

Original Article - Year 2011 - Volume 26 -
Anthropometric study of craniofacial asymmetry in unilateral coronal craniosynostosis
Estudo antropométrico das assimetrias craniofaciais na craniossinostose coronal unilateral
ABSTRACT
Introduction: Unilateral coronal craniosynostosis (UCC) is the unilateral premature ossification of the coronal suture, leading to a 3-dimensional deformity that may affect the skull and orbits. Objective: The purpose of this study was to measure and compare the craniofacial asymmetry of patients with UCC in the preoperative and postoperative periods to assess the effectiveness of surgical UCC correction. Methods: Nine patients (4 girls and 5 boys) underwent surgical correction of UCC between January 2007 and December 2010. Their craniofacial dimensions were measured with a goniometer to calculate the craniofacial asymmetry index (CAI) in the preoperative and postoperative periods, and the CAI averages of the periods were compared. The CAI was calculated as the ratio of the craniofacial diagonal measurements of the unaffected side to those of the affected side. Results: The mean patient age was 2 years 1 month. The average surgical time was 2 h 46 min. The average volume of transfused blood was 280 ml. The preoperative and postoperative CAI averages were 1.045 and 1.009, respectively (p=0.0109), indicating a strong tendency for symmetry after the surgery. Conclusion: Surgical UCC correction is effective for achieving craniofacial symmetry. Overcorrection of the bony structures is required to obtain bone symmetry postoperatively.
Keywords: Craniosynostoses. Plagiocephaly. Craniofacial abnormalities.
RESUMO
Introdução: A craniossinostose coronal unilateral (CCU) é a ossificação prematura da sutura coronal unilateralmente e provoca uma deformidade em 3 dimensões, que pode afetar o crânio e as órbitas. O objetivo do presente trabalho foi aferir e comparar a assimetria do crânio e face dos pacientes portadores de CCU no período pré e pós-operatório. Método: Nove pacientes foram submetidos à correção da craniossinostose coronal unilateral, entre janeiro de 2007 a dezembro de 2010. Quatro pacientes foram do sexo feminino e cinco do sexo masculino. Foram aferidas medidas da região craniofacial para quantificar o índice de assimetria craniofacial no período pré-operatório e compará-lo com o período pósoperatório. O índice de assimetria craniofacial (IAC) foi determinado pela diferença entre as medidas craniofaciais diagonais obtidas com o goniômetro. Resultados: A idade média dos pacientes submetidos à correção de CCU foi de 2 anos e 1 mês. O tempo médio de cirurgia foi de 2 horas e 46 minutos. O volume médio de sangue transfundido foi de 280 ml. A média das diferenças das medidas diagonais obtidas com o goniômetro no período pré-operatório (IAC) foi de 1,045 e do pós-operatório de 1,009 (p=0,0109), indicando forte tendência à simetria craniofacial após o ato cirúrgico. Conclusão: O tratamento proposto para as CCU foi eficiente na obtenção de simetria craniofacial. Foi necessária a sobrecorreção das estruturas ósseas para obtenção de simetria óssea no período pós-operatório.
Palavras-chave: Craniossinostoses. Plagiocefalia. Anormalidades craniofaciais.
Craniosynostosis is the premature fusion of one or more sutures of the cranial vault and its associated cranial deformities. The pattern of skull deformities is peculiar to the fused suture (metopic, coronal, sagittal, and lambdoid). Unilateral coronal craniosynostosis (UCC) is the premature fusion of the coronal suture. Its incidence is approximately 1 in 10,000 live births, and it has been described as the second most frequently identified synostosis in specialized centers for the treatment of craniofacial deformities1.
The vast majority of patients with UCC typically present morphological changes of the cranial vault due to a compensatory mechanism of brain growth (Virchow's law), usually toward the open sutures, which causes a 3-dimensional deformity. This situation leads to considerable deviation of the sagittal axis of the skull base, observed during physical examination through the discrepant position of the ears (the affected side is positioned higher and forward), deviation of the nasal root to the affected side, and deviation of the nasal tip to the opposite side. The frontoparietal region ipsilateral to the affected suture is depressed, leading to a compensatory contralateral hump. The eyebrow position is always higher on the affected side. The mentonian region is deviated to the contralateral side. The zygomaticomaxillary region may be more anteriorly positioned in relation to the contralateral side, following the 3-dimensional rotation of the skull base2,3.
The clinical implication of the rotation of the skull base in UCC has been intensely debated, and this rotation is believed to be responsible for all the clinical findings of UCC. As described by Silva-Freitas et al.4, the orbit in Harlequin (elevation of the superolateral corner of the orbit) is a typical sign of UCC, because of the anomalous position of the greater sphenoid wing on the affected side. The premature fusion of the coronal suture may be associated with craniofrontonasal dysplasia5, Saethre-Chotzen syndrome6, and the Pro250-to-Arg mutation in the FGFR3 gene7, also known as the Muenke mutation. The clinical features vary according to the identified genetic mutation and may involve the upper limbs8.
The purpose of the present study was to measure and compare the craniofacial asymmetry of patients with UCC in the preoperative and postoperative periods to assess the effectiveness of surgical UCC correction.
METHODS
Nine patients (4 girls and 5 boys) underwent surgical correction of UCC between January 2007 and December 2010. Their craniofacial dimensions were measured with a goniometer to calculate the craniofacial asymmetry index (CAI) in the preoperative and postoperative periods and the CAI averages of the periods were compared.
The CAI was calculated as the ratio of the craniofacial measurements of the unaffected side to those of the affected side. For example, a preoperative CAI average greater than 1 indicates a larger unaffected side before surgery (Figure 1). All patients included in the analysis were photographed in a standardized photography studio while lying down to obtain photographs in the full frontal, lateral, oblique, and frontobasal views. Patients suffering from syndromic craniofrontonasal dysplasia associated with UCC were excluded.
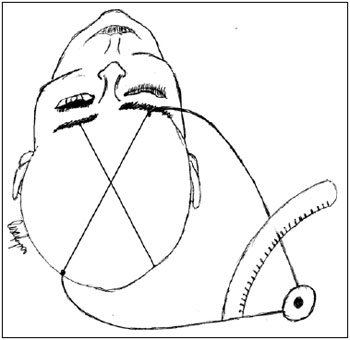
Figure 1 - Delineation of the anatomical dimensions measured with a goniometer in the patients with unilateral coronal craniosynostosis.
Operative Technique
With the patient in the supine position, under general anesthesia, UCC correction was begun with a coronal incision and subgaleal undermining of the frontal flap. Subsequently, a periosteal flap was elevated from the coronal suture level to the orbital roof. The supraorbital neurovascular bundle was carefully identified, elevated, and released from the frontal bone together with the periorbit. With access to the inner orbit, periorbital undermining was performed along the subperiosteal plane.
Craniotomy was performed through the fontanel, providing safe access to the intracranial area. The cranial bone was easily removed and cut with a piecemeal instrument, Jackson scissors, or a reciprocating saw. Cranioplasty was performed on the surgical table. The anterior cranial base was detached at the central and lateral portions, with extensive detachment of the greater sphenoid wing. Osteotomy was performed from the region of the greater sphenoid wing toward the lateral wall of the orbit. The basilar region was decompressed by using a malleable retractor, with appropriate protection of the notable structures.
Fronto-orbital advancement was not performed because the rapid and intense brain growth in the first year of life allows the orbital structures to become symmetrical naturally; this surgery was reserved for older patients with UCC. Children younger than 1 year of age present a favorable combination of flexibility and possibility of large brain expansion during growth of the craniofacial skeleton. This combination enables surgical correction without the use of molding helmets and the need to move the orbital structures.
Suction drains were placed and maintained for 24-48 h. Dressings were used until 12 h after drain removal. The scalp was sutured with 4-0 nylon sutures3.
Statistical Evaluation
Student's t-test was used to compare the preoperative and postoperative CAI averages. P values less than 0.05 were considered significant.
RESULTS
The patients underwent the same surgical technique, with completion of cranioplasty and decompression of the skull base. Decompression of the skull base usually provides enough room for brain growth.
The average patient age was 2 years 1 month. The average surgical time was 2 h 46 min. The average volume of blood transfused was 280 ml.
The preoperative and postoperative CAI averages were 1.045 and 1.009, respectively, showing a significant difference (p=0.0109; Figures 2-6).

Figure 2 - Preoperative photograph of a patient with unilateral coronal craniosynostosis (right). Photograph of the patient 2 years after surgery to correct the craniosynostosis (left). Considerable improvement in the contour of the frontal region and orbital dystopia were observed; the improvement was achieved because of rapid brain expansion, usually occurring in patients undergoing surgery within 6 months of birth.

Figure 3 - Preoperative photograph of a patient with unilateral coronal craniosynostosis, strabismus associated with congenital muscular torticollis, and vertical orbital dystopia who underwent surgery to correct the craniosynostosis at 3 months of age (right). Postoperative photograph of the patient (left). Note the considerable improvement in the contour of the frontal region and orbital dystopia.

Figure 4 - Preoperative photograph of a patient with unilateral coronal craniosynostosis, strabismus associated with congenital muscular torticollis, and vertical orbital dystopia (right). Photograph of the patient after surgery to correct the craniosynostosis (left). Note the considerable improvement in the contour of the frontal region and orbital dystopia.

Figure 5 - Preoperative (right) and postoperative (left) photographs of the same patient (right) from another photographic angle. Note the considerable improvement in the contour of the frontal region.

Figure 6 - Preoperative photograph of a patient with unilateral coronal craniosynostosis who underwent surgery at 3 months of age (right). Postoperative view (left); considerable improvement in the frontoparietal contour can be seen.
DISCUSSION
In the present study, the postoperative CAI average was close to 1, indicating that important cranial symmetry was achieved surgically. Surgery for UCC correction also has direct implications on facial symmetry and positioning of the orbits, and therefore, it should always be performed before 1 year of age. The brain normally doubles in size in the first year of life8. This rapid brain growth acts directly on the repositioning of the craniofacial structures in patients surgically treated for UCC3. The main goal of early surgical intervention is to interrupt the deleterious effects of abnormal suture fusion on the craniofacial skeleton. In addition, craniosynostosis may be associated with increased intracranial pressure, even when only 1 suture is compromised9, and can lead to deficits in the neurocognitive development of the affected child9. The immediate relief of clinical signs of intracranial hypertension by surgery usually allows normal craniofacial development.
The craniofacial skeleton of a child aged 3-5 months is malleable and easy to reshape. The postoperative bone defects undergo reossification due to the osteogenic potential of the dura mater and periosteum in patients under 1 year of age10. Therefore, early surgery has considerable benefits. The mean age of the patients who underwent surgical UCC correction in this study was 25 months; 2 patients aged 3 years accounted for the increase in mean age. The remaining 7 patients were operated on before 1 year of age. Preferably, patients should be operated on at around 4 months of age. However, many patients are referred to the hospital when they are older, mainly because of the lack of early diagnosis. The unmalleable skull bones of older patients make this surgery more difficult, with more intense blood loss. Often, it is prudent to delay the start of the operation until blood products are physically present in the operating room. Anticipation of the need for blood replacement and careful intraoperative monitoring of the volume of blood loss are essential for successful surgery.
Although several agents for bleeding control are available, such as bone wax, Surgicel, and fibrin glue, blood loss continues to occur in the immediate postoperative period. Therefore, blood transfusion is frequently required in the first 2 postoperative days. In the present study, all the patients required blood transfusion (~280 ml blood), and this volume may correspond to 40% of the total blood volume in a 3-month-old child. New technologies such as preoperative injection of erythropoietin and autologous transfusion are used by large North-American centers. However, because of their high costs, these modalities have not yet been introduced in the Brazilian National Health System (SUS). The current economic growth in Brazil and an increase in the resources for public health will facilitate access to new technologies in hospitals, ultimately reducing the potential risks inherent to a major surgery.
Measurement of the craniofacial structures is essential for diagnosis and monitoring of changes in growth; moreover, it may indicate the effectiveness of surgical intervention. Several methods for these measurements are available, such as X-ray, 3-dimensional computed tomography (CT), and magnetic resonance imaging. CT has the disadvantage of exposing children to a radioactive load; moreover, it requires the presence of an anesthesiologist during the surgery, which may not be possible on short notice. Alternative measurement methods, such as 3-dimensional photography and plagiocephalometry, can be used; however, they are not always applicable because of technical difficulties and scarcity of the required materials. In our department, the measurements were carried out by the same evaluator using a metric-scale tape and goniometer.
The CAI was used to verify, through measurements in the preoperative and postoperative periods, whether the surgical results visible upon clinical examination were significant. The obtained p value (p=0.0109) demonstrated that the postoperative CAI average was significantly lower than the preoperative CAI average, indicating a strong tendency for symmetry after the surgery. Clinically, the skull of all the patients had advanced toward symmetry, demonstrating the efficiency of the surgical technique for correction of UCC.
CONCLUSION
Surgical correction is effective for achieving craniofacial symmetry in patients with UCC. Overcorrection of the bony structures is required to obtain craniofacial symmetry postoperatively.
REFERENCES
1. Pyo DJ, Persing J. Craniosynostosis. In: Aston SJ, Beasley RW, Thorne CHM, Grabb WC, Smith JW, eds. Grabb and Smith's Plastic Surgery. Philadelphia:Lippincott-Raven;1997. p.281-304.
2. Sakurai A, Hirabayashi S, Sugawara Y, Harii K. Skeletal analysis of craniofacial asymmetries in plagiocephaly (unilateral coronal synostosis). Scand J Plast Reconstr Surg Hand Surg. 1998;32(1):81-9.
3. Raposo-Amaral CE, Nunes PF, Buzzo CL, Raposo-Amaral VL, Raposo- Amaral CM. Long-term follow up: report of 7 cases of unilateral coronal synostosis. Proceedings of Tenth International Congress of the International Society of Craniofacial Surgery. In: Salyer K, ed. Bologna:Medimond;2003. p.195-7.
4. Silva-Freitas RD, Alonso N, Shin JH, Persing J. Assimetrias cranianas em crianças: diagnóstico e tratamento. Rev Bras Cir Craniomaxilofac. 2010;13(1):44-8.
5. Kawamoto HK, Heller JB, Heller MM, Urrego A, Gabbay JS, Wasson KL, et al. Craniofrontonasal dysplasia: a surgical treatment algorithm. Plast Reconstr Surg. 2007;120(7):1943-56.
6. Foo R, Guo Y, McDonald-McGinn DM, Zackai EH, Whitaker LA, Bartlett SP. The natural history of patients treated for TWIST1-confirmed Saethre-Chotzen syndrome. Plast Reconstr Surg. 2009;124(6):2085-95.
7. Ranger A, Chaudhary N, Rau J, Matir D, Goobie S. Coronal synostosis syndrome (Muenke syndrome): the value of genetic testing versus clinical diagnosis. J Craniofac Surg. 2011;22(1):187-90.
8. Rogers GF, Proctor MR, Mulliken JB. Unilateral fusion of the frontosphenoidal suture: a rare cause of synostotic frontal plagiocephaly. Plast Recontr Surg. 2002;110(4):1011-21.
9. Gault DT, Renier D, Marchac D, Jones BM. Intracranial pressure and intracranial volume in children with craniosynostosis. Plast Reconstr Surg. 1992;90(3):377-81.
10. Cooper GM, Mooney MP, Gosain AK, Campbell PG, Losee JE, Huard J. Testing the critical size in calvarial bone defects: revisiting the concept of a critical-size defect. Plast Reconstr Surg. 2010;125(6):1685-92.
1. Full Member of the Brazilian Society of Plastic Surgery (BSPS), Regent of the Chapter on Craniofacial Surgery of the BSPS, Vice-President of the SOBRAPAR Hospital, Campinas, SP, Brazil.
2. Resident Physician at the SOBRAPAR Hospital, Campinas, SP, Brazil.
3. Associate Member of the BSPS, Supervisor of Resident Physicians in Plastic Surgery at the Hospital SOBRAPAR, Campinas, SP, Brazil.
4. Full Member of the BSPS, Regent of the Plastic Surgery Service Professor. Dr. Cassio Raposo do Amaral, Campinas, SP, Brazil.
Corresponding author:
Cassio Eduardo Raposo-do-Amaral
Hospital de Crânio e Face SOBRAPAR
Av. Adolpho Lutz, 100 - Cidade Universitária
Campinas, SP, Brazil. CEP 13083-880
E-mail: cassioraposo@hotmail.com
Submitted to SGP (Sistema de Gestão de Publicações/Manager Publications System) of RBCP (Revista Brasileira de Cirurgia Plástica/Brazilian Journal of Plastic Surgery).
Received: December 18, 2010
Accepted: February 5, 2011
Work performed at the Hospital de Crânio e Face SOBRAPAR - (SOBRAPAR Hospital), Campinas, SP, Brazil.


 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter