

Original Article - Year 2011 - Volume 26 -
Histopathological findings in tissue specimens from reduction mammaplasties
Achados histopatológicos de produtos de ressecção em mamaplastias redutoras
ABSTRACT
Introduction: Reduction mammaplasty is among the 5 most commonly performed cosmetic surgeries in Brazil. There is no consensus in the literature regarding the need for routine examination of resected tissue obtained during the procedure. This study presents the statistics of specimens obtained from reduction mammaplasty during the last 5 years and discusses the relevance of the histological details of these specimens. Methods: The results of 96 surgical breast reduction specimens from 2006-2010 were obtained from a single institution and analyzed retrospectively. Results: Histopathological changes were observed in 83.3% of specimens. Non-proliferative benign lesions were the main findings; the most frequent were fibrosis, adenosis, and cysts. Proliferative changes were detected in a significant percentage of patients (13.54%). One patient (1.16%), aged 50 years, had lobular carcinoma in situ. Patients younger than 40 years showed no malignant or premalignant lesions. Conclusions: The routine practice of histopathological screening of reduction mammaplasty specimens in young patients seems questionable, although it has been beneficial in patients older than 40 years. Additional studies are needed to define groups for which preventive measures should be undertaken to ascertain the cost-effectiveness of this practice.
Keywords: Mammaplasty. Breast Neoplasms. Histology.
RESUMO
Introdução: A mamoplastia redutora está entre as cinco cirurgias estéticas mais realizadas no Brasil. Não há consenso na literatura sobre a necessidade do exame de rotina dos tecidos ressecados durante o procedimento. Esse trabalho apresenta a estatística dos espécimes obtidos de mamoplastias redutoras e discute a relevância do detalhamento histopatológico dessas peças. Método: Resultados de 96 peças cirúrgicas de reduções mamárias, realizadas durante o período de 2006 a 2010, foram obtidos de uma única instituição e analisados retrospectivamente. Resultados: Alterações histopatológicas foram observadas em 83,3% dos espécimes. As lesões não-proliferativas benignas foram os principais achados, sendo fibrose, adenose e cistos as mais frequentes. Alterações proliferativas foram encontradas em percentual significativo das pacientes (13,54%). Uma paciente (1,16%), com 50 anos de idade, apresentou carcinoma lobular in situ. Pacientes na faixa etária menor que 40 anos não apresentaram lesões malignas ou pré-malignas. Conclusões: A prática rotineira de rastreamento histopatológico de peças de mamoplastias redutoras em pacientes jovens parece discutível, embora tenha sido benéfica em uma paciente com idade superior a 40 anos. Trabalhos adicionais são necessários para definir um grupo em que medidas preventivas teriam melhor relação custo-benefício.
Palavras-chave: Mamoplastia. Neoplasias da Mama. Histologia.
Reduction mammaplasty is among the 5 most commonly performed cosmetic surgeries in Brazil. It is estimated that in 2008, about 55,000 breast reductions were performed in the country1. The main surgical indication is macromastia treatment characterized by increased mammary stroma related to genetic and hormonal factors2,3.
Breast reduction is aimed at obtaining aesthetic and posture balance in patients with macromastia as well as congenital breast asymmetry or symmetrization after contralateral mastectomies3.
The candidates for reduction mammaplasty are subjected to a preoperative screening to detect potentially neoplastic changes3. Although the patients with negative findings during preoperative screening are at a low risk for hidden breast carcinoma, histological analysis of resected tissues has been a common practice for decades4.
There is endless discussion in the literature regarding the need for routine examination of resected tissue during the surgical procedure. The extremely low incidence of neoplastic changes in these specimens and the younger age group undergoing these surgeries are factors that must be considered when questioning the cost-effectiveness of this practice4.
Moreover, about 60% of patients without neoplastic changes in preoperative examinations show benign changes in mammaplasty surgical specimens. Resected tissue analysis could diagnose premalignant proliferative lesions and direct appropriate follow-up of these patients5.
Thus, regional studies should be conducted to profile the incidence of major changes found in given populations and determine the actual importance of analyzing resected specimens in terms of public health.
This paper presents the statistics of specimens obtained from patients who underwent reduction mammaplasty during the past 5 years in our department and discusses some important aspects about the real benefits of detailed histopathology of these specimens by means of a literature review.
METHODS
This quantitative study was performed retrospectively with a descriptive approach at the Department of Plastic Surgery and Microsurgery of the Hospital Universitário Walter Cantídio.
The results of 96 surgical specimens originating from 50 aesthetic reduction mammaplasties between 2006 and 2010 were obtained from histopathological reports archived in medical records and subsequently reviewed.
All studied patients underwent preoperative screening by means of breast ultrasound and mammography. Suspicious malignant lesions were not identified in any patient during preoperative examinations.
Non-neoplastic benign lesions were analyzed individually. The intraductal proliferative lesions were classified as usual ductal hyperplasia, atypical ductal hyperplasia, and ductal carcinoma in situ according to criteria of the World Health Organization (2003)3. Atypical lobular hyperplasia and lobular carcinoma in situ were computed separately.
The data were analyzed using the Statistical Package for Social Sciences (SPSS) version 16.0.
RESULTS
Ninety-six surgical specimens from 50 bilateral breast reductions were studied. For 4 patients, histopathological report of only 1 breast was obtained.
The average age of patients undergoing reduction mammaplasty was 31.88 years, ranging from 15-57 years (SD = 11.45).
Histopathological changes were observed in 83.3% of the specimens. Non-proliferative benign lesions were the main findings, with fibrosis (73.95%), adenosis (52.08%), and cysts (43.75%) being the most common (Table 1).

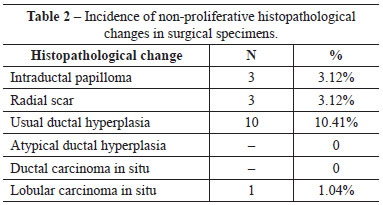
Proliferative changes were found in a significant percentage of patients (13.54%). Intraductal papilloma and radial scarring was noted in 3.12% of the specimens. Usual ductal hyperplasia was found in 10.41% of the specimens, and 50% of these patients were younger than 35 years. Usual ductal hyperplasia and ductal carcinoma in situ were not detected in the studied samples. One (1.16%) 50-year-old patient had lobular carcinoma in situ according to the histological report; after consultation with the Mastology Service, non-surgical management and appropriate follow-up were chosen (Table 2).
DISCUSSION
Several studies demonstrate the occurrence of histological alterations in surgical specimens obtained from reduction mammaplasty. The importance of the microscopic details of the surgical specimens has also been questioned6.
A survey conducted on British doctors in 1994 shows that 89% of surgeons routinely send resected specimens for biopsy; 42% said they found at least 1 case of breast carcinoma in the resected tissues4.
In a different study, occult carcinoma was found in 0.05- 1.66% of specimens from breast reductions; the risk varied depending on the accuracy of pre- and postoperative diagnostic methods4.
In a study with 5,008 specimens, Snyderman and Lizardo7 reported that cancer was detected in 0.4% of cases (0.24- 0.62%); this study included patients with carcinoma detected in the preoperative period. In a similar study of 2,576 specimens, Jansen et al.8 found an incidence of neoplasia of 0.16% (0.04-0.4%). Recently, Tang et al.9 recorded the existence of invasive carcinoma in 0.06% (0.03-0.09%) of 27,500 breast reductions but did not include ductal carcinoma in situ in their results. Other authors describe detailed pathologic findings in surgical specimens, but cancer was not detected in these studies4.
These studies reflect the decrease in occult cancer detection in reduction mammaplasty specimens in recent years, which can be explained by technological advances in early detection methods, greater population awareness, a younger age group of patients undergoing breast surgery, and more complete preoperative screening4.
The study sample indicates that the incidence of occult carcinoma is 1.04%, which is higher than the incidences reported in the above-mentioned studies but consistent with some other published series. The incidence of occult neoplasia was 8.33% in subjects over 40 years of age; no patient younger than 40 presented with carcinoma. It is important to highlight that the diagnosed lesions were not invasive, and some studies did not consider them in the presented case selections.
At present, it is not recommended to perform any form of breast cancer screening, except during clinical examinations, in women younger than 35 years. Despite this, young patients are subjected to histopathological screening after undergoing aesthetic breast surgery, without any clear indication. There are published reports of patients who had findings of uncertain clinical significance and were subjected to years of anxiety and multiple surgical procedures without any proven benefits4.
Some authors describe that part of the difficulty in dealing with patients with histopathological changes is that the specimens are not well geograpgically described during the surgery, making it impossible to accurately determine the affected area. Resection techniques that include the mobilization of tissue distort the mammary architecture during the postoperative period. Therefore, subsequent radiological assessment is not simple, and surgical management is challenging for the mastologist. Although cancer can be detected at the early stages after breast reduction, the affected patients were more likely to undergo a mastectomy than conservative surgery4. Thus, it is evident that careful preoperative screening is essential during preparation for breast surgery.
In this study, a patient had lobular carcinoma in situ and did not require surgical therapy; rigorous and frequent monitoring was recommended for this patient. Thus, the results benefited and alerted the patient to perform surveillance in subsequent years.
Following another line of analysis, according to the literature, about 60% of patients without preoperative changes show benign alterations in surgical specimens from mammaplasties5.
In a study conducted in Brazil, Tafuri and Gobi3 reviewed 867 specimens that originated from bilateral reduction mammaplasty in asymptomatic patients and found that 50.9% had fibrocystic changes and 10.1% had epithelial hyperplasia, which is characterized by premalignant proliferative lesions of the breast that require more frequent follow-up. These data are similar to those published by other authors.
The assessment of proliferative lesions in the studied specimens can individualize patients and help set strategies for preventive measures or monitoring such as the use of prophylactic mastectomy and antiestrogenic therapies3.
Of the case selection in question, 83.3% exhibited histological changes, which were mostly non-proliferative benign changes. It should be noted that specimens that exhibited benign changes during preoperative imaging were not excluded from these statistics. Proliferative lesions such as intraductal papilloma and radial scar each occurred in 3.12% of cases. Usual ductal hyperplasia was observed in 10.41% of the studied specimens. No atypical or premalignant lesions were found.
Some researchers have tried to classify patients into groups of patients at increased risk for developing breast carcinoma after reduction surgery and those that show a higher incidence in the resected tissues.
In another study in Brazil, Souza et al.6 found histopathological changes in 98.63% of 1,018 analyzed specimens and distributed them by age. They also reported findings of 3 premalignant breast lesions; one of them occurred in a patient younger than 35 years (0.25% of 406 patients in the group). No findings of carcinoma were reported in this study.
A Swedish study that also analyzed results by age found an incidence of in situ carcinoma of 8% in specimens from reduction mammaplasty in patients older than 40 years10.
A recent prospective study also indicates a significantly higher rate than that described in the literature. Atypical hyperplasia and carcinomas were found in 12.4% of subjects and only in patients older than 40 years (6.2% in patients aged over 40 years and 7.9% in those aged over 50 years)11.
Cowell et al.2 report that the incidence of cancer in specimens can vary with the type of surgery and stratified their data for macromastia surgeries, congenital asymmetry, and reduced contralateral symmetrization for post-mastectomy patients. Among 800 reductions (611 bilateral and 189 unilateral), the prevalence of cancer was 0.8% (0.28-1.63%), 0.7% in the macromastia group (0.18-1.68%), 0% in the breast asymmetry group, and 1.2% in the contralateral symmetrization group (0.14-4.20%). The group that underwent contralateral breast reduction for reconstruction exhibited a higher risk than the normal population for neoplasia. Note that breast cancer itself is already an important risk factor for contralateral neoplasia.
Thus, according to the literature, in patients over 40 years of age or those who have undergone breast reduction for post-mastectomy symmetrization, histological examination of surgical specimens can provide scientific confirmation. In this study, patients in the contralateral reconstruction group were not assessed.
CONCLUSIONS
The case selection presented here indicates that the incidence of occult carcinoma in the studied institution is similar to that reported in the literature. No cancer or premalignant lesions were detected in the specimens from patients younger than 40 years. The routine practice of histopathological screening of reduction mammaplasties specimens in young patients seems questionable, although it has been beneficial in patients older than 40 years. Additional studies are needed to define groups for which preventive measures should be undertaken to ascertain the cost-effectiveness of this practice.
REFERENCES
1. Pesquisa Datafolha encomendada para Sociedade Brasileira de Cirurgia Plástica. Disponível em:
2. Cowell AS, Kukreja J, Breuing KH, Lester S, Orgill DP. Occult breast carcinoma in reduction mammaplasty specimens: 14-year experience. Plast Reconstr Surg. 2004;113(7):1984-8.
3. Tafuri LSA, Gobbi H. Hiperplasias epiteliais em espécimes de mamoplastia redutora estética bilateral e mamoplastia redutora contralateral a câncer de mama. J Bras Patol Med Lab. 2005;41(2):135-41.
4. Keshtgar M, Hamidian Jahromi A, Davidson T, Escobar P, Mallucci P, Mosahebi A, et al. Tissue screening after breast reduction. BMJ. 2009; 338:b630.
5. Ayhan S, Basterzi Y, Yavuzer R, Latifoglu O, Cenetoglu S, Atabay K, et al. Histologic profiles of breast reduction specimens. Aesthetic Plast Surg. 2002;26(3):203-5.
6. Souza LHG, Oliveira Segundo SWG, Dalul DB, Morais CM, Antunes DE, Pirani F, et al. Estudo histopatológico de 1018 peças cirúrgicas de mamaplastia redutora. Rev Bras Cir Plást. 2005;20(3):173-5.
7. Snyderman RK, Lizardo JG. Statistical study of malignancies found before, during, or after routine breast plastic operations. Plast Reconstr Surg. 1989;25:253-6.
8. Jansen DA, Murphy M, Kind GM, Sands K. Breast cancer in reduction mammaplasty: case report and a survey of plastic surgeons. Plast Reconstr Surg. 1998;101(2):361-4.
9. Tang CL, Brown MH, Levine R, Sloan M, Chong N, Holowaty E. Breast cancer found at the time of breast reduction. Plast Reconstr Surg. 1999;103(6):1682-6.
10. Bondeson L, Linell F, Ringberg A. Breast reductions: what to do with all the tissue specimens? Histopathology. 1985;9(3):281-5.
11. Ambaye AB, MacLennan SE, Goodwin AJ, Suppan T, Naud S, Weaver DL. Carcinoma and atypical hyperplasia in reduction mammaplasty: increased sampling leads to increased detection. A prospective study. Plast Reconstr Surg. 2009;124(5):1386-92.
1. Resident Physician at the Department of Plastic Surgery and Reconstructive Microsurgery at Hospital Universitário Walter Cantídio, Aspiring Member of the Brazilian Society of Plastic Surgery (BSPS), Fortaleza, CE, Brazil.
2. Medical Student at Universidade Federal do Ceará, Fortaleza, CE, Brazil.
3. Plastic Surgeon, Full Member of the BSPS; Head of the Department of Plastic Surgery and Reconstructive Microsurgery of the Walter Cantídio University Hospital of Universidade Federal do Ceará, and from the São Lucas Hospital of Surgery and Anesthesiology, Fortaleza, CE, Brazil.
Corresponding author:
Juliana Régia Furtado Matos
Rua Mombaça, 164 - Aldeota
Fortaleza, CE, Brazil - CEP 60160-190
E-mail: julianarfm@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: November 24, 2010
Accepted: February 6, 2011
Study performed at the Hospital Universitário Walter Cantídio, Universidade Federal do Ceará - (Walter Cantídio University Hospital, Universidade Federal do Ceará), Fortaleza, CE, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter