

Original Article - Year 2011 - Volume 26 -
Use of fibular osteocutaneous flaps in microsurgical reconstruction of complex mandibular defects
Uso do retalho osteocutâneo microcirúrgico de fíbula na reconstrução dos defeitos complexos de mandíbula
ABSTRACT
Introduction: The fibular osteocutaneous free flap is, in most situations, the first choice for reconstruction of segmental defects of the mandible and adjacent soft tissue. Objective: This study presents a four-year experiment with the use of a fibular osteocutaneous free flap for mandibular reconstruction in patients operated upon under the supervision of a single surgeon. Methods: Fifteen patients who underwent microsurgical reconstruction of the mandible and oral floor with a fibular osteocutaneous flap were analyzed. The average postoperative follow-up time was 2 years. Histopathological classification of the primary tumor, location of the resected mandibular portion, vessels used for anastomosis, associated flaps, exposure to radiotherapy, results, and complications were studied. Results: The most common histological type was squamous cell carcinoma (81%) followed by osteosarcoma (13%). The mandibular portion resected with greatest frequency was the central arc (81% of the cases), and 87% of patients received radiotherapy. Reconstruction was immediate in 81% of the patients. Associated flaps were used in 46% of the cases. Immediate complications were observed in 25% of patients and late complications in 31%; the success rate was 100%. Conclusions: The fibular osteocutaneous free flap is indicated for the reconstruction of large mandibular defects. This procedure may present postoperative complications that are significant but do not compromise the success of the procedure, and it must be individualized by taking into account the risks, benefits, and impact on the quality of life of patients.
Keywords: Reconstruction. Microsurgery. Mandible/surgery. Surgical Flaps. Fibula.
RESUMO
Introdução: O retalho livre osteocutâneo de fíbula é a primeira escolha para reconstrução de defeitos segmentares da mandíbula e tecido mole adjacente, na maioria das situações. Objetivo: Este estudo apresenta uma experiência de 4 anos com o uso de retalho osteocutâneo livre de fíbula para reconstrução mandibular. Método: Foi feita análise de 15 pacientes submetidos à reconstrução microcirúrgica de mandíbula e assoalho oral com retalho osteocutâneo de fíbula. O tempo médio de seguimento pós-operatório foi de 2 anos. Foram estudados classificação histopatológica do tumor primário, localização da porção mandibular ressecada, vasos utilizados para anastomose, retalhos associados, exposição à radioterapia, resultados e complicações. Resultados: O tipo histológico mais comum foi o carcinoma espinocelular (81%), seguido do osteossarcoma (13%). A porção mandibular ressecada com maior frequência foi o arco central, em 81% dos casos, e 87% dos pacientes foram expostos à radioterapia. A reconstrução foi imediata em 81% dos pacientes. Retalhos associados foram usados em 46% dos casos. Complicações imediatas foram observadas em 25% dos pacientes e tardias, em 31%, com taxa de sucesso de 100%. Conclusões: O retalho osteocutâneo livre de fíbula está indicado na reconstrução de grandes defeitos mandibulares. Sua indicação deve ser individualizada, levando-se em consideração riscos, benefícios e impacto na qualidade de vida do paciente.
Palavras-chave: Reconstrução. Microcirurgia. Mandíbula/cirurgia. Retalhos Cirúrgicos. Fíbula.
Oncological resection of the mandible has a huge impact on the shape of the lower third of the face and on function; it can severely compromise chewing, speech, and facial aesthetics1. Initial reconstruction attempts with non-vascularized bone grafts and pedicled osteocutaneous flaps were marked by a high incidence of postoperative complications and poor results in the long run2. This changed significantly with the advent of microvascular surgery. The transfer of free flaps for mandibular reconstruction has been well accepted for decades and many donor sites have been documented in the literature3.
The fibular free flap was first described by Taylor in 1975 and Hidalgo described its use for mandibular reconstruction in 1989. Since then, it has become popular in several reconstructive centers4. The inclusion of a safe island of skin from the lateral leg portion as an osteocutaneous flap expanded the application of this procedure for composite mandibular defects, which often require both bone and soft tissue components5. Although many foreign studies have been published on the results of the use of fibular osteocutaneous free flaps in mandibular reconstruction, studies demonstrating the experience of surgeons in Brazil with this type of reconstruction are rare.
The present study assessed a series of patients who underwent complex oromandibular reconstruction, under the supervision of a single surgeon, using a fibular osteocutaneous free flap by itself or in combination with other free and pedicled flaps after major tumor resection at the Instituto Nacional do Câncer-RJ.
METHODS
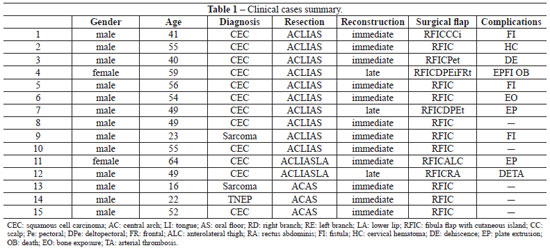
An analysis of 15 patients who underwent microsurgical reconstruction of the mandible and oral floor with a fibular osteocutaneous flap was performed between January 2006 and December 2009 (Table 1).
The average follow-up time after surgery was two years, with one case of death in the late postoperative period.
The following parameters were studied: histopathological classification of the primary tumor, location of the resected mandibular portion, vessels used for anastomosis, associated flaps, exposure to radiotherapy, results, and complications.
RESULTS
Histological classification of the primary tumor revealed 12 (81%) cases of squamous cell carcinoma, 2 (13%) cases of osteosarcoma of the mandible, and 1 (6%) case of primitive neuroectodermal tumor (Figure 1).
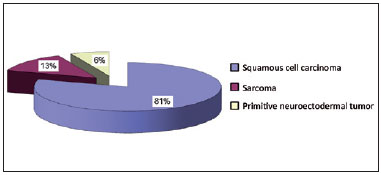
Figure 1 - Types of tumor
In relation to the resected mandibular portion, resection of the central arch was performed in 12 (81%) cases, resection of the central arch with right subtotal mandibulectomy was performed in 2 (13%) cases, and resection of the central arch with left subtotal mandibulectomy in 1 (6%) case (Figure 2).

Figure 2 - Resected mandibular portion.
Reconstruction was immediate in 12 (81%) patients and late in 3 (19%; Figure 3). The most used artery for anastomosis was the facial artery and the most used vein was the tireolinguofacial trunk, both in 53% of the cases (Figure 4).
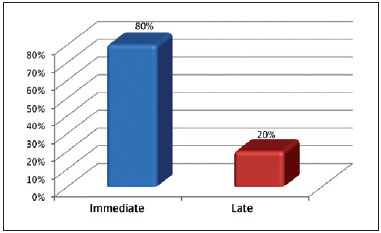
Figure 3 - Timing of the reconstruction.
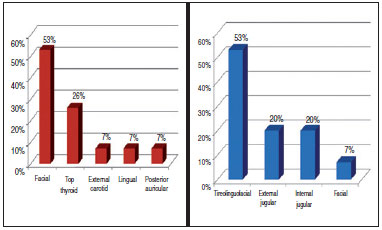
Figure 4 - Receptor vessels.
In some cases, pedicled scalp, deltopectoral, and pectoral associated flaps were used, as well as free rectus abdominis and anterolateral thigh flaps (Figure 5).
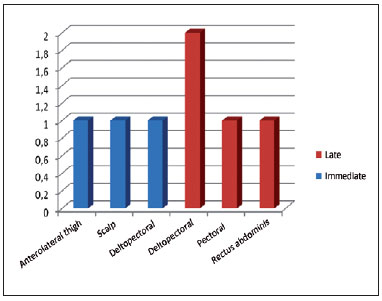
Figure 5 - Associated flaps.
Thirteen (87%) patients underwent radiotherapy, 9 (61%) after surgery and 4 (26%) before surgery (Figure 6).
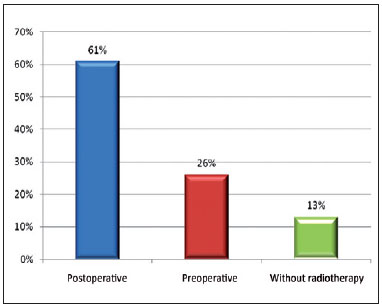
Figure 6 - Patients treated with radiotherapy.
The early complications noted were as follows: 2 cases (13%) of intraoral wound dehiscence, 1 (6%) of cervical hematoma, and 1 (6%) of arterial thrombosis after 48 hours, who underwent surgical revision. The late complications were 3 cases of extrusion and plate removal, 1 case of orocervical fistula, and 1 case of bone exposure. There was one death in the late postoperative period due to pulmonary complications, despite the viability of the microsurgical flap (Figure 7).
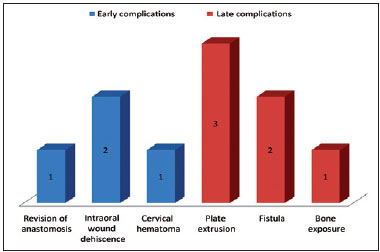
Figure 7 - Early and late complications.
The average postoperative follow-up period was 2 years. In this series of cases, there was no flap loss, despite the complications.
Figures 8 to 11 illustrate some examples of this case selection.

Figure 8 - A: Skin of the cervical-mandibular area superiorly hit back; B: Complex defect after resection of the oral floor, tongue, and the central arch of the jaw; C: Osteocutaneous flap molded to the plate. Its bony portion reforms the mandibular contour and the cutaneous portion the oral floor.
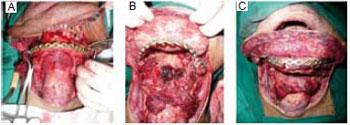
Figure 9 - Preoperative: A: Front view; B: Profile; C: Intraoral view showing a tumor involving the base of the tongue, oral floor, and central arch of the jaw.
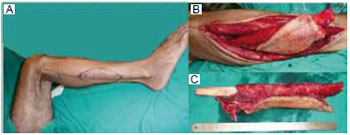
Figure 10 - A: Marking; B: Dissection of the fibular flap with skin island; C: Free flap, ready to be framed by triangular osteotomies.

Figure 11 - Postoperative: A: and B: Front view and profile demonstrating the maintenance of the mandibular contour; C: Intraoral view showing the skin island with early mucous metaplasia.
DISCUSSION
In most comparable studies in the literature, the average age of patients ranges from 40 to 50 years; the average patient age in our study was 45 years (range from 16 to 64 years old)1,3,4. The majority (87%) of our patients were male. Other studies also reported a higher incidence of the procedure being performed in male patients. This may be the result of gender differences in the consumption of alcohol and nicotine, because most of these procedures are performed for the treatment of malignancies1,3,4. Because our facility is an oncological center, our case selection does not include post-trauma reconstruction, as in some studies. Reconstructions were performed to correct defects after tumor resection. The most common histological type was squamous cell carcinoma (81%), which is comparable to other reports in the literature1,3,4.
Using the classification system of Jewer et al.6, the location of the mandibular bone defect in our cases can be defined as LCL (central segment) in 12 patients and LC (central and lateral segment without condyle) in 3 patients. Based on research showing that functional and aesthetic results are more correlated with the extent of the soft tissue defect than with the extent of the bone defect, the classification system has been modified to include an "m" for mucous defects, "s" for skin, and "sm" or "through-and-through" for overall plane defects7. This is relevant when comparing the results obtained in different studies and in guiding the choice of technique to be used in reconstruction5. All of the cases analyzed had defects that involved the bone, skin, and mucosa to varying degrees. The need for additional tissue in some patients led to the combination of pedicled scalp, deltopectoral, and pectoral flaps, as well as microsurgical flaps in two cases (one rectus abdominis and one anterolateral thigh). The success of these associations is consistent with the recent literature and demonstrates that multiple simultaneous free flaps can be used in patients, with acceptable recovery times and good functional results8.
Most patients (61%) who underwent immediate reconstruction of the mandible received postoperative radiotherapy, which, on average, was performed two months after surgery. Some studies have demonstrated that radiotherapy does not seem to delay the consolidation of osteotomy sites and does not compromise bone flap viability1,9. Our case series did not include any cases of osteoradionecrosis of the mandible, which can be prevented through proper oral hygiene, fractionated radiotherapy, and the appropriate timing of radiotherapy initiation1.
Regarding the placement of osteointegrated dental implants, we did not perform the primary procedure because of the need for postoperative radiotherapy2. In our case selection, 33% of the patients had early complications, a rate consistent with that reported in the literature, in which the occurrence of complications was as high as 56%9. Such complications can, in some cases, delay radiotherapy after surgery. Despite inconclusive scientific evidence, it is widely accepted that patients with oral cancer should receive postoperative radiotherapy as soon as possible, preferably within six weeks10.
In this context, complications, though minor, may affect the treatment schedule and should be taken into account. Moreover, minor complications, such as intraoral wound dehiscence - found in two cases in our study - may lead to infection due to contamination by saliva. A cervical hematoma may compress the cervical pedicle and put the flap at risk. Most small fistulae can be conservatively treated with drainage and antibiotics9. Arterial thrombosis occurred within 48 hours and was addressed with anastomosis revision, while maintaining flap viability.
Regarding late complications, there were three cases of extrusion and removal of the plate. We used a single plate of titanium 2.7 because a recent study comparing single plates to miniplates demonstrated that plate selection does not affect complication rates in the reconstruction of the mandible using a fibular free flap, and does not destabilize the reconstruction with failure of consolidation11.
Regarding the timing of surgery, immediate reconstruction was performed in 12 cases and late reconstruction in 3 cases. There were no complications at the donor sites of these patients, and this low incidence of complications at the donor site is also observed in other studies2. Although recent evidence suggests that primary and secondary reconstruction procedures have the same complication rates12, our experience shows that secondary reconstruction is more complex than immediate reconstruction.
Loss of normal anatomy, retraction of structures, fibrosis secondary to surgery, and radiotherapy increase the reconstruction complexity9,13. There was one death in the late postoperative period due to pulmonary complications. This emphasizes the importance of patient assessment; in highly complex and long-duration surgeries, clinical events may impair the patient's recovery. In these cases, the improvement in quality of life as a result of the improvement in the appearance and function of the reconstructed mandible has to be weighed against the potential morbidity of the surgical intervention14.
CONCLUSION
The fibular osteocutaneous free flap remains the chosen procedure for the reconstruction of large mandibular defects, especially the anterior portion of the jaw, after major tumor resection. It may be associated with postoperative complications that are significant but do not compromise the success of the procedure. Its indication must be individualized, taking into account the risks, benefits, and the impact on the quality of life of the patient.
REFERENCES
1. Hidalgo DA, Pusic AL. Free-flap mandibular reconstruction: a 10-year follow-up study. Plast Reconstr Surg. 2002;110(2):438-49.
2. Wallace CG, Chang YM, Tsai CY, Wei FC. Harnessing the potential of the free fibula osteoseptocutaneous flap in mandible reconstruction. Plast Reconstr Surg. 2010;125(1):305-14.
3. Wedler V, Farshad M, Sen M, Koehler C, Hanschin A, Graetz K, et al. Retrospective analysis and clinical evaluation of mandible reconstruction with a free fibula flap. Eur J Plast Surg. 2007;29(6):285-91.
4. Winters HAH, van Loenen DKG. Comparison between fibula and iliac crest in mandibular reconstruction. Eur J Plast Surg. 2007;29(5):205-8.
5. Takushima A, Harii K, Asato H, Momosawa A, Okazaki M, Nakatsuka T. Choise of osseous and osteocutaneous flaps for mandibular reconstruction. Int J Clin Oncol. 2005;10(4):234-42.
6. Jewer DD, Boyd JB, Manktelow RT, Zuker RM, Rosen IB, Gullane PJ, et al. Orofacial and mandibular reconstruction with the iliac crest free flap: a review of 60 cases and a new method of classification. Plast Reconstr Surg. 1989;84(3):391-403.
7. Boyd JB, Gullane PJ, Rotstein LE, Brown DH, Irish JC. Classification of mandibular defects. Plast Reconstr Surg. 1993;92(7):1266-75.
8. Hanasono MM, Weinstock YE, Yu P. Reconstruction of extensive head and neck defects with multiple simultaneous free flaps. Plast Reconstr Surg. 2008;122(6):1739-46.
9. Chaine A, Pitak-Arnnop P, Hivelin M, Dhanuthai K, Bertrand JC, Bertolus C. Postoperative complications of fibular free flaps in mandibular reconstruction: an analysis of 25 consecutive cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;108(4):488-95.
10. Langendijk JA, de Jong MA, Leemans CR, de Bree R, Smeele LE, Doornaert P, et al. Postoperative radiotherapy in squamous cell carcinoma of the oral cavity: the importance of the overall treatment time. Int J Radiat Oncol Biol Phys. 2003;57(3):693-700.
11. Robey AB, Spann ML, McAuliff TM, Meza JL, Hollins RR, Johnson PJ. Comparison of miniplates and reconstruction plates in fibular flap reconstruction of the mandible. Plast Reconstr Surg. 2008;122(6):1733-8.
12. Andrade WN, Lipa JE, Novak CB, Grover H, Bang C, Gilbert RW, et al. Comparison of reconstructive procedures in primary versus secondary mandibular reconstruction. Head Neck. 2008;30(3):341-5.
13. Pohlenz P, Blessmann M, Heiland M, Blake F, Schmelzle R, Li L. Postoperative complications in 202 cases of microvascular head and neck reconstruction. J Craniomaxillofac Surg. 2007;35(6-7):311-5.
14. De Santis G, Pinelli M, Baccarani A, Pedone A, Spaggiari A, Jacob V. Clinical and instrumental evaluation of implant stability after free fibula flaps for jaw reconstruction. Eur J Plast Surg. 2006;29(2):53-66.
1. Resident Physician in the Department of Plastic Surgery and Microsurgery at the Instituto Nacional do Câncer-RJ, Rio de Janeiro, RJ, Brazil.
2. Full Member of the Brazilian Society of Plastic Surgery. Master of Medicine at the Universidade Estadual de Campinas (UNICAMP); Plastic Surgeon at HU-UFRJ. Coordinator of the Residency Program in Plastic Surgery of the Instituto Nacional do Câncer-RJ, Rio de Janeiro, RJ, Brazil.
3. Resident Physician of the Plastic Surgery Department at the Hospital da Força Aérea do Galeão-RJ, Rio de Janeiro, RJ, Brazil.
4. Full Member of the Brazilian Society of Plastic Surgery; Professor at the Universidade Federal do Estado do Rio de Janeiro. Head of the Department of Plastic Surgery and Microsurgery at the Instituto Nacional do Câncer-RJ, Rio de Janeiro, RJ, Brazil.
Corresponding author:
Igor Felix Cardoso
Rua Alecrim lote 6 - bloco A - apto 506 - Stilo Residencial - Águas Claras
Brasília, DF, Brazil - CEP 71938 -720
E-mail: igorfelixcardoso@gmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: November 30, 2010
Accepted: February 22, 2011
Work was performed at the Serviço de Cirurgia Plástica e Microcirurgia do Instituto Nacional do Câncer - INCA/RJ - (Department of Plastic Surgery and Microsurgery at the Instituto Nacional do Câncer-RJ), Rio de Janeiro, RJ, Brazil.
Prize-winning work, Sirlei Rinaldi Award 2010.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter