

Original Article - Year 2025 - Volume 40Issue 1
Outcomes of Pregnancy in Patients Submitted to Postbariatric Fleur-De-Lis Abdominoplasty
Desfechos da gestação em pacientes submetidas à abdominoplastia pós-bariátrica em âncora
ABSTRACT
Introduction: Obesity is a growing condition leading to a concomitant increase in bariatric procedures. The anchor-line or fleur-de-lis abdominoplasty improves body contour by excising redundant skin and subcutaneous tissue. Pregnancy implies abdominal distension, both musculoaponeurotic and cutaneous. However, the knowledge of its relationship with abdominoplasty remains scarce, especially regarding the potential negative effects on esthetic outcomes or abdominoplasty-related increases in gestational complications.
Materials and Methods: We conducted a retrospective study on patients submitted to postbariatric fleur-de-lis abdominoplasty from 2012 and 2023 who subsequentially got pregnant. We assessed their medical records, photographic archives, and answers to an online questionnaire.
Results: The study included seven patients, all previously submitted to gastric bypass. Although one patient suffered a miscarriage, the remaining subjects had successful pregnancies. Six patients noticed an altered pattern of abdominal growth. Five pregnancies were full-term, and one was preterm; the delivery route was cesarean section in five patients and vaginal labor in one subject. Two newborns were small for their gestational age. The reported esthetic issues included a new onset of striae in five patients, scar stretching in four, and excessive skin worsening in six subjects. The preand postpregnancy scores decreased from 8.7 to 5.8 points. One patient reported no changes in the esthetic outcomes.
Conclusion: Although pregnancy had some influence on abdominoplasty esthetic outcomes, the impairment was not severe. Pregnancy and delivery in patients previously submitted to postbariatric fleur-de-lis abdominoplasty did not present a higher complication rate.
Keywords: abdominoplasty; bariatric surgery; body contouring; obesity; pregnancy; surgery; plastic
RESUMO
Introdução: A obesidade é cada vez mais prevalente na atualidade, com consequente crescimento da realização de cirurgias bariátricas. A abdominoplastia pós-bariátrica em âncora é um procedimento cirúrgico para a melhora do contorno corporal pelo tratamento do excedente de pele e tecido subcutâneo abdominal. Sabe-se que a gravidez é um período no qual ocorre distensão da parede abdominal muscular e cutânea; no entanto, sua interferência nos resultados estéticos da abdominoplastia e os potenciais efeitos desta no processo gestacional são pouco conhecidos.
Materiais e Métodos: Realizamos estudo retrospectivo emque pacientes submetidas a abdominoplastia pós-bariátrica em âncora entre 2012 e 2023 que engravidaram posteriormente tiveram dados de prontuário e registro fotográfico avaliados e responderam a um questionário online.
Resultados: Foram avaliadas sete pacientes, todas submetidas a bypass gástrico. Uma paciente apresentou aborto, e as demais completaram a gestação. Seis pacientes relataram crescimento alterado do abdome na gestação. Cinco tiveram gestações a termo e uma, pré-termo; a via de parto foi cesariana em cinco pacientes e vaginal em uma. Dois recém-nascidos foram considerados pequenos para a idade gestacional. Entre as alterações estéticas houve novas estrias abdominais em cinco pacientes, alargamento da cicatriz em quatro e novo excesso de pele em seis. Houve redução de 8,7 para 5,8 pontos nas pontuações de resultado pré e pós-gestação. Apenas uma paciente referiu resultados inalterados.
Conclusão: Embora os resultados estéticos abdominais tenham sido impactados pela gestação, o grau de comprometimento não foi severo. A gestação e o parto em pacientes submetidas à abdominoplastia pós-bariátrica em âncora não apresentaram aumento de complicações.
Palavras-chave: abdominoplastia; cirurgia bariátrica; cirurgia plástica; contorno corporal; gravidez; obesidade
Introduction
Obesity is a condition currently experiencing a significant increase in prevalence. According to data from the World Health Organization (WHO), in 2022, more than 1 billion people in the world were obese, including 650 million adults, 340 million adolescents, and 39 million children. As a result, the last decade witnessed a massive increase in bariatric surgeries as a treatment option for obese patients.
Obesity in women of childbearing age has increased worldwide in recent decades, and an increasing number of patients undergoing bariatric surgery are females in this age group.1According to a 2019 report by the International Federation of Surgery for Obesity and Metabolic Diseases (IFSO), 833,687 bariatric procedures occurred in 61 countries, including 77.1% female patients, with an average age of 43 years. A pilot study2 for the national registry of Brazilian data on bariatric surgery, implemented in 7 reference centers selected by the Brazilian Society of Bariatric and Metabolic Surgery (Sociedade Brasileira de Cirurgia Bariátrica e Metabólica, SBCBM, in Portuguese), identified that 67.2% of the sample were female patients, with a mean age of 39 years. Some authors3-5 have reported that bariatric surgery has a positive effect on maternal and fetal outcomes, reducing the risk of gestational diabetes, gestational hypertensive diseases, prematurity, fetal macrosomia, and maternal complications during childbirth.
Postbariatric surgery abdominoplasty occurs after massive weight loss to improve body contour by removing excess skin and subcutaneous fat from the abdominal wall. In addition, it restores musculoaponeurotic integrity, resulting in improved physical, psychological, and social well-being.6,7
In these cases, two techniques are usually applied. Conventional horizontal abdominoplasty predominantly enables the treatment of the region below the umbilical scar and plication of the anterior aponeurosis of the rectus abdominis muscles in the midline to treat diastasis, when present, requiring a wide detachment of the abdominal flap, and keeping the umbilical scar adhered to its deep pedicle for subsequent transposition.8The anchor-line or fleur-de-lis abdominoplasty occurs most frequently in patients after significant weight loss and, in addition to the horizontal incision, it uses a vertical xiphopubic component to treat both the vertical and side-to-side directions, especially in the epigastric region. Currently, neoumbilicoplasty is associated with this approach, that is, discarding the original umbilical scar and using skin flaps from the remaining abdominal skin for umbilical reconstruction. We prefer using two lateral quadrangular flaps, as the technique has shown superior outcomes for navel shape and appearance.9,10
Pregnancy leads to progressive distension of the abdominal wall with widening of the linea alba and the aponeurosis of the rectus abdominis muscles. It is the main etiology of sagging and excessive abdominal skin for surgical treatment in non-postbariatric patients. Thus, patients who get pregnant after abdominoplasty could, in addition to compromising the esthetic outcome, have compromised the stability of muscle plication, favoring its distension or rupture and even the appearance of epigastric, incisional or umbilical hernias,11-17 new sagging, and excessive skin.
On the other hand, rectus abdominis muscle plication can increase intra-abdominal pressure and, consequently, potentially decrease maternal lung function during pregnancy. Increased intra-abdominal pressure could also reduce uterine perfusion and restrict intrauterine fetal growth, alter labor dynamics, and increase the number of cesarean sections.18-20
Few published studies report the effects of pregnancy on the aesthetic outcome of abdominoplasty and the potential maternal-fetal consequences during pregnancy caused by abdominoplasty: only two case series21,22 have been published on the subject to date. Although one21 included postbariatric patients, there was no discrimination regarding the type of abdominoplasty.
Objective
The current study aimed to evaluate the impacts of pregnancy on the the esthetic outcomes of the abdominal wall of patients previously submitted to postbariatric abdominoplasty and the occurrence of maternal-fetal complications in these subjects.
Materials and Methods
This retrospective, descriptive, observational study was conducted at the Plastic Surgery Outpatient Clinic of the Teaching Hospital of Universidade Estadual de Campinas (Unicamp) and the private clinic of the principal investigator (DRC).
The study included patients who got pregnant after abdominoplasty postbariatric surgery, operated on between 2012 and 2023. We excluded patients refusing to participate in the research and those with incomplete data.
After identifying the patients who underwent postbariatric anchor abdominoplasty through the review of medical records, including photographic documentation, we contacted the patients by telephone to identify those who had gotten pregnant after the procedure.
After agreeing to participate in the study and filling out the free and informed consent form, we invited the patients to answer an online questionnaire in the Google Forms platform to collect data regarding date of birth, date of delivery, gestational age, obstetric and gestational history, diseases/ complications during and after pregnancy, previous comorbidities and use of medications, height, weight, and potential diseases of the newborn, as well as the personal evaluation of the esthetic outcome of the abdominal wall after pregnancy. We obtained data regarding the surgeries (bariatric surgery and abdominoplasty) from the medical records.
The Ethics in Research Committee of Unicamp’s School of Medical Sciences approved the study under protocol number CAAE: 71036423.4.0000.5404.
Results
Clinical characteristics of the patients
We identified 7 patients who underwent anchor-type abdominoplasty postbariatric surgery from 2012 to 2023 and got pregnant. All of them underwent gastric bypass surgery with Roux-en-Y reconstruction, and in 1 of them we opted for concomitant gastric ring placement. The mean age at bariatric surgery was of 26 years, ranging from 20 to 30 years. The mean weight before the bariatric surgery was of 113 kg, with a mean body mass index (BMI) of 41.7 kg/m2. The mean weight before abdominoplasty was of 68 kg, with a mean weight loss of 45 kg between the bariatric surgery and the abdominoplasty. All patients underwent abdominal surgery with a BMI below 28 kg/m2, with a mean BMI of 25.4 kg/m2. The mean current weight at the time of the study was of 76 kg, corresponding to a mean BMI of 28 kg/m2.
Regarding obstetric history, 6 patients were multiparous, and 1 subject was primiparous. A single patient reported a miscarriage in previous pregnancies. Only 2 patients were smokers, and there were no other findings regarding habits such as alcoholism or the use of illicit substances (►Table 1).
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | |
|---|---|---|---|---|---|---|---|
| Current age (years) | 38 | 39 | 39 | 36 | 41 | 31 | 30 |
| Habits/addictions | None | Smoking | Smoking | None | None | None | None |
| Date of bariatric surgery | 2013 | 2014 | 2015 | 2013 | 2009 | 2018 | 2014 |
| Age at bariatric surgery (years) | 28 | 29 | 30 | 26 | 26 | 25 | 20 |
| Prebariatric weight (kg) | 100 | 112 | 143 | 113 | 130 | 104 | 95 |
| Prebariatric Body Mass Index (kg/m2) | 39.1 | 42.7 | 44.6 | 39.6 | 48.9 | 39.6 | 37.6 |
| Weight loss between bariatric surgery and abdominoplasty (kg) | 35 | 42 | 53 | 43 | 75 | 34 | 39 |
| Date of abdominoplasty | 2019 | 2019 | 2016 | 2016 | 2012 | 2019 | 2019 |
| Preabdominoplasty weight (kg) | 65 | 70 | 90 | 70 | 55 | 70 | 56 |
| Preabdominoplasty Body Mass Index (kg/m2) | 25.5 | 26.7 | 28.1 | 24.5 | 20.7 | 26.7 | 22.2 |
| Current weight (kg) | 75 | 70 | 96 | 75 | 72 | 82 | 65 |
| Current Body Mass Index (kg/m2) | 29 | 26 | 29 | 26 | 27 | 31 | 25 |
| Total number of pregnancies | 3 | 4 | 3 | 2 | 1 | 2 | 2 |
BMI, Body mass index.
Characterization of the postabdominoplasty gestational process
The mean interval between pregnancy and abdominoplasty was of 4 years, and no patient presented comorbidities when becoming pregnant after abdominoplasty. The mean prepregnancy weight was of 70 kg, corresponding to a mean BMI of 26.7 kg/m2. One patient (patient 4) had a miscarriage at 12 weeks of gestation, while the others completed their pregnancy. Five patients had diseases during the gestational period, and 1 developed a left inguinal hernia at the end of pregnancy.
Four patients reported abdominal pain or discomfort during pregnancy that they considered different from what they had felt in previous pregnancies. Five patients whose pregnancies progressed to term reported changes in the abdominal growth pattern during pregnancy, with 4 reporting a greater atypical volume increase in the upper part (►Table 2).
| Patient 1 | Patient 2 | Patient 3 | Patient 4 | Patient 5 | Patient 6 | Patient 7 | |
|---|---|---|---|---|---|---|---|
| Time between abdominoplasty and pregnancy (years) |
4 | 4 | 5 | 5 | 3 | 4 | 5 |
| Weight before pregnancy (kg) | 70 | 68 | 95 | 70 | 55 | 80 | 57 |
| Body Mass Index before pregnancy (kg/m2) | 27.3 | 25.9 | 29.6 | 24.5 | 20.7 | 30.5 | 22.5 |
| Miscarriage after abdominoplasty | No | No | No | Yes | No | No | No |
| Gestational diseases | Gestational anemia | Placenta previa | Uterine carcinoma | None | None | Gestational anemia | Gestational diabetes |
| Abdominal pain/discomfort during pregnancy | Yes | Yes | No | Not applicable | Yes | Yes | No |
| Hernia during pregnancy | No | No | No | No | Yes (left inguinal hernia) | No | No |
| Different abdominal shape during pregnancy (growth pattern) |
Yes (small abdominal volume increase) | Yes (more superior increase) | Yes (more superior increase) | Not applicable | Yes (more central increase) | Yes (more superior increase) | No |
| Patient 1 | Patient 2 | Patient 3 | Patient 5 | Patient 6 | Patient 7 | |
|---|---|---|---|---|---|---|
| Date of birth | February 25, 023 |
April 17, 2021 | October 15, 2021 | April 14, 2015 | May 24, 2023 | December 02, 2022 |
| Gestational age | 38 weeks | 38 weeks | 34 weeks | 39 weeks | 38 weeks | 39 weeks |
| Delivery route | Cesarean section | Cesarean section | Cesarean section | Cesarean section | Cesarean section | Vaginal |
| Birth weight | 2,622 g | 1,820 g | 2,600 g | 3,075 g | 3,660 g | 2,800 g |
| Birth length | 45 cm | 41 cm | 48 cm | 48 cm | 47 cm | 42 cm |
Fetal and delivery outcomes of postabdominoplasty pregnancy
Five patients had full-term pregnancies, and 1 subject had a preterm gestation. Five patients underwent a cesarean section, and only 1 had a vaginal delivery. Two newborns were considered small for the gestational age, and the other 3 were presented adequate size for the gestational age. No newborns presented pathological alterations at birth or during pregnancy.
Esthetic outcomes of the abdominal wall after pregnancy
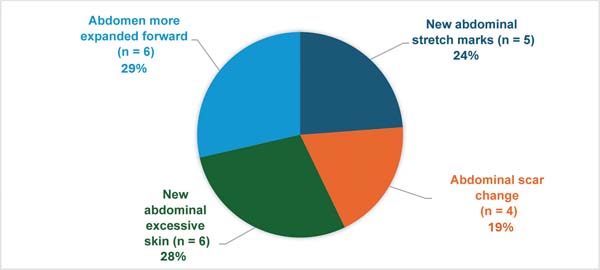
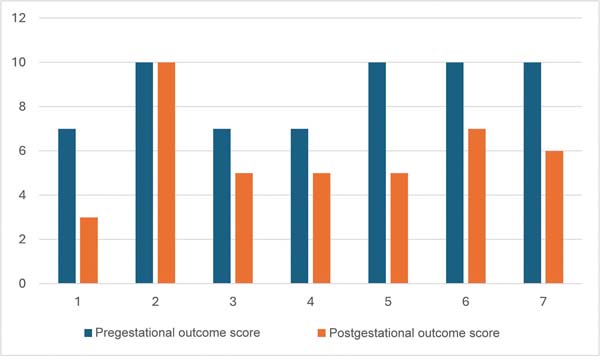
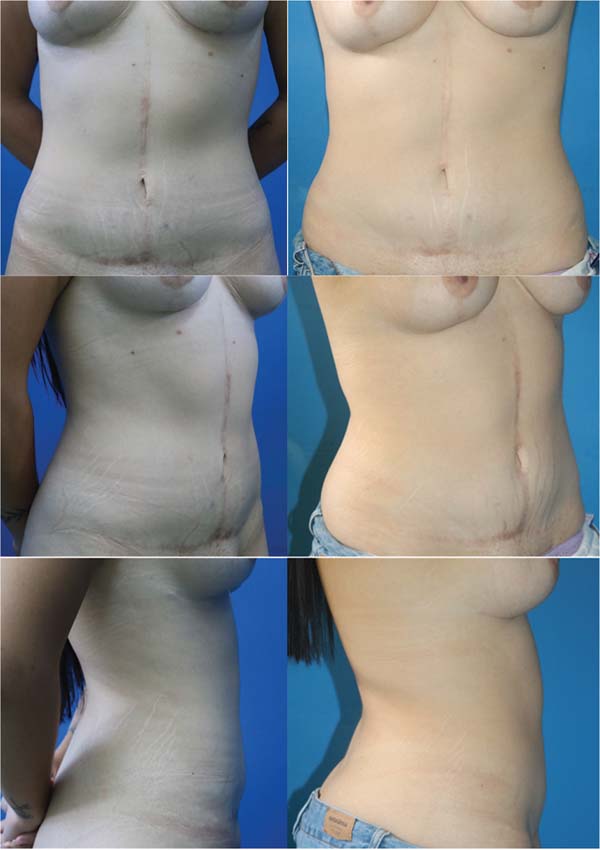
Five patients presented new stretch marks on the abdomen after pregnancy, and 4 subjects reported abdominoplasty scar widening. Six patients presented new excessive skin on the abdomen. In addition, they said that the abdomen was more expanded forward after the gestational period (►Fig. 1). We asked the patients to assign a score from 0 to 10 to the abdominoplasty outcomes before and after pregnancy. The mean prepregnancy score was of 8.7 points, and the mean postpregnancy score, of 5.8 points, indicating a reduction of 2.9 points, or 33.3%. A single patient felt no worsening of the abdominoplasty outcomes (►Fig. 2). ►Figs. 3-5 illustrate the evolution of the esthetic outcomes of the abdominal wall in patient 6 (who reported worsening from 10 to 7 in the self-assigned score) and patient 7 (who reported worsening from 10 to 6 in the self-assigned score). No patient underwent a new abdominoplasty after the last pregnancy.


Discussion
The recent increase in the obese population in Brazil has consequently increased the number of bariatric surgeries. Data from the SBCBM indicate the performance of 74,738 procedures in 2022 compared with 34,629 in 2011. In addition, a study2 in 7 bariatric surgery centers in Brazil, including 1,363 procedures, showed thatmostpatientswere women (67.2%) with an average age of 39 years. All patients in the current study underwent bariatric surgery at a childbearing age, with an average age of 26 years.
We expect to observe a higher number of pregnant women who previously underwent postbariatric abdominoplasty in the coming years, and there are no studies evaluating the degree of satisfaction of patients who got pregnant after this procedure regarding the postgestational outcomes.
Few scientific articles in the literature report the esthetic impacts of postoperative abdominoplasty after pregnancy. Abdominoplasty is a body-contouring procedure often performed due to abdominal wall sagging, and the most significant interventions include excision of excess skin and aponeurosis plication to treat diastasis of the rectus abdominis muscles. The literature6-8,23,24 indicates that the increased intra-abdominal pressure during pregnancy can compromise the esthetic and functional outcomes of abdominoplasty, evolving with recurrence of excessive skin and muscle diastasis, abdominal bulging, scar changes, and the appearance of new stretch marks.
According to Faessen et al.,25 the fibrotic tissue secondary to the repair of the rectus abdominis muscle diastasis is strong enough to withstand the changes in intra-abdominal pressure during pregnancy. However, in the immediate postoperative period, the fibrotic tissue may not be strong enough to support pregnancy, and its maturation will be complete approximately 1 year after surgery. In addition, the hormones released during pregnancy promote tissue elasticity, stretching other abdominal wall muscles (transverse, internal oblique, and external oblique) and reducing the tension in the rectus abdominis muscle. The last stage in the physiological wound healing process is maturation, which lasts approximately 1 to 2 years, featuring collagen fiber remodeling and type-III collagen replacement by type-I collagen, promoting increased scartensile strength and wound contraction.26 All patients in the present study got pregnant more than 1 year (range: 3-5 years) after abdominoplasty and reported changes in the growth pattern of the abdominal wall during pregnancy. This change can result from higher intra-abdominal pressure, hindering the abdominal wall from expanding centrally due to the plication of the rectus abdominis muscle during abdominoplasty.
Per Oma et al.,15 in a descriptive study with more than 20 thousand pregnant women, 0.08% and 0.12% of sample presented primary ventral and inguinal hernias respectively. In the current study, a single pregnant woman developed an inguinal hernia at the end of pregnancy, which does not suggest an increased frequency, especially when compared with the previous series of pregnancies after abdominoplasty, which found a frequency of 6.3%22 However, due to the small sample and lack of a control group, we cannot draw conclusions on the incidence of abdominal wall hernias after pregnancy in patients undergoing abdominoplasty postbariatric surgery.
Sagie et al.22conducted a descriptivecross-sectional study with 32 patients who got pregnant after abdominoplasty. Among these patients, 15% had late preterm births, 1 had a miscarriage, and 1 had an emergency cesarean section. In the current study, 5 patients underwent a cesarean section, which is not at odds with the overall incidence of cesarean sections in Brazil, corresponding to more than 50% of deliveries.27 Five patients had full-term pregnancies, with gestational ages ranging from 38 to 39 weeks, and 1 patient was preterm, with a gestational age of 34 weeks. Two newborns were considered small for the gestational age, and the other 4 had an appropriate size for the gestational age. No newborn had complications at birth. Although the small sample size does not enables us to draw statistical conclusions from these data, the frequencies of prematurity and small-for-gestational-age newborns does not appear to differ from previous Brazilian epidemiological data,28-30 a priori not corroborating the suspicions that abdominoplasty would imply significant intrauterine growth restriction.
Moreover, according to Sagie et al.,22 pregnancy compromised the esthetic outcomes, with the appearance of new stretch marks in 50% of the cases, widening of the abdominoplasty scar in 28%, resulting in new excessive abdominal skin in 37%, and abdominal bulging in 25%. Two patients underwent postpregnancy abdominoplasty revision, and all patients reported some degree of esthetic compromise after pregnancy. In the present study, most patients (n ¼ 6; 85.7%) reported some degree of compromise of the esthetic abdominoplasty outcome after pregnancy (►Fig. 2), including the appearance of stretch marks, scar widening, recurrence of excessive skin, or change in the abdominal shape (►Fig. 1). Despite the evaluation made by the patients themselves, who in virtually all cases reported some noticeable outcome worsening, we did not observe a significant worsening of the general appearance in cases with a longer follow-up, with a significant improvement concerning the preoperative abdominoplasty (►Figs. 3-4). Thus, we conclude that, despite the changes mentioned, most of the results remained, and none of the patients in the study were motivated to seek a new surgical intervention.
It is worth considering, when analyzing the change in the results, that all patients presented weight gain during the period, progressing from an average preoperative BMI of 25.4 kg/m2 to 26.7 kg/m2 prepregnancy and, finally, to 28 kg/m2 at the self-assessment, corresponding to an average weight increase of 8 kg. New weight gain can interfere with the maintenance of the outcomes of body-contouring surgeries and is a common phenomenon in the postbariatric population,31 who tend to experience higher weight gain than subjects who have not undergone bariatric surgery after body-contouring surgeries.32
It is interesting to observe the specific aspects of anchorline abdominoplasty, namely the appearance of the vertical scar and the shape of the neoumbilicus. Umbilical scar changes are common after pregnancy. There were no previous reports on how the standard umbilical reconstruction in anchor-line abdominoplasty would evolve in these cases. Cases evaluated with photographic comparison showed good maintenance of the diameter and shape of the neoumbilicus, with no widening, in the presence of postgestational abdominal sagging.
Few studies in the literature evaluated maternal and fetal morbidity in pregnant women who had undergone abdominoplasty. Current studies20,21 suggest that abdominoplasty may increase the frequency of cesarean sections. Menz17 reported a case of an uneventful pregnancy in a 37-yearold woman who had undergone abdominoplasty 3 years earlier and had a cesarean delivery. Nahas13 reported a 25- year-old patient who became pregnant 2 years after abdominoplasty, which was uneventful. Wallach33 described a case of a 24-year-old woman who became pregnant 6 months after abdominoplasty and had an uneventful vaginal delivery. In the present study, 5 patients underwent cesarean section, 1 patient had a vaginal delivery, and 1 patient had a miscarriage. The reported gestational diseases, such as gestational anemia, placenta previa, gestational diabetes, and uterine carcinoma, do not appear to be related to previous abdominoplasty.
Concerning bariatric surgery, according to Pajula et al.,21 previous bariatric procedures did not increase the risk of premature birth or low birth weight, and the authors considered pregnancy after abdominoplasty safe. However, the first 12 to 16 months after bariatric surgery are a period of excessive weight loss and significant metabolic changes, which can cause nutritional deficiencies. As a result, it is advisable to wait 2 years before a future pregnancy.34,35 In the present study, we only included patients who became pregnant after abdominoplasty postbariatric surgery, with a time interval of more than 2 years between procedures. Two newborns were small for their gestational age. Only 1 newborn was premature at birth (16%). We believe prior abdominoplasty is unrelated to prematurity, since its prevalence in Brazil from 2011 to 2021 was of 11%,28 which is consistent with our findings.
We believe that our results can support patients and surgeons in the decision-making process regarding the performance of postbariatric anchor-line abdominoplasty with neoumbilicoplasty in patients who wish to get pregnant later. However, we must mention some limitations of the study, such as the small sample size, the lack of a control group, and the retrospective design, which do not enable us to draw definitive conclusions, especially regarding gestational complications. Although difficult to perform, prospective studies comparing the esthetic outcomes between women who got pregnant or not after abdominoplasty and between pregnant women who underwent bariatric surgery followed or not by abdominoplasty could offer more accurate conclusions.
Conclusion
Although pregnancy affected the esthetic outcomes of abdominoplasty, the impairment was not severe. The pregnancy and delivery process in patients previously submitted to postbariatric anchor-line abdominoplasty did not increase maternal and fetal complications.
REFERENCES
1. Carvalho ADS, Rosa RDS. Bariatric surgeries performed by the Brazilian National Health System in residents of the Metropolitan Region of Porto Alegre, Rio Grande do Sul, Brazil, 2010-2016. Epidemiol Serv Saude 2018;27(02):e2017010
2. Silva LB, Quadros LGd, Campos JM, Boas MLV, Marchesini JC, Ferraz AAB, et al. Brazilian national bariatric registry - pilot study. Rev Col Bras Cir 2023;50:e20233382. Doi: 10.1590/0100-6991e-20233382-en PubMed
3. Ibiebele I, Gallimore F, Schnitzler M, Torvaldsen S, Ford JB. Perinatal outcomes following bariatric surgery between a first and second pregnancy: a population data linkage study. BJOG 2020;127(03):345-354. Doi: 10.1111/1471-0528.15993
4. Al-Nimr RI, Hakeem R, Moreschi JM, Gallo S, McDermid JM, Pari- Keener M, et al. Effects of Bariatric Surgery on Maternal and Infant Outcomes of Pregnancy-An Evidence Analysis Center Systematic Review. J Acad Nutr Diet 2019;119(11):1921-1943. Doi: 10.1016/j.jand.2019.02.008
5. Kwong W, Tomlinson G, Feig DS. Maternal and neonatal outcomes after bariatric surgery; a systematic review and meta-analysis: do the benefits outweigh the risks? Am J Obstet Gynecol 2018;218 (06):573-580. Doi: 10.1016/j.ajog.2018.02.003
6. De Paep K, Van Campenhout I, Van Cauwenberge S, Dillemans B. Post-bariatric Abdominoplasty: Identification of Risk Factors for Complications. Obes Surg 2021;31(07):3203-3209. Doi: 10.1007/s11695-021-05383-0
7. Schlosshauer T, Kiehlmann M, Jung D, Sader R, Rieger UM. Post- Bariatric Abdominoplasty: Analysis of 406 Cases With Focus on Risk Factors and Complications. Aesthet Surg J 2021;41(01): 59-71. Doi: 10.1093/asj/sjaa067
8. Rosenfield LK, Davis CR. Evidence-based abdominoplasty review with body contouring algorithm. Aesthet Surg J 2019;39(06): 643-661. Doi: 10.1093/asj/sjz013
9. Reno BA, Mizukami A, Calaes IL, Staut JG, Claro BM, Baroudi R, et al. Neo-onfaloplastia no decurso das abdominoplastias em âncora em pacientes pós-cirurgia bariátrica. Rev bras Cir Plást 2013;28(01): 114-118. Doi: 10.1590/S1983-51752013000100019
10. Mizukami A, Ribeiro BB, Renó BA, Calaes ILd, Calderoni DR, Basso RdCF, et al. Análise retrospectiva de pacientes pós-bariátrica submetidosà abdominoplastia com neo-onfaloplastia: 70 casos. Rev Bras Cir Plást 2014;29(01):89-93. Doi: 10.5935/2177-1235.2014RBCP0015
11. Villegas-Alzate FJ, Villegas-Mesa JD. Pregnancy after transverse plication lipoabdominoplasty, undermining halted at umbilicus, liposuction without restrictions, umbilicoplasty with a skin graft, and low transverse scar localization (TULUA). Literature review and case report. Rev Colomb Obstet Ginecol 2020;71(04): 374-383. Doi: 10.18597/rcog.3567
12. Janes LE, Fracol ME, Dumanian GA. Appreciation of postpartum changes of the rectus muscles in primary and repeated abdominoplasty. Plast Reconstr Surg 2019;144(02):197e-204e. Doi: 10.1097/PRS.0000000000005862
13. Nahas FX. Pregnancy after abdominoplasty. Aesthetic Plast Surg 2002;26(04):284-286. Doi: 10.1007/s00266-002-1487-y
14. Oma E, Henriksen NA, Jensen KK. Ventral hernia and pregnancy: A systematic review. Am J Surg 2019;217(01):163-168. Doi: 10.1016/j.amjsurg.2018.04.016
15. Oma E, Bay-Nielsen M, Jensen KK, Jorgensen LN, Pinborg A, Bisgaard T. Primary ventral or groin hernia in pregnancy: a cohort study of 20,714 women. Hernia 2017;21(03):335-339. Doi: 10.1007/s10029-017-1618-7
16. Borman H. Pregnancy in the early period after abdominoplasty. Plast ReconstrSurg2002;109(01):396-397. Doi: 10.1097/00006534-200201000-00070
17. Menz P. Pregnancy after abdominoplasty. Plast Reconstr Surg 1996; 98(02):377-378. Doi: 10.1097/00006534-199608000-00038
18. Kuzmin V, Kutyrev D, Nudelman S, Golubkov N. Intraabdominal hypertension in aesthetic abdominoplasty: 1AP5-5. EJA 2014; 31:18. Doi: 10.1097/00003643-201406001-00049
19. Pereira N, Sciaraffia C, Danilla S, Parada F, Asfora C, Moral C. Effects of abdominoplasty on intra-abdominal pressure and pulmonary function. Aesthet Surg J 2016;36(06):697-702. Doi: 10.1093/asj/sjv273
20. Pimentel VM, Powell K, Karkowsky CE. Is the cesarean delivery rate higher after abdominoplasty? Obstetrical outcomes in the setting of abdominoplasty. . [7C]Obstet Gynecol 2016;127:28S Doi: 10.1097/01.AOG.0000483356.94088.2b
21. Pajula S, Gissler M, Kaijomaa M, Jyränki J, Tukiainen E, Koljonen V. Pregnancy and delivery after lower body contouring surgery is safe for the mother and child. J Plast Reconstr Aesthet Surg 2021; 74(01):143-151. Doi: 10.1016/j.bjps.2020.08.008
22. Sagie RA, Wiser I, Heller L, Klein D, Hadad E. Pregnancy Reverses Abdominoplasty Aesthetic Outcome: Myth or Misconception? A Cross-Sectional Study. Aesthet Surg J 2022;42(01):NP20-NP26. Doi: 10.1093/asj/sjab356
23. Marouf A, Mortada H. Complications of Body Contouring Surgery in Postbariatric Patients: A Systematic Review and Meta-Analysis. Aesthetic Plast Surg 2021;45(06):2810-2820. Doi: 10.1007/s00266-021-02315-2
24. Marchica P, Costa AL, Brambullo T, Marini M, Masciopinto G, Gardener C, et al. Retrospective Analysis of Predictive Factors for Complications in Abdominoplasty in Massive Weight Loss Patients. Aesthetic Plast Surg 2023;47(04):1447-1458. Doi: 10.1007/s00266-022-03235-5
25. Faessen JL, Meesters-Caberg MAJ, Stoot JHMB. Pregnancy after abdominoplasty with mesh placement: A case report. JPRAS Open 2020;26:8-11. Doi: 10.1016/j.jpra.2020.08.003
26. Neligan PC. Plastic Surgery - Vol. 1 Principles. 5th ed. Philadelphia: Elsevier; 2024
27. Boerma T, Ronsmans C, Melesse DY, Barros AJD, Barros FC, Juan L, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet 2018;392(10155):1341-1348. Doi: 10.1016/S0140-6736(18)31928-7
28. Alberton M, Rosa VM, Iser BPM. Prevalence and temporal trend of prematurity in Brazil before and during the COVID-19 pandemic: a historical time series analysis, 2011-2021. Epidemiol Serv Saude 2023;32(02):e2022603. Doi: 10.1590/S2237-962220 23000200005
29. Tenório MCS, Tenório MB, Ferreira RC, Mello CS, Oliveira ACM. Prevalência de recém-nascidos pequenos para a idade gestacional e fatores associados em uma capital do Nordeste brasileiro. Rev Bras Saude Mater Infant 2018;18(03):539-547. Doi: 10.1590/1806-93042018000300006
30. Barreto CM, Pereira MAL, Rolim ACB, Abbas SA, Langhi DM Junior, Santos AMN. Incidência de recém-nascidos pequenos para a idade gestacional segundo curva de Fenton e Intergrowth-21st em uma maternidade de nível secundário. Rev Paul Pediatr 2021;39: e2019245. Doi: 10.1590/1984-0462/2021/39/2019245
31. Reis MG, Moreira LFG, Carvalho LSVdA, Castro CT, Vieira RAL, Guimarães NS. Weight regain after bariatric surgery: A systematic review and meta-analysis of observational studies. Obes Med 2024;45:100528. Doi: 10.1016/j.obmed.2023.100528
32. Henderson JT, Koenig ZA, Woodberry KM. Weight Control following Body Contouring Surgery: Long-Term Assessment of Postbariatric and Nonbariatric Patients. Plast Reconstr Surg 2023;152 (05):817e-827e. Doi: 10.1097/PRS.0000000000010370
33. Wallach SG. Pregnancy after abdominoplasty. Plast Reconstr Surg 2002;110(07):1805, author reply 1805-1806 . Doi: 10.1097/00006534-200212000-00036
34. Gasmi A, Bjørklund G, Mujawdiya PK, Semenova Y, Peana M, Dosa A, et al. Micronutrients deficiences in patients after bariatric surgery. Eur J Nutr 2022;61(01):55-67. Doi: 10.1007/s00394-021-02619-8
35. Ben-Porat T, Weiss R, Sherf-Dagan S, Nabulsi N, Maayani A, Khalaileh A, et al. Nutritional Deficiencies in Patients with Severe Obesity before Bariatric Surgery: What Should Be the Focus During the Preoperative Assessment? J Acad Nutr Diet 2020; 120(05):874-884. Doi: 10.1016/j.jand.2019.10.017
1. Division of Plastic Surgery, Department of Surgery, Faculty of Medical Sciences,
University of Campinas (Unicamp), Campinas, SP, Brazil
Address for correspondence Davi Reis Calderoni, Departamento de Cirurgia, Faculdade de Ciências Médicas, Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brasil (e-mail: davircal@unicamp.br).
Article received: September 02, 2024.
Article accepted: February 06, 2025.
Conflict of Interests
The authors have no conflict of interests to declare.











 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter