.
The aim of this study was to optimize the shape results of breast implants by analyzing the following:
Breast shapes from a three-dimensional, geometric perspective on the basis of the Phi ratio, establishing the ideal anatomy of beautifully shaped breasts; Different forms of hypomastia; A new shape of breast prosthesis on the basis of the Phi ratio.
In addition to the criteria currently used by specialists, this paper introduces a practical and academic supporting element - the Phi ratio, which is mathematically reproducible - for obtaining esthetic results.
The Phi ratio: history, current concepts, and its importance for shape
Human reactions to beauty and esthetics have been built since the prehistoric period against the adaptive pressures of natural selection6. Humans react instinctively, a phenomenon termed "archetype" in Jungian psychology7. Geometric shapes can be recognized by brain circuits molded by the action of natural selection in the human brain8,9, and which act as a prior mechanism of discipline10.
From antiquity to the present day, only a mathematical ratio is repeatedly mentioned as being contained in generally beautiful shapes: the Phi ratio (1/1.6180339887...; Figure 1). It has always existed in the fields of physics and mathematics. The moment when the Phi ratio was first described or applied is unknown. The Greek mathematicians and philosophers Plato, Aristotle, Pythagoras, and Euclid studied11-16 and observed that creations containing this ratio show harmony6 and beauty. The Egyptians used the Phi ratio in constructing the pyramids15. Phidias used it a lot, including in the Parthenon. Therefore, in the early twentieth century, it was called Phi by the American mathematician Mark Barr: the first part of the name of the Greek sculptor and architect Phidias10.
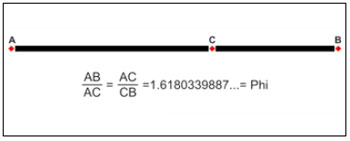
Figure 1 - The Phi ratio (1/1.6180339887...), also called the golden or divine ratio, as a mathematical beauty factor in many areas of knowledge and which touches the human senses.
The Phi ratio was also described by Leonardo of Pisa (Fibonacci), who referred to it in his mathematical sequence. Leonardo da Vinci called it the golden ratio and used it for the Vitruvian Man. Kepler called it divine. Paccioli called it the divine ratio8,9,16. Botanists find it in phyllotaxis17. The Phi ratio is also observable in classical music scores12. The Phi ratio is believed to be registered in the human limbic system as the value of efficiency, beauty, harmony, and balance10. It is an instinctively recognized, esthetic heritage of the human evolutionary process. Since da Vinci, studies of the shapes of the face7,17,18 and also psychology16,19 have been developed on human preferences for structures containing this ratio.
Three geometric shapes based on the Phi ratio were selected to serve as models in the geometric and esthetic study of breasts:
Golden ovoid (Figure 2): The "golden ovoid" is the projection on a single plane of an ovoid consisting of two partially overlapping circles, irrespective of their size. When the Phi ratio (1/1.618) is applied to its vertical axis, as in Figure 2A (AD is to BD as BD is to DC), the same shape is always obtained;
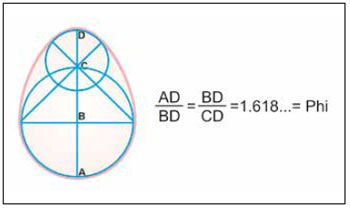
Figure 2 - The golden ovoid with the Phi ratio proposed as a basis for analyzing breast implants.
Golden isosceles triangle: This shape has been thus recognized throughout the Phi history (Figure 3). Its sequential subdivisions maintain the same shape and angles infinitely;
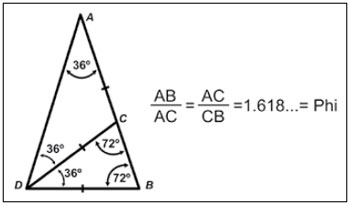
Figure 3 - The golden triangle with the Phi proportion proposed for profile analysis of beautifully shaped breasts.
Golden pyramid (Figure 4A): Four golden triangles joined by their closest sides and apexes form the "golden pyramid." When it is turned on the vertical axis, it forms the "golden cone" (Figure 4B).
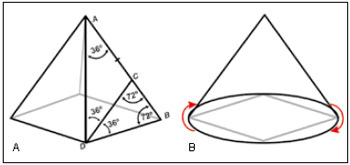
Figure 4 - A: Four golden triangles with the Phi ratio joined from the apex to the base result in the golden pyramid; B: The pyramid turned on its vertical axis, for breast projection analysis, results in the golden cone.
The ovoid was applied to the frontal view of the breast and prostheses bases, the triangle in the lateral view, and the cone in the vertical view.
METHODS
Ratio and anatomy of beautiful breast shape
Beautiful breast shape can be analyzed three-dimensionally (frontal, lateral, and vertical views), where possible esthetic distortions are reflected in each view.
Frontal view: Considering the breast to be shaped as an irregular cone, its horizontal diameter is smaller than its vertical diameter, in the ratio of 1:1.3. This ratio is the result of Phi application to the vertical axis (Figure 5A), with the golden ovoid shape. The ABCD axis is the breast meridian line (BML) and is between two other horizontal lines. The lowest horizontal breast line (LHBL) joins the inframammary crease at their confluence with the breast meridians (points I, Figure 5A). The highest horizontal breast line (HHBL) joins the highest part of two anterior axillary creases. The vertical measurement between these two lines varies in each patient and determines the vertical extension of the base of the breast. When the ratio of 1:1.3 is applied the proportion and resulting lateral extension are obtained. In the frontal view of the breast, in the presence of sagging skin and ptosis, the vertical and horizontal axes tend to have reverse proportions, with the vertical diameter reducing and the horizontal diameter increasing, and the neck empties. Points I do not change.
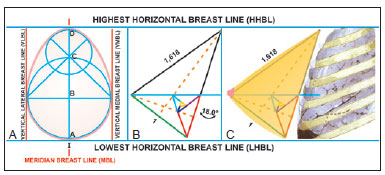
Figure 5 - A: The golden ovoid as the base of a beautifully shaped breast in the frontal view, containing four milk lines that delimit the extent of the base and the position the beautifully shaped breast in the chest; B: Inclination of 18° in the golden triangle is equal to the inclination of the chest in the breast implant area; C: The stylized breast as the golden triangle and inclined at 18° to the chest.
Lateral view: The normal thoracic skeleton, in the anterior sternocostal region, has an inclination of approximately 18º to the vertical axis of the body in the region of breast implants. When the golden triangle is inclined under this angle to the vertical plane, it resembles a beautiful breast in profile (Figures 5B and 5C). In the lateral view, a normal breast without ptosis is located above horizontal plane A (LHBL) (Figures 6A and 6B). Plane A coincides with points I (intersection of the breast meridians with the inframammary crease). Another horizontal plane (M) crosses the breast cone apex and divides the breast into two segments: upper and lower. When it crosses the breast meridians, it determines point M, where the papilla is generally located (it and the areola may be ectopic, out of the cone apex). From the cone apex to points I, the breasts have ideal measurements between 7 and 12 cm. These measurements may vary according to countries, periods, and fashions. Smaller breasts have less volume and projection, and vice versa. Smaller breasts tend to measure 7 cm and larger ones measure 12 cm. The upper segment of the breast cone apex up to the HHBL measures 1.618 times the lower segment measurement, which is the Phi ratio again (Figures 6A and 6B).
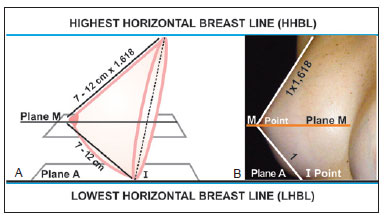
Figure 6 - A: Scheme of the profile view of a breast with beautiful anatomical shape, with the Phi ratio between the lower and the higher pole measurements, and consequently, the others. Plane A passes through points I and plane M passes through the cone apex; B: An anatomically beautiful breast with the same characteristics and geometric proportions as shown in A.
Vertical view: In the vertical view, when the patient looks at herself from top down (Figures 7A and 7B), a normal beautiful breast is located between two vertical lines: the vertical lateral breast line (VLBL) and vertical medial breast line (VMBL). The first coincides with the anterior axillary line and the second is located 1-2 cm laterally to the midsternal line (Figures 7A and 7B). Applying the geometric analysis in the vertical view, the combination of four golden triangles (Figure 4A) by their closest sides and apexes results in the golden pyramid. When the pyramid is turned on its vertical axis, the golden cone is obtained (Figure 4B). It has the ratio of 1:1.618 between its height and its base, and resembles a beautiful breast from the vertical view. If the lines from the base to the apex are curved, it will resemble a beautiful breast from the vertical view (Figure 8).
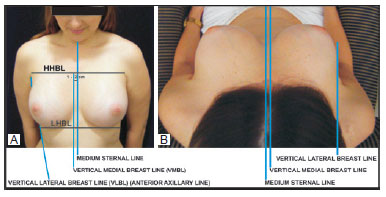
Figure 7 - Vertical view of an anatomically beautiful breast seen by the patient, contained between the HHBL and the LHBL horizontally and between the VLBL and the VMBL vertically.
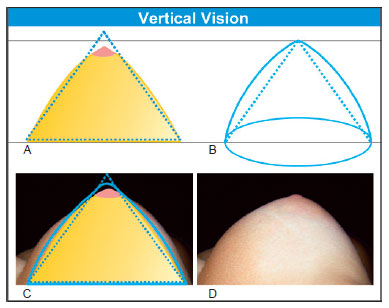
Figure 8 - A: Scheme of an anatomically beautiful vertical view (yellow) over the golden cone (red); B: The golden cone with a slight curvature of the strands, resembling the beautiful breast in Figure 8D; C: Anatomically beautiful breast in the vertical view underneath the schemes; D: Beautifully shaped breast based on the golden cone in the vertical view.
The Phi ratio should not be considered an accurate measurement but serves as a reference and indisputable value to establish an anatomical pattern of beautiful breast shape, which is mathematically reproducible, because the breasts are also beautiful in the ratio of 1:1.5.
The breasts can have a beautiful shape and small volume if the ends of their horizontal and vertical diameters do not touch the horizontal and vertical lines described and established in the chest as their limitations.
Breast-shape diagnosis
During complete clinical assessment of breast esthetic changes, including hypomastia, other elements in addition to the frontal, lateral, and vertical views should be considered. For the breasts, ptosis, volume, axillary extensions, and pectoral extensions must be considered. For the chest, chest anatomy with its vertical and lateral inclinations, curvature of the ribs, and the presence of pectoral muscles must be considered. Further, for the areolar papilla, the position, diameter, projection, shape, and color must be considered. Finally, the symmetry should be observed.
In this study, the authors considered the shape of the breasts and the associated volumes as the basis for implantation in the chest.
The shape of the breast determines its volume. Personal choice, eras, countries, and trends dictate the volume. Volume and shape are different parameters and must be analyzed separately. If the breast contains or approximates the Phi ratio, it is beautiful even though its volume is inadequate.
Breast shapes and their alterations as well as hypomastia and hypertrophy can be assessed according to the frontal, lateral, and vertical views (base and projection of the cone, without ptosis) (Figures 9 and 10):
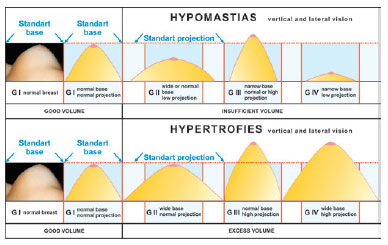
Figure 9 - Classification of breast shapes with hypertrophy, hypomastia, and normomastia. This one is considered anatomically beautiful in the vertical and lateral views, without ptosis regarding shape and volume and touching the horizontal and vertical lines.
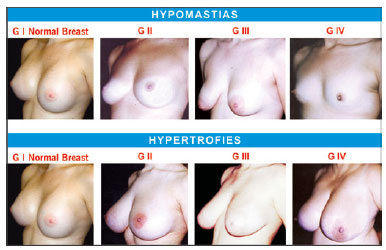
Figure 10 - Photographs of patients with various forms of hypertrophy and hypomastia described in the text and in accordance with the schemes in Figure 9.
Ptosis must be ignored for shape classification. If present, the patient or surgeon should elevate the breast to the ideal position by using an open hand, disregard the ptosis, and proceed with the shape analysis.
Prosthesis fabrication
In this study, two forms of Phi prostheses were developed in two different projections. PhiA forms (high projection) have the anatomical shape of beautiful breasts previously described. In the frontal view, the horizontal and vertical diameters have a ratio of 1:1.3, derived from the Phi ratio between the diameters of two partially overlapping circles (the golden ovoid, Figure 11A). In the lateral view, the ratio of the distance from the apex (M) to the bottom edge (point I) and that from the apex to the upper edge is 1:1.618 (the Phi ratio; the golden triangle, Figure 11B). In the vertical view, the projection and base measurements are in the Phi ratio (1/1.618; the golden cone, Figure 11C). These prostheses are indicated for GII and GIV breasts.
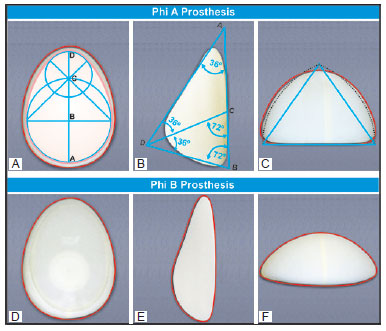
Figures 11 - A-C: Shapes of PhiA prostheses in the frontal, lateral, and vertical views, with the Phi ratio in all of them. They are usable in GII and GIV breasts and breast reconstruction. The straight lines were slightly curved and the apex was removed; D-F: Shapes of PhiB prostheses, with projection reduction in the vertical and lateral views. They are usable in GIII breasts.
PhiB prostheses (low projection) have decreased projection in the vertical and lateral views (Figure 11B) and are indicated for more projected breasts (GIII).
In the frontal view, each half centimeter increase in the vertical stem (AD) of the meridian line of the prosthesis, ranging between 13 and 15 cm, yields prostheses with five different volumes. For example, if the vertical extent of the PhiA prosthesis of 13 cm (280 ml) is changed to 13.5 cm, the volume increases by 50 ml. Accordingly, from 13.5 cm to 14 cm, more than 55 ml is obtained; from 14 cm to 14.5 cm, more than 60 ml is obtained; and from 14.5 cm to 15 cm, more than 65 ml is obtained. Therefore, an increase in the vertical extent from 13 cm to 15 cm results in a volume gain of more than 230 ml (PhiA-15 cm = 510 ml). Silimed, Inc. (Rio de Janeiro, Brazil) manufactured 10 pairs of Phi prostheses for the study: five pairs each of PhiA and PhiB prostheses, with a standby unit of each pair to be used if required during surgery.
Case selection
Ten female patients aged between 20 and 45 years were selected from among the staff of the Hospital de Base, São José do Rio Preto, SP, Brazil. These patients included individuals with GI breasts who wanted more volume; those with GII, GIII, or GIV breasts; and one woman with postmastectomy amastia.
They were operated between October 2008 and May 2009, and followed for 12 months.
Preoperative demarcation and prosthesis choice
With the patient standing, the midsternal line, MBL of each breast, LHBL, and HHBL were marked (Figure 12). Points I (intersection of the MBLs and LHBL) were also marked. The implant for the base of the future breast, to prevent sagging, must be located between the two horizontal lines in the frontal view and the vertical lines VLBL and VMBL. The prostheses were chosen on the basis of (a) the vertical measurement between the midsternal line and the LHBL-HHBL (13.5 cm in the patient in Figure 12) and (b) the hypomastia classification proposed in this study.
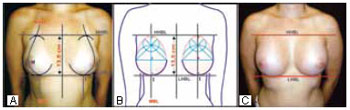
Figure 12 - A: In the frontal view, the choice of prosthesis is based on the patient's vertical measurement between the HHBL and LHBL over the midsternal line. In this patient, the vertical measurement was 13.5 cm; B: Scheme of the same patient and of the chosen prosthesis base of 13.5 cm along the vertical axis, in the frontal view, and within the lines and points described in the text; C: The same patient after the prosthesis placement.
The vertical extent in the patients ranged between 12.5 and 15.5 cm (Figure 12B), but the implants were chosen according to the vertical extent of the prostheses fabricated for this study (between 13 and 15 cm).
For the patients with GIV and GII breasts (low projection), the PhiA prostheses (high projection) were used. For the patients with GIII breasts (high projection), PhiB prostheses (low projection) were employed. The lateral view was enough to observe the mammary projections.
In the case of ptosis, the previously described breast-lift maneuver was performed for breast-shape and projection diagnoses.
Surgery
All the patients were operated under general anesthesia. At the beginning and end of the surgery, 1 g of intravenous hydrocortisone and 10 mg of dexamethasone, respectively, were injected.
Skin incisions and excisions were performed according to need to remove skin excess for correcting ptosis. Axillary incisions were not used. The detachment was performed in the retroglandular position in the lower half of the cavity and under the muscular fascia21 in its upper half, except for the first patient (GII breasts). In this patient, total detachment was performed in the retroglandular position. The cavity base extent was approximately 0.5 cm longer than the prosthesis base extent (Figure 13). The MBL and prosthesis meridian coincided.
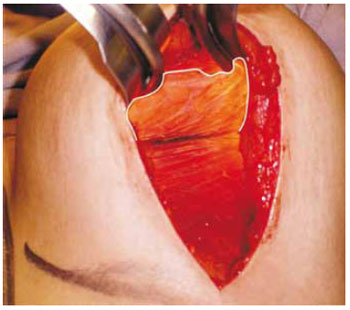
Figure 13 - Cavity prepared to receive the prosthesis under the major pectoralis muscle fascia in the upper half, marked with a white line. The cavity perimeter is 0.5 cm wider than the base perimeter of the prosthesis.
Each prosthesis was washed with saline and placed immediately into a plastic sleeve. It was implanted, and as soon as the glove was removed, it was adjusted to its proper position within the cavity. For difficulties in positioning, an optical fiber valve and a spatula were used to check the position (Figure 14). Before the end of the surgery, a catheter was introduced in each surgical cavity and 30 ml of a solution containing 60 ml saline, 10 mg dexamethasone, 20 ml lidocaine, 1 ml of 1:1000 epinephrine, and 5000 IU hyaluronidase was injected per cavity. The catheters were then removed, and with the aim of spreading the solution, gentle breast massage was performed.
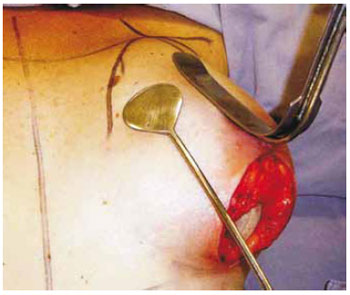
Figure 14 - Optical fiber valve and spatula to check the prosthesis position in the cavity. Vertical excision of skin is shown (same patient as in Figure 18).
RESULTS
The patients did not develop significant postoperative complications. The first operated patient, with GII breasts, was thin and her prosthesis was entirely placed at the retroglandular level. Because her left prosthesis was more evident in the upper edge, she received gentle pressure application on the upper pole of the breasts with a chest belt for 2 months. After this period, the result normalized.
The degrees of patient satisfaction were assessed by survey and they scored grades from 0 to 10 for the results. The arithmetic mean of their scores was 9.9. Other plastic surgeons also rated each outcome by issuing grades from 0 to 10 and the obtained arithmetic mean was 9.0. In the study, the Phi prostheses were considered to yield better shape outcomes than those obtained with the conventional prostheses.
Figures 15 to 21 illustrate cases of the described Phi prosthesis shapes. The patient (GI breasts) in Figure 15 wished to increase her breast size despite the suitable shape and volume for the country she lives in (Brazil). Figure 16 shows the case of a patient with GII breasts. In the case illustrated in Figure 17, conventional prostheses were exchanged with PhiA prostheses and the scars improved. Figure 18 shows the case of a patient with GII breasts. Figure 19 illustrates the case of a patient with GIV breasts after breast pexia 5 years ago; she was dissatisfied with the breast volume and shape. Figures 20 and 21 are from a patient who underwent bilateral breast reconstruction with expander previously included on the right for 90 days and prosthesis replacement in addition to prophylactic adenomastectomy on the left and prosthesis inclusion.
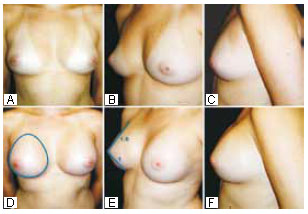
Figure 15 - Same patient as in Figure 12. This patient had GI breasts but wanted more volume. Preoperative and 6-month postoperative photographs are shown, with the Phi ratio established in all the views. The PhiA prostheses measured 13.5 cm along the vertical axis (330 ml). A submammary skin incision was used.
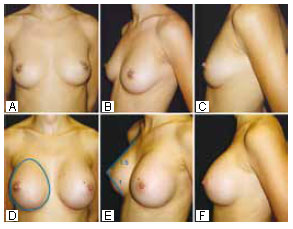
Figure 16 - Preoperative and 12-month postoperative photographs of a patient with GII breasts. The PhiA prostheses measured 13 cm (280 ml) in the vertical measurement of the base, equal to the patient's vertical measurement between the HHBL and the LHBL. A submammary incision was used. All measurements neared the Phi ratio.

Figure 17 - Preoperative and 5-month postoperative photographs of a case of resection of inverted T scars and prosthesis exchange with PhiA prostheses measuring 14.5 cm along the vertical axis (445 ml). Note the Phi ratio approach in the lateral and frontal views.
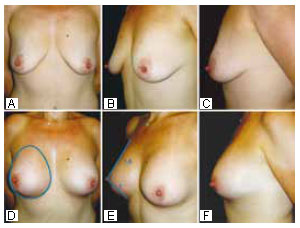
Figure 18 - Preoperative photographs of a patient with GIII breasts and moderate ptosis and 6-month postoperative photographs showing vertical fusiform resection of skin from points I to the papilla. PhiB prostheses measuring 15 cm (435 ml) in the vertical measurement were used, equal to the patient's vertical measurement. The Phi ratio is present.

Figure 19 - Preoperative photographs of a patient with GIV breasts who had undergone mastopexy with L-scars 5 years ago and 10-month postoperative photographs. PhiA prostheses measuring 14 cm (385 ml) were used, equal to the vertical measurement between the LHBL and the HHBL. Further Phi ratios, noting a less beautiful side view.
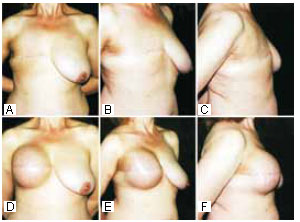
Figure 20 - Photographs of a patient with GIV breasts after (right side) mastectomy with a transverse scar. Reconstruction after expansion and expander exchange with a PhiA prosthesis measuring 14.5 cm (445 ml) were performed. The vertical measurement equals the patient's vertical measurement in the midsternal line between the HHBL and the LHBL. Reconstruction of the papilla and areolar tattooing were also performed. The same transverse incision was used in the left breast for prophylactic adenomastectomy and a PhiA prosthesis measuring 14.5 cm (445 ml) was placed. Areolar-papillary relocation by flaps was performed.
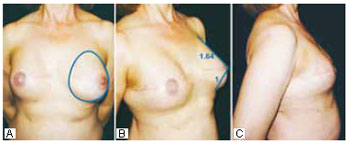
Figure 21 - Postoperative photographs of the patient in Figure 20. The ratios are close to the Phi ratio.
All 10 pairs of PhiA and PhiB prostheses were used. There was no need for additional prostheses.
DISCUSSION
In the frontal view, variation in the vertical measurement of beautifully shaped breasts leads to proportional variations in other measurements, generating different volumes if the Phi ratio is maintained among them. Therefore, by the vertical measurement between the HHBL and the LHBL on the midsternal line and the breast cone projection (GII, GIII, or GIV breasts), PhiA or PhiB prostheses can be selected.
In each patient, the vertical measurement determines the vertical extent of the prosthesis to be chosen and the classification of hypomastia determines the use of PhiA or PhiB prostheses.
The HHBL and LHBL and the VMBL and VLBL are also indicators for choosing the base extension of skin expanders in breast reconstruction:
GI breasts: Patients with these breasts have balanced shape and volume proportions, and do not need correction. However, if they desire more volume, PhiA prostheses are used for higher projection or PhiB prostheses are used for lower projection. The marking is the same; GII breasts: The patients with these breasts have no projection and PhiA prostheses (high projection) are indicated; GIII breasts: The patients with these breasts have adequate breast projection and do not require increased projection. A lower-projection prosthesis (PhiB) is recommended. For such patients, the breast projection can be decreased by a longitudinal incision in the meridian of the mammary gland, causing "collapse" of its lateral and medial segments horizontally. This maneuver can change the current choice of prosthesis profile; GIV breasts and postmastectomy amastia breasts: The patients have little or no breast, so a high-projection prosthesis (PhiA) is indicated. Only this prosthesis will provide beautiful shape and suitable volume, as demonstrated in Figures 20 and 21.
Phi prostheses are filled with silicone slightly harder than the conventional prostheses and coated with polyurethane. Nevertheless, the feeling of a natural breast on palpation is not impaired. Prostheses coated with polyurethane do not move inside their cavities, stick to the bloody tissues as Velcro, and have lower incidence of capsular contracture22.
The polyurethane coating is necessary to prevent prosthesis displacement inside the cavity, preventing deformities. As Phi prostheses are irregular, they do not move inside the cavity. However, studies are necessary to confirm this observation.
The upper portion of the prostheses was placed under the major pectoralis muscle, where it better follows the upper trunk inclination because of the anteroposterior compression exerted by the higher rigidity of the fascia.
Positioning and adjusting the prostheses without folds within the surgical cavity are important because the polyurethane coating sticks to the bloody tissue and does not allow prosthesis movement in the postoperative period. It will not be possible to undo any folds later.
The prostheses cannot be placed with excessive force through small incisions, because permanent deformities may occur in its shape.
The solution injected through catheters at the end of the surgery, containing dexamethasone, lidocaine, epinephrine, and hyaluronidase, reduces pain and swelling in the immediate postoperative period, inflammatory reactions, fibrosis, and the consequent capsular contracture.
For two months postoperatively, the polyurethane-covered prostheses should not be massaged or be involved in trauma, because they may loosen from the bloody tissues and cause hematoma, seroma, fibrosis, and capsular contracture.
Eventually, if the patient wishes larger breasts than those applicable between the described horizontal and vertical lines, the surgeon can increase the vertical extent of the prostheses by increasing the detachment below the inframammary crease (LHBL). On the other hand, if the patient wishes smaller breasts, the detachment should be set above the inframammary crease. The upper detachment does not change in either case.
In the frontal view, if there is ptosis, the horizontal and vertical diameters of the breast base are inverted and the upper pole will be empty. In addition to skin-excess resection, the PhiA and PhiB prostheses are the best options to fill the void neck and invert the diameters to the ideal ratio of 1:1.3.
Many patients are generally satisfied with just breast augmentation and the perception of breasts with ideal and proportional shape is impaired. However, when the patients in the study compared the final shape of their breasts with the outcomes of patients who received conventional prostheses, especially those who had their prostheses exchanged with PhiA and PhiB prostheses (two patients), they demonstrated a higher degree of satisfaction.
The volumes of the Phi prostheses cannot be compared to those of the conventional prostheses. The Phi prosthesis base is more extensive and the volume corresponding to the conventional ones is always greater.
The angles of the golden triangle were naturally abolished for the prosthesis fabrication.
CONCLUSION
On the basis of three-dimensional observations (frontal, lateral, and vertical views) of beautiful breast shape and the Phi ratio, the ideal shape of breast prostheses must contain this ratio. This type of prostheses can be used to correct all cases of hypomastia, including reconstructions, and allows good esthetic results. Their choice is based on the patient's vertical measurement and classification of hypomastia.
REFERENCES
1. Vázquez G. Modificación del implante anatómico de gel de silicona con cubierta de poliuretano. Cir Plást Iberlatinamer. 2005;31(3):193-8.
2. Capozzi A, Pennisi VR. Clinical experience with polyurethane-covered gel-filled mammary prostheses. Plast Reconstr Surg. 1981;68(4):512-20.
3. Eyssen JE, von Werssowetz AJ, Middleton GD. Reconstruction of the breast using polyurethane-coated prostheses. Plast Reconstr Surg. 1984;73(3):415-21.
4. Mira JA. Anatomic asymmetric prostheses: shaping the breast. Aesthet Plast Surg. 2003;27(2):94-9.
5. Fruhstorfer BH, Hodgson EL, Malata CM. Early experience with an anatomical soft cohesive silicone gel prosthesis in cosmetic and reconstructive breast implant surgery. Ann Plast Surg. 2004;53(6):536-42.
6. Peck H, Peck S. A concept of facial esthetics. Angle Orthod. 1970;40(4):284-318.
7. Marquardt SR. Marquardt beauty analysis (web site). Available at: http://www.beautyanalysis.com. Accessed March 15th, 2010.
8. Etcoff NL. Psychology. Beauty and the beholder. Nature. 1994;368(17):186-7.
9. Etcoff NL. A lei do mais belo. Rio de Janeiro:Editora Objetiva;1999.
10. Ricketts RM. The biologic significance of the divine proportion and Fibonacci series. Am J Orthod. 1982;81(5):351-70.
11. Livio M. La proporción áurea, la historia de PHI, el numero más sorprendente del mondo. Barcelona:Editorial Ariel;2005.
12. Brown D. The Da Vinci code. Special Illustrated Edition. GMT Editores; 2004.
13. Eco U. Storia della belleza. Milão:Bompiani;2004.
14. Atalay B. Math and the Mona Lisa, the art and science of Leonardo da Vinci. New York:Harper Collins;2004.
15. Ono E, Walter-Porto COT, Medici-Filho E, Moraes LC, Moraes MEL, Castilho JCM. Análise da proporção áurea em indivíduos dolico, braqui e mesofaciais, por meio de radiografias cefalométricas laterais. Rev Odonto Ciênc. 2007;22(56):154-9.
16. Gil CTLA, Médici Filho E. Estudo da proporção áurea na arquitetura craniofacial de indivíduos adultos com oclusão normal, a partir de telerradiografias axiais, frontais e laterais. Ortodontia. 2002;35(2):69-85.
17. Preston JD. The golden proportion revisited. J Esthet Dent. 1993;5(6):247-51.
18. Bashour M. History and current concepts in the analysis of facial attractiveness. Plast Recontr Surg. 2006;118(3):741-56.
19. Langlois JH, Roggman LA, Casey RJ, Ritter JM, Rieser-Danner LA, Jenkins VY. Infant preferences for attractive faces: rudiments of a stereotype? Developmental Psychology 1987;23(3):363-9.
20. Bozola AR. Breast reduction with short L scar. Plast Reconstr Surg. 1990;85(5):728-38.
21. Graf RM, Bernardes A, Rippel R, Araujo LR, Damasio RC, Auersvald A. Subfascial breast implant: a new procedure. Plast Reconstr Surg. 2003;111(2):904-8.
22. Bozola AR, Bozola AC, Carrazzoni RM. Inclusão de próteses mamárias de silicone-poliuretano. Rev Soc Bras Cir Plast. 2006;21(1):18-22.
1. Professor, PhD in Plastic Surgery, Head of the Plastic Surgery Service of Hospital de Base, Faculdade de Medicina de São José do Rio Preto, São Jose do Rio Preto, SP, Brazil.
2. Plastic Surgeon - Italy.
3. Surgeon dentist, São Jose do Rio Preto, SP, Brazil.
Corresponding author:
Antonio Roberto Bozola
Av. José Munia, 7075
São José do Rio Preto, SP, Brazil - CEP 15085-350
E-mail: ceplastica@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: January 3, 2011
Accepted: February 15, 2011
Work performed at the Serviço de Cirurgia Plástica do Hospital de Base da Faculdade de Medicina de São José do Rio Preto - (Plastic Surgery Service of Hospital de Base, Faculdade de Medicina de São José do Rio Preto), São Jose do Rio Preto, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter