

Original Article - Year 2024 - Volume 39 -
LipoCodes Methodology: Objective Control of Infiltrated and Aspirated Volumes in Liposuction
Metodologia LipoCodes: Controle objetivo de volumes infiltrados e aspirados em lipoaspiração
ABSTRACT
Background Liposuction techniques, technologies, publications, and scientific events evolve continuously seeking better, more predictable outcomes withmaximum potential safety. However, there are no references to objective volume controls for more precise and predictable liposuction outcomes. These objective parameters could improve outcomes and safety, leading to the development of a methodology to obtain objective safety information to support fluid replacement and control regional and total aspirated volumes, thus optimizing surgical time. The present study aimed to describe a method called LipoCodes to measure infiltrated and aspirated volumes, surgical time, and speed in liposuction and fat grafting procedures.
Materials and Methods The LipoCodesmethodology relies on fourmain parameters: fat deposit and graft regions; liposuction depth levels; access portals (incisions); and infiltrated and aspirated volume control.
Results The LipoCodes methodology controls infiltrated, fat suction, and fat graft volumes for each previously defined region as well as liposuction speed.
Discussion The LipoCodes methodology systematizes liposuction regardless of the equipment and preferred technique of each plastic surgeon. The goal is to make liposuction more controlled, objective, didactic, educational, and predictable.
Conclusion The LipoCodes methodology uses simple equipment to measure each milliliter of infiltrated, aspirated, and grafted volumes from previously defined body regions. This information provides objective parameters, volume control in liposuction, and surgical time control.
Keywords: allografts; lipectomy; methods; statistics and numerical data; surgery, plastic
RESUMO
Introdução As técnicas atuais, tecnologias e publicações de lipoaspiração continuam a evoluir, buscando resultados melhores e mais previsíveis com o máximo de segurança possível. Por outro lado, não há referências a controles de volume mais objetivos para obter resultados mais precisos e previsíveis na lipoaspiração, parâmetros objetivos que poderiam melhorar os resultados e a segurança. Dentro deste contexto, foi desenvolvida uma metodologia para obter informações objetivas de segurança, apoiar a reposição de fluidos e o controle de volumes aspirados por região e total, otimizando dessa forma o tempo cirúrgico. O objetivo deste trabalho é descrever uma metodologia denominada Lipocodes, criada para aferir o volume infiltrado e aspirado, o tempo e a velocidade cirúrgica, em procedimentos de lipoaspiração e/ou lipoenxertia.
Materiais e Métodos A metodologia LipoCodes é baseada em regiões de depósito de gordura e regiões de enxerto; níveis de profundidade da lipoaspiração; portais de acesso (incisões); controle de volumes infiltrados e aspirados.
Resultados A metodologia LipoCodes desenvolveu o controle de volumes infiltrados, de sucção de gordura, e de enxerto de gordura, para cada região previamente definida, bem como a velocidade de lipoaspiração.
Discussão A metodologia LipoCodes foi desenvolvida para sistematizar a lipoaspiração, independentemente do equipamento e da técnica preferida de cada cirurgião plástico. O objetivo é tornar a lipoaspiração mais controlada, objetiva, didática e educacional, com mais previsibilidade.
Conclusão A metodologia LipoCodes utiliza equipamentos simples para medir cada mililitro de volume infiltrado, aspirado e enxertado de regiões corporais previamente definidas. Essas informações auxiliam com parâmetros objetivos, controle de volumes em lipoaspiração, bem como controle do tempo cirúrgico.
Palavras-chave: aloenxertos; cirurgia plástica; estatística e dados numéricos; lipectomia; métodos
Introduction
Liposuction techniques, technologies, publications, and scientific events evolve continuously, seeking increasingly better and more predictable outcomes with maximum potential safety.
Searching for better outcomes, there are references1-14 about abdominal and body definition techniques and new technologies with laser, ultrasound, and radiofrequency devices for higher contraction of the fibrous septa and dermis, in addition to fat grafting techniques as great allies for improving outcomes with new preparation techniques and better integration. On the other hand, there are no references to objective volume controls for more precise and predictable liposuction outcomes, which would reduce the need for retouching or refinements by combining aesthetic sensitivity and surgical experience with objective parameters to control infiltrated and aspirated volumes of each body region treated.
Regarding safety, scientific articles15-20 highlighted several points to minimize major and minor complications, emphasizing the significance of selecting a specialist with adequate training in plastic surgery and liposuction. The authors emphasized preoperative measures, including a thorough clinical evaluation, healthy and non-inflammatory nutritional status, avoiding obese patients and combined surgeries, and, especially, limiting surgical times to up to 5hours.
A review revealed many articles highlighting these safety points to avoid complications, the importance of the aspirated volume for prognosis, and the greater risk of longer surgeries. However, there were few references21-24 regarding a more effective control of infiltrated and aspirated volumes to minimize potential major and minor complications.
The present study aimed to describe a methodology called Lipocodes to measure the infiltrated and aspirated volume, time, and surgical speed in liposuction and fat grafting procedures.
Materials and Methods
The current descriptive theoretical study presents the LipoCodes methodology.
The author developed the LipoCodes methodology in 2010 due to the difficulty in knowing exactly what was being infiltrated and aspirated in each body region during liposuction. This information would allow greater control of volumes and more precise outcomes, minimizing reinterventions and increasing the safety level in liposuction.
The lack of a previously described or properly presented model for controlling volumes in liposuction inspired the development of a methodology for volume control in liposuction.
Initially, it consisted of notes on printed paper of the volumes aspirated in the main liposuction regions for greater control. It evolved to control the infiltrated, aspirated, and grafted volumes in liposuction, in addition to the start and end time of infiltration and aspiration.
More recently, in 2021, this information was transferred to a Microsoft Excel (Microsoft Corp, Redmond, WA, USA) spreadsheet using volume automatic calculation tools, prior definition of the liposuctioned and fat-grafted regions, definition of access portals for liposuction/fat grafting, and calculation of the time for infiltration and liposuction. The LipoCodes methodology has been registered at the Brazilian National Institute of Industrial Property (Instituto Nacional da Propriedade Industrial - INPI, in Portuguese) since 2021, under number 920441726.
The LipoCodes methodology consists of four main parameters:
1. FAT DEPOSITION REGIONS AND GRAFT REGIONS;
2. LIPOSUCTION DEPTH LEVELS;
3. ACCESS PORTALS (INCISIONS); AND
4. INFILTRATED AND ASPIRATED VOLUME CONTROL.
1. FAT DEPOSIT AND GRAFT REGIONS:
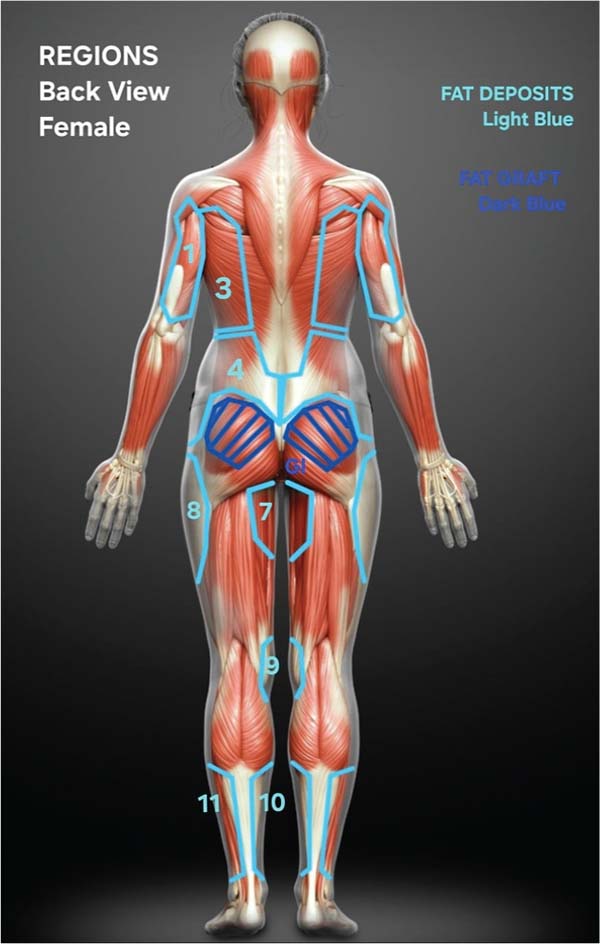
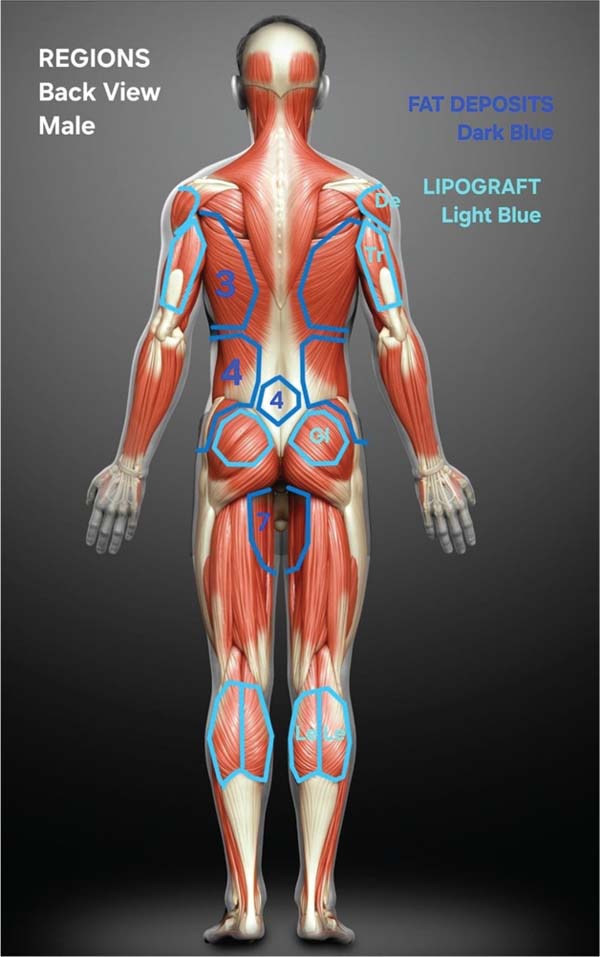
The methodology defines 11 main fat deposit regions and 8 fat graft regions. Their limits (anatomical references) are described below (►Figs. 1-4):
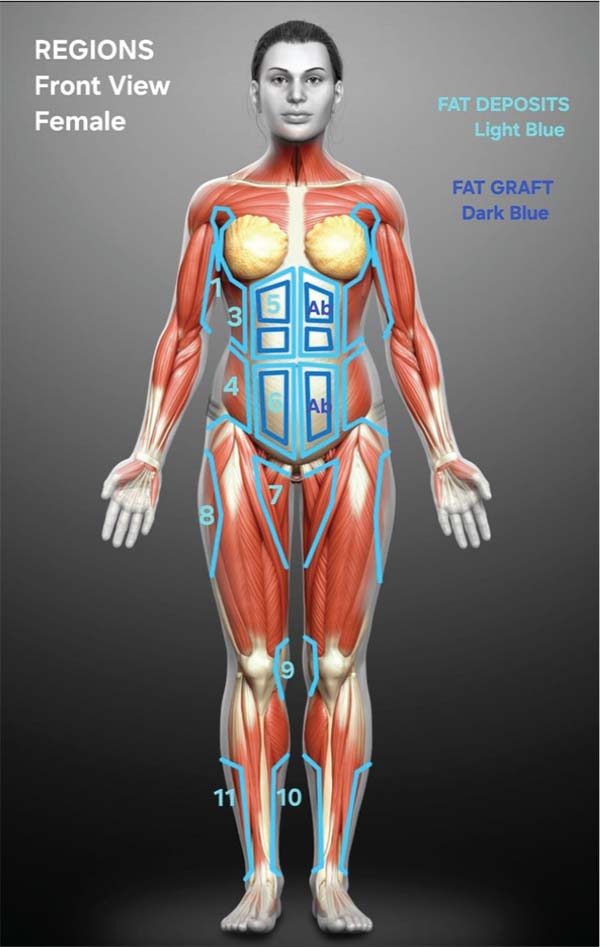
1A. FAT DEPOSITION REGIONS:
Surface of the deltoid muscles (posterior or spinal portion) and triceps.
CHEST (►Fig. 3)
Surface of the pectoralis major muscle (portions with a sternal origin, sixth and seventh ribs, rectus abdominis).
Surface of the serratus anterior muscle (anterior limit), teres major and teres minor muscles (upper limit), and the upper third of the latissimus dorsi muscle (inferior and posterior limit).
Surface of the lower third of the latissimus dorsi muscle (upper limit), thoracolumbar fascia (posterior limit), external oblique muscle (anterior limit), and Lockwood’s ligament (inferior limit).
The medial limit is the linea alba, from the umbilicus to the xiphoid process; the superior limit is the costal margin; the lateral limit is the anterior borders of the serratus and external oblique muscles; and the inferior limit is the horizontal line from the linea semilunaris to the umbilicus.
The medial limit is the linea alba, from the umbilicus to the pubic symphysis; the superior limit is the horizontal line from the linea semilunaris to the umbilicus; the lateral limit is the anterior border of the external oblique muscle; and the inferior limit goes from the inguinal ligament to the pubic symphysis.
Triangle between the inguinal ligament (upper limit), sartorius muscle (lateral limit), posterior border of the adductor magnus muscle (posterior limit).
TROCHANTERAL REGION (►Figs. 1-2)
Tensor fasciae latae muscle (anterior limit), gluteus maximus muscle (posterior limit), vastus lateralis muscle (inferior limit), and Lockwood’s ligament (upper limit).
Inner knees and pes anserinus region (tendons of the gracilis, sartorius, and semitendinosus muscles).
Lower border of the medial gastrocnemius muscle belly (upper limit), calcaneal tendon (posterior limit), tibia (anterior limit), medial malleolus of the tibia (inferior limit).
Lower border of the lateral gastrocnemius muscle belly (upper limit), calcaneal tendon (posterior limit), tibialis anterior muscle (anterior limit), lateral malleolus of the fibula (inferior limit).
1B. FAT GRAFTING REGIONS:
Surface of the rectus abdominis muscles.
Surface of the deltoid muscle (lateral portion).
TRICEPS (Tr) (►Fig. 4)
Surface of the triceps muscle (long and lateral portions).
BICEPS (Bi) (►Fig. 3)
Surface of the biceps muscle (long and short portions).
CHEST (Ch) (►Fig. 3)
Surface of the pectoralis major muscle.
Surface of the gluteus maximus muscle (upper 3/4).
THIGHS (Th) (►Fig. 3)
Surface of the vastus lateralis and vastus medialis muscles.
Surface of the lateral and medial bellies of the gastrocnemius muscle.
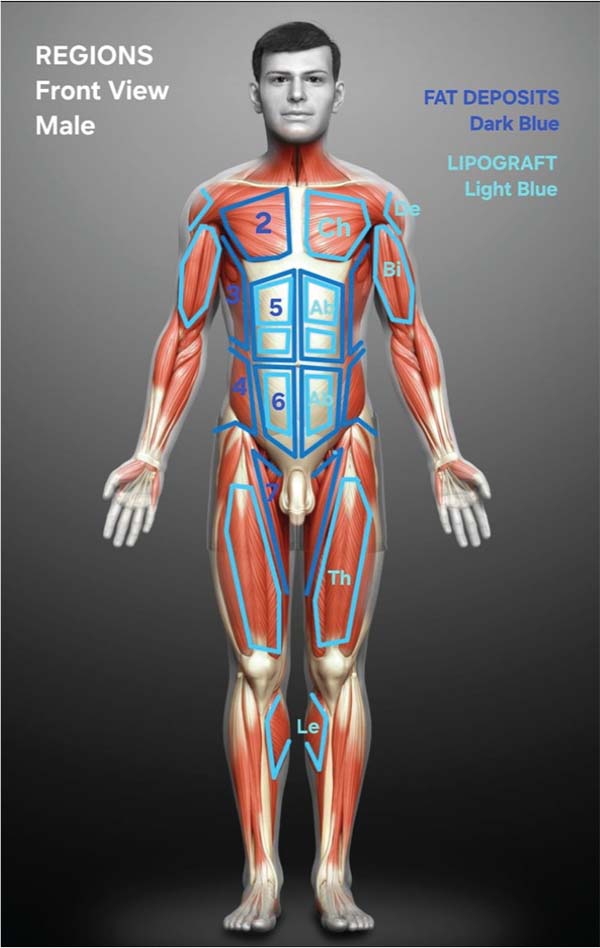
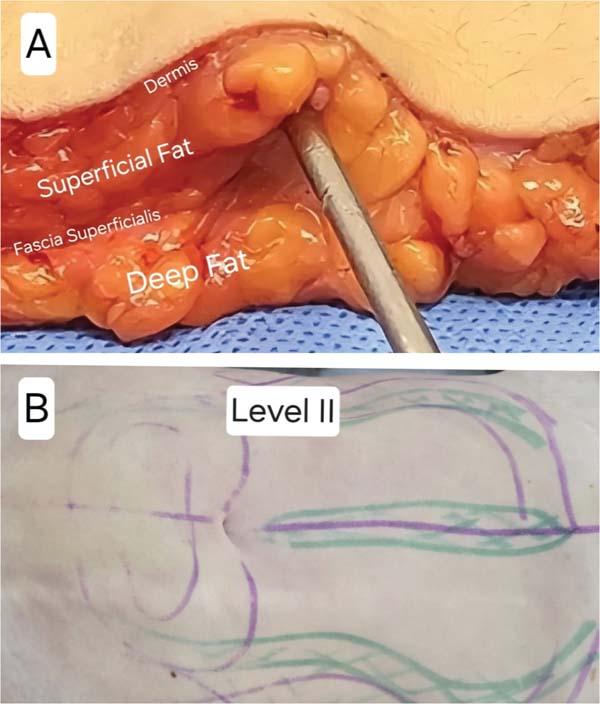
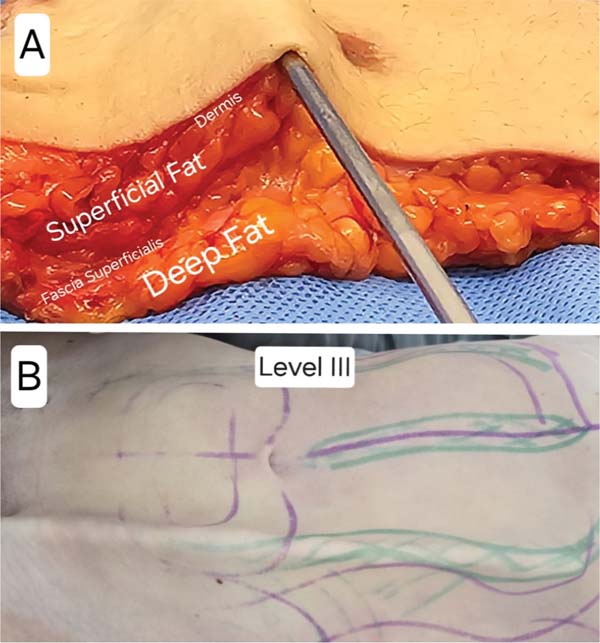
2. LIPOSUCTION DEPTH LEVELS (►Fig. 5):
LEVEL I (►Fig. 5): Liposuction of fat from the deepest plane of the subcutaneous cellular tissue (SCCT) below the superficial fascia and above the muscular fascia.
LEVEL II (►Fig. 6): Liposuction of fat from the SCCT above the superficial fascia and below the dermis.
LEVEL III (►Fig. 7): Liposuction of fat from the SCCT above the superficial fascia and below the dermis. Its difference from level II is its proximity to the dermis (juxtadermal) and positioning of the cannula holes facing downwards. Level III aims to promote the formation of depressions and grooves to highlight planned anatomical elements (definition liposuction).
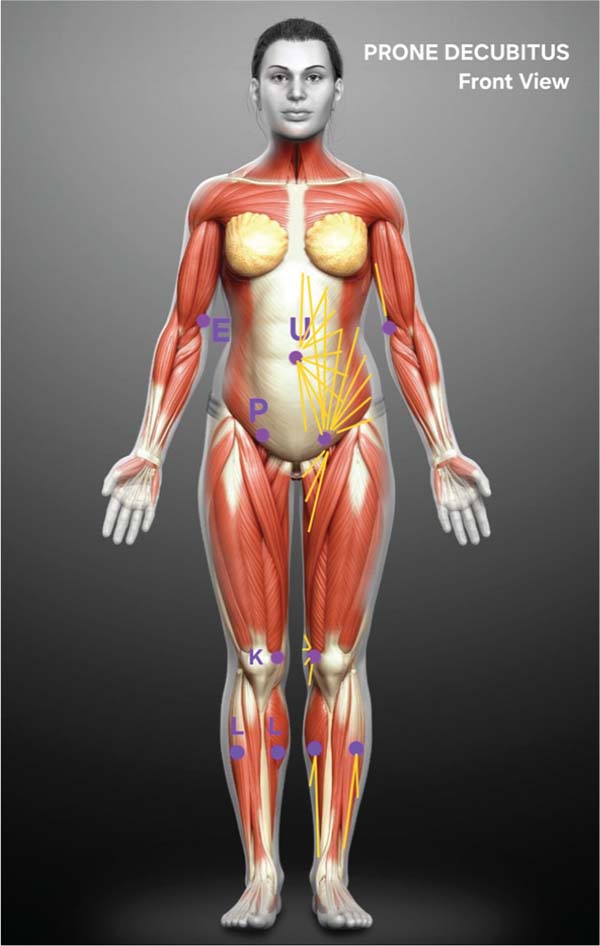
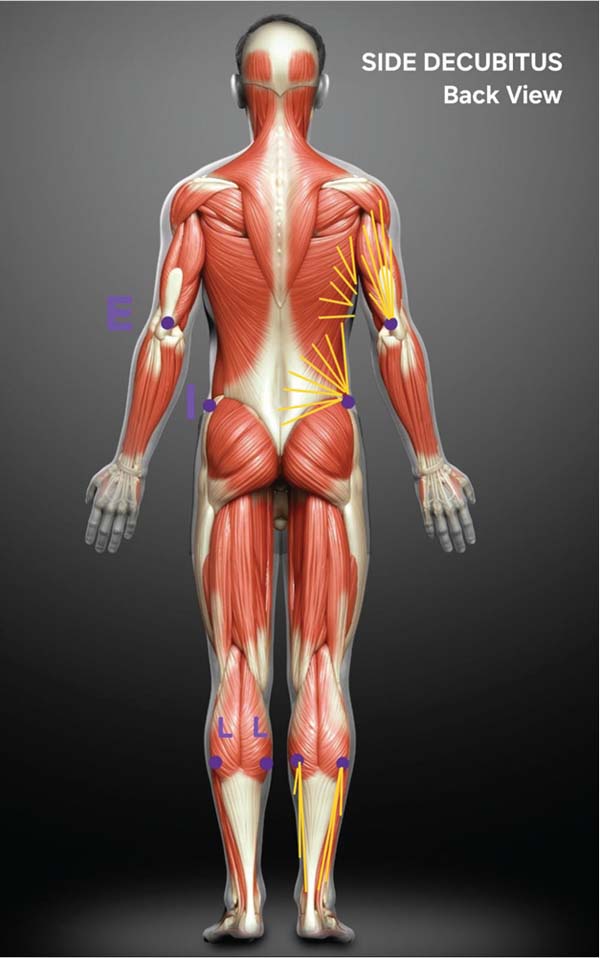
3. ACCESS PORTALS (INCISIONS) (►Figs. 8-11):
These portals were designed for the two most commonly used decubitus positions in liposuction surgeries:
3A. VENTRAL DECUBITUS (VP) (►Figs. 8-9)
• E (elbow)
• P (pubis)
• K (knees)
• L (legs)
• T (thoracic back)
• S (sacrum)
• G (gluteal groove)
• U (umbilicus)
3B. SIDE DECUBITUS (SD) (►Figs. 10-11)
• E (elbow)
• M (mammary groove)
• I (iliac crest)
• P (pubis)
• K (knees)
• L (legs)
• U (umbilicus)
4. INFILTRATED AND ASPIRATED VOLUME CONTROL
Infiltrated volume control
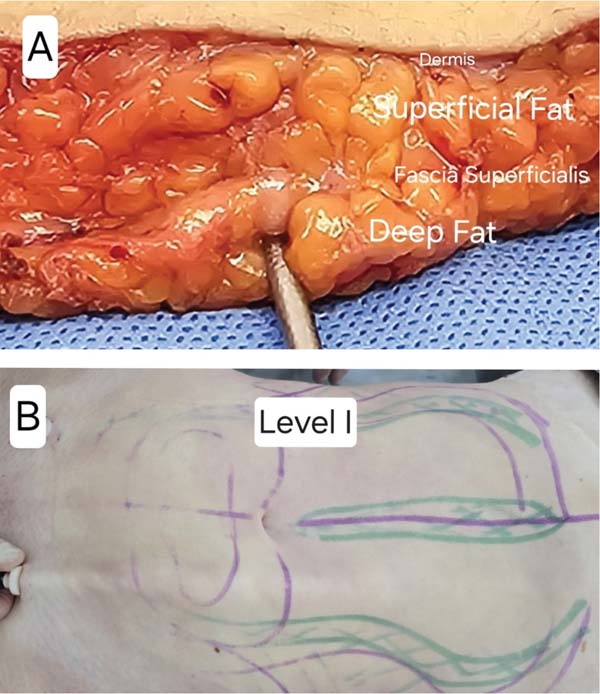
Infiltration of the prepared solution with a 50-mL graduated syringe to control each milliliter of infiltrated volume in each previously defined region. The infiltrated volume is recorded in a specific Excel spreadsheet, the LipoCodes spreadsheet, which has a model for female (►Fig.12) and another for male patients (►Fig. 13). The two spreadsheets have an automatic sum feature to control the regional and total infiltrated volumes.
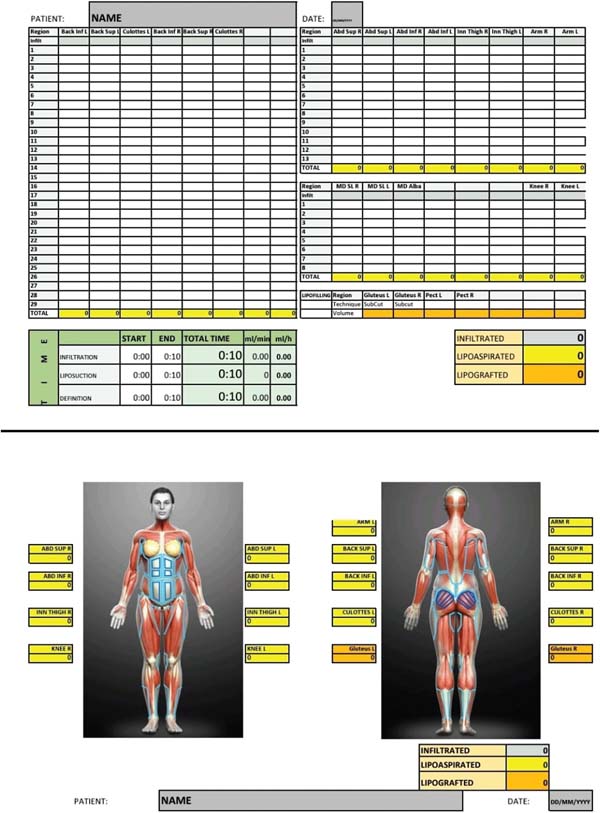
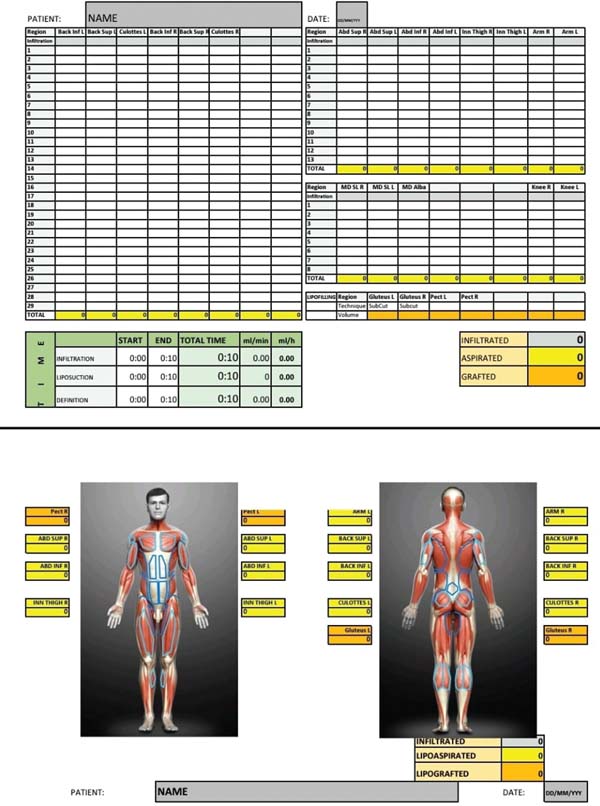
Each column of the spreadsheet corresponds to the previously described regions. The columns for the most commonly treated regions in liposuction are defined, and the blank columns are for less common regions. The infiltration volume from sequential 50-mL syringes is recorded in the first line of each column, highlighted in gray.
Aspirated volume control
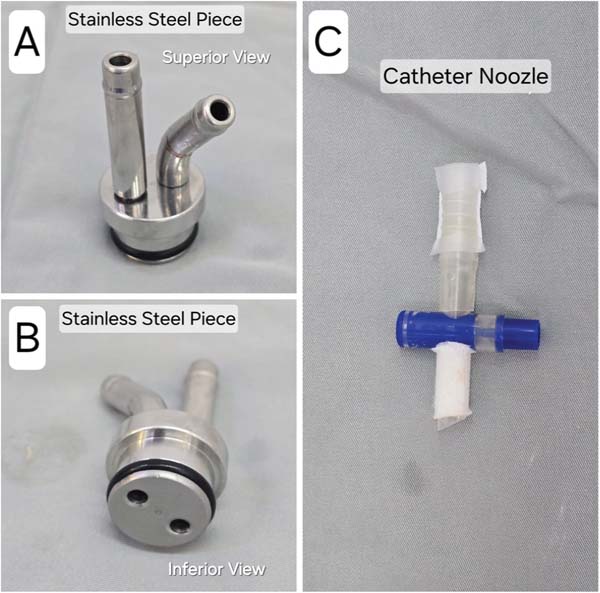
This control uses an intermediate system (►Figs. 14-15) developed by the author to count aspirated volumes positioned between the liposuction hoses, called the LipoCodes system.
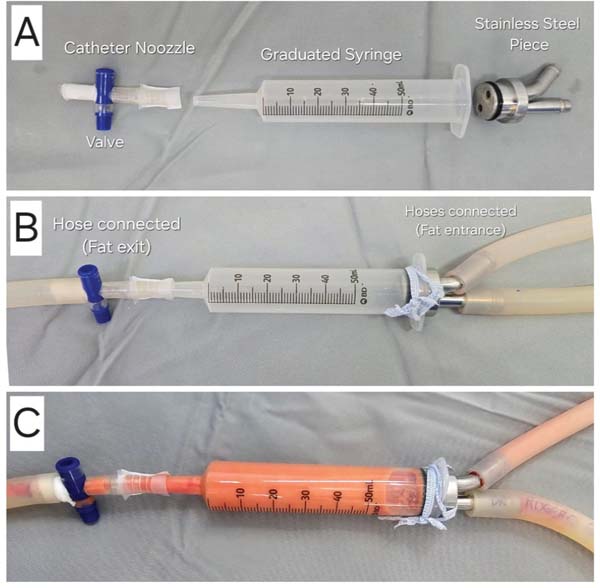
The LipoCodes system consists of a 50-mL syringe with a catheter tip, graduated in milliliters, without the plunger (which is removed) (►Fig. 14).
The upper part of the 50-mL syringe, at the plunger inlet, has a stainless-steel piece developed by the author with 2 outlets for liposuction hose connection: one hose for liposuction and the other for exhaust (►Fig. 15).
In the lower part of the 50-mL syringe, the catheter tip is connected to an outlet connector from a urine collector, and its opening and closing valve controls the volume aspirated in the 50-mL syringe (►Fig. 15).
In this system, the liposuction fat enters the upper part and fills the 50-mL syringe. When the syringe is full (►Fig. 14), the volume in milliliters is recorded on the spreadsheet (►Figs. 12-13) in the column corresponding to each region, and the total aspirated volume is automatically recorded. Next, the valve at the bottom is opened to empty the syringe and then closed.
This sequence is repeated until the liposuction outcome and volume for each region are achieved.
Grafted volume control
Fat grafting aspiration uses negative pressure and a 50-mL graduated syringe for exact control, per milliliter, of the grafted volumes in each previously defined region.
The grafted volumes by region are recorded in the space provided for fat grafting in the LipoCodes spreadsheet (►Figs. 12-13), allowing their visualization at any time during surgery or later.
Results
The methodology allowed the control of infiltrated, aspirated, and fat-grafted volumes in milliliters for each previously defined region, the surgical speed in mL/min and mL/h, and the total surgical time.
Discussion
New techniques, technologies, and scientific publications on liposuction continue to evolve significantly, increasingly seeking better and more predictable outcomes1-14 with maximum potential safety.15-20
The Lipocodes methodology allows precise control of infiltrated and aspirated volumes per milliliter with specific and well-defined anatomical regions, coinciding with the usual locations of fat deposits, well known by plastic surgeons, with higher anatomical definitions for better understanding and education purposes.
The methodology defines three levels of suction depth, which, combined with the above-mentioned anatomical regions, provide a three-dimensional view of liposuction.
This objective information on the volume in milliliters from each region increases the expectation of the aesthetic outcome to control symmetry and treat any potential asymmetries, in addition to controlling the grafted fat volume when indicated. Currently, the endpoint in most liposuctions has been based on coarser volume information (deciliter or centiliter) and the subjective observation and personal experience of each plastic surgeon. In this methodology, the volume information is inserted into the Lipocodes spreadsheet, which is monitored by the surgeon and the medical team during the procedure, to achieve greater precision in liposuction by using objective parameters that help the surgeon forecast the volumes for infiltration and aspiration in each region, guiding the correction of any asymmetries. It also contributes to better team monitoring, making liposuction more educational, controlled, and objective for younger and more experienced surgeons.
In addition, objective information about infiltrated and aspirated volumes is significant for safety by aiding intra and postoperative fluid replacement.
The author developed the LipoCodes intermediate system (►Figs. 14-15) for counting aspirated volumes with a 50-mL syringe without a plunger and a stainless-steel part positioned between the liposuction hoses in an artisanal manner to control each milliliter. Current commercial systems count in 50-mL increments, which prevents more rigorous volume control. The author is negotiating to develop the intermediate system with specialized companies for large-scale production and commercialization.
Another significant piece of information provided by LipoCodes is the surgical speed in mL/min and mL/h. This information provides the plastic surgeon and the team with knowledge on the pace of the surgery, the liposuctioned fat removal time, and the procedural duration. The importance of surgical time to minimize complications is well cited in the literature.11,14,17,18,20,25 Since there is growing concern regarding surgical time, the Lipocodes methodology encourages a better intraoperative flow and improves the understanding of the entire team through standardization, reducing anesthesia time, surgical time, materials, and stress.
The defined portals or incisions lie at the two most commonly used decubitus positions for posterior region liposuction. These are suggestions to minimize the number of portals, and the surgeon can modify them according to personal preference.
Regarding liposuction depth, level I is below the superficial fascia, allowing increased volumetric reduction and lower contour remodeling; this is why we begin liposuction in this deeper plane. Level II is above the superficial fascia for better contour remodeling, requiring more care to avoid irregularities. Level III is closer to the dermis, and it requires leaving the cannula holes facing downwards to avoid greater trauma to the deep dermis, which could cause exaggerated retractions, dyschromia, pain, and other complications. This liposuction for definition purposes was originally described by Mentz26 and improved by Hoyos,27 being widely used by several plastic surgeons and challenged by others.
By controlling the well-defined regions, the infiltrated and aspirated volumes, and the aspiration depth levels, the three-dimensional liposuction has a more precise control for better outcomes, asymmetry correction, and fewer touchups and refinements.
The LipoCodes methodology systematizes liposuction regardless of the equipment and technique preferred by each plastic surgeon. The goal is to make liposuction more controlled, objective, didactic, and educational, with higher predictability.
The LipoCodes methodology can use any liposuction equipment: syringe, aspirator, vibration system, ultrasound, and laser. The plastic surgeon does not need to change their preferred technique or equipment for infiltration and liposuction, only add the intermediate system and the LipoCodes spreadsheet to transfer the information obtained during the liposuction surgery with or without grafting.
Our review found six articles using volume and region control measurements. Araújo28 measured the skin fold with an adipometer before and six months after the procedure, showing the outcomes with no numbers, only photos. Cohen et al.10 compared three-dimensional magnetic resonance images and total fat aspirated for the entire abdomen, before and six months after surgery. Marongiu et al.21 cited a method to control and accelerate infiltration. Bukret and Alonso22 developed geometric models for liposuction marking to improve efficacy and safety in laser liposuction. Harutyunyan et al.23 used ultrasound to calculate the fat volume for liposuction and developed specific software. Lastly, Gu et al.24 developed a method for circumferential liposuction in several locations in the arm, quantifying clinical efficacy. We did not find references presenting a clear control of infiltrated and aspirated volumes, defining regions and aspiration planes, describing access portals, or controlling surgical speed.
In summary, the main objectives of the LipoCodes methodology are to:
1. Obtain objective parameters of liposuction volumes byareas, depth, and volumes to be aspirated.
2. Develop an intraoperative flow (sequence).
3. Improve the understanding of the entire team throughstandardization.
4. Reducelosses (anesthesia, materials, surgical time, stress).
5. Increase the surgical procedure flow.
6. Reduce surgical time.
7. Improve predictability.
8. Obtain more consistent outcomes.
9. Improve asymmetry treatment.
10. Minimize the potential for refinements or adjustments.
11. Assist in the artistic thinking of the plastic surgeon.
12. Use with any liposuction equipment preferred by eachplastic surgeon.
Conclusion
The author developed the LipoCodes methodology to be used with any liposuction equipment: syringe, aspirator, vibration system, ultrasound, and laser.
This information aims to assist the plastic surgeon with objective parameters, infiltrated, aspirated, and grafted volume control, and surgical time control so that the surgical team can obtain more predictable outcomes, improve asymmetry treatment, reduce the need for touch-ups and reinterventions, and increasing patients’ safety.
REFERENCES
1. Sood J, Jayaraman L, Sethi N. Liposuction: Anaesthesia challenges. Indian J Anaesth 2011;55(03):220-227. Doi: 10.4103/00195049.82652
2. Cucchiaro JV. Abdominal etching: Surgical technique and outcomes. Plast Reconstr Surg 2020;145(02):454e. Doi: 10.1097/PRS.0000000000006460
3. Durán Vega HC, Lopez Echaury A, Flores E. The Energy a Plastic Surgeon Expends during Liposuction. Plast Reconstr Surg Glob Open 2023;11(05):e5001. Doi: 10.1097/GOX.0000000000005001
4. Hoyos A, Perez ME, Guarin DE, Montenegro A. A report of 736 high definition lipoabdominoplasties performed in conjunction with circumferential Vaser liposuction. Plast Reconstr Surg 2018;142 (03):662-675
5. Gomes RS, Mattiello CM, Rendon NB, Garcia EB, Gomes HFC, Ferreira LM. Lipoaspiração de Alta Definição e Tubos de Silicone. Rev Bras Cir Plást 2018;33(04):567-571
6. Gomes RS, Nicolau GV. Abdominal Liposuction: Evolving from high to medium definition. Rev Bras Cir Plást 2021;36(02):1-11
7. Nagy MW, Vanek PF Jr. A multicenter, prospective, randomized, single-blind, controlled clinical trial comparing VASER-assisted Lipoplasty and suction-assisted Lipoplasty. Plast Reconstr Surg 2012;129(04):681e-689e. Doi: 10.1097/PRS.0b013e3182442274
8. Danilla S, Babaitis RA, Jara RP, et al. High-Definition Liposculpture: What are the Complications and How to Manage Them? Aesthetic Plast Surg 2020;44(02):411-418. Doi: 10.1007/s00266019-01475-6
9. Pereira-Netto D, Montano-Pedroso JC, Aidar ALES, Marson WL, Ferreira LM. Laser-Assisted Liposuction (LAL) Versus Traditional Liposuction: Systematic Review. Aesthetic Plast Surg 2018;42 (02):376-383. Doi: 10.1007/s00266-018-1085-2
10. Cohen SR, Weiss ET, Brightman LA, et al. Quantitation of the results of abdominal liposuction. Aesthet Surg J 2012;32(05): 593-600. Doi: 10.1177/1090820X12449457
11. Lipp MB, Butterwick K, Angra K, Chunhara C, Goldman MP. Evaluation of Long-Term Outcome and Patient Satisfaction Results After Tumescent Liposuction. Dermatol Surg 2020;46 (Suppl 1):S31-S37. Doi: 10.1097/DSS.0000000000002498
12. Cansancao AL, Condé-Green A, David JA, Cansancao B, Vidigal RA. Use of Tranexamic Acid to Reduce Blood Loss in Liposuction. Plast Reconstr Surg 2018;141(05):1132-1135. Doi: 10.1097/PRS.0000000000004282
13. Rodríguez-García FA, Sánchez-Peña MA, de Andrea GT, et al. Efficacy and Safety of Tranexamic Acid for the Control of Surgical Bleeding in Patients Under Liposuction. Aesthetic Plast Surg 2022; 46(01):258-264. Doi: 10.1007/s00266-021-02486-y
14. Willet JW, Alvaro AI, Ibrahim AK, Javed MU. A Systematic Review of Efficacy and Complications of High-Definition Liposuction. Plast Reconstr Surg 2023;152(01):57-63. Doi: 10.1097/PRS.0000000000010203
15. Nogueira FVM, Coelho GVBF, Da Silveira VF Junior, De Andrade CZN, Hetem CMC, Farina JÁ Junior. Liposuction and fat embolism: a literature review. Rev Bras Cir Plást 2015;33(04):511-517
16. Cantarelli J, Godoy MF. Safe limits for aspirate volume under wet liposuction. Obes Surg 2009;19(12):1642-1645. Doi: 10.1007/s11695-009-9958-8
17. Kaoutzanis C, Gupta V, Winocour J, et al. Cosmetic Liposuction: Preoperative Risk Factors, Major Complication Rates, and Safety of Combined Procedures. Aesthet Surg J 2017;37(06):680-694. Doi: 10.1093/asj/sjw243
18. Rohrich RJ, Avashia YJ, Savetsky IL. Cosmetic Surgery Safety: Putting the Scientific Data into Perspective. Plast Reconstr Surg 2020;146(02):295-299. Doi: 10.1097/PRS.0000000000006980
19. Wu S, Coombs DM, Gurunian R. Liposuction: Concepts, safety, and techniques in body-contouring surgery. Cleve Clin J Med 2020;87 (06):367-375. Doi: 10.3949/ccjm.87a.19097
20. Kanapathy M, Pacifico M, Yassin AM, Bollen E, Mosahebi A. Safety of Large-Volume Liposuction in Aesthetic Surgery: A Systematic Review and Meta-Analysis. Aesthet Surg J 2021;41(09):1040-1053. Doi: 10.1093/asj/sjaa338
21. Rubino C, Marongiu F, Manzo MJ, et al. A simple and cheap system to speed up and to control the tumescent technique procedure: the Tedde’s system. Eur Rev Med Pharmacol Sci 2014;18(11): 1647-1648
22. Bukret WE, Alonso GF. Use of 3D geometrical models to improve efficacy and safety of Laser-assisted liposuction: a prospective study. Rev Bras Cir Plást 2015;30(03):381-390
23. Harutyunyan R, Gilardino MS, Papanastasiou VW, Jeffries SD, Hemmerling TM. Ultrasound Calculation of Fat Volume for Liposuction: A Clinical Software Validation. Aesthet Surg J 2023;43 (10):1150-1158. Doi: 10.1093/asj/sjad121
24. Gu Y, Kang N, Lv Q, et al. Application of a Proposed MultiPositional Circumferential Arm Liposuction Method and Quantification of its Clinical Efficacy Evaluation. Aesthetic Plast Surg 2021;45(03):1115-1124. Doi: 10.1007/s00266-020-02121-2
25. Barros LFL, Teixeira VF, Reis Júnior JAP, Ferraz RA, Araújo DC, Vendramin FS. Complications in liposuction: systematic review. Rev Bras Cir Plást 2023;38(01):1-10
26. Mentz HA III, Gilliland MD, Patronella CK. Abdominal etching: differential liposuction to detail abdominal musculature. Aesthetic Plast Surg 1993;17(04):287-290. Doi: 10.1007/BF00437100
27. Hoyos AE, Millard JÁ VASER-assisted high-definition liposculpture. Aesthet Surg J 2007;27(06):594-604. Doi: 10.1016/j.asj.2007.08.007
28. Almeida ARH, Mafra AVC, Araújo GKM. Methodology for analysis of results in liposuction. Rev Bras Cir Plást 2011;26(02):288-292
1. Plastic Surgery Service, Hospital Carlos Corrêa, Florianópolis, SC, Brazil
Address for correspondence Rogerio Schützler Gomes, Serviço de Cirurgia Plástica, Hospital Carlos Corrêa, Florianópolis, SC, Brazil (e-mail: plasticarogerio@gmail.com adm@rogeriogomes.com.br).
Article received: March 29, 2024.
Article accepted: September 29, 2024.
Conflict of Interests
The author has no conflict of interests to declare.




















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter