

Ideas and Innovation - Year 2024 - Volume 39 -
Tuberous Breast Treatment: A New Photochemical Perspective
Tratamento de mama tuberosa: Uma nova perspectiva fotoquímica
ABSTRACT
Background Tuberous breast deformity is a congenital anomaly with several presentations that has always been a real challenge for plastic surgeons. As such, we propose using the One Selective Tissue Engineering Photostimulation (STEP) technique, which acts directly on the denaturalization of the fibrous septae, releasing the inframammary fold, and allowing a subglandular pocket creation.
Materials and Methods The present retrospective descriptive study included 15 patients treated by the senior author using the One STEP technique from 2017 to 2020. All subjects received sedation and local anesthesia. The Meara et al./Kolker system was used to classify tuberous breast deformity in all patients. Our proposed protocol relies on infrared light at 1,210nm wavelength, which has photochemical properties.
Results From 2017 to 2020, 15 female patients with tuberous breasts underwent treatment with the One STEP technique. These subjects presented atraumatic results, less bleeding, and retraction of the areolomamillary herniation and nipple-areolar complex, enabling the placement of a subglandular round breast implant with a satisfactory outcome for the patients.
Conclusion Although different techniques may be used to treat tuberous breasts, they do not always provide the same outcome in distinct classifications. In our study, patients with tuberous breast deformity underwent the same treatment using the One STEP technique, regardless of the classification, with one-stage correction, obtaining satisfactory outcomes in all cases. The One STEP technique showed excellent results in the treatment of patients with tuberous breasts, with less trauma, bleeding, and edema, in addition to a better postoperative recovery time.
Keywords: breast; breast implant; lasers; lipectomy; mammaplasty; stem cell transplantation; stem cells
RESUMO
Introdução A mama tuberosa é uma anomalia congônita com apresentações variadas que sempre foi um verdadeiro desafio para os cirurgiões plásticos. Por isso propomos a utilização da técnica One Selective Tissue Engineering Photostimulation (STEP), que atua diretamente na desnaturalização dos septos fibrosos, liberando o sulco inframamário permitindo a criação da bolsa subglandular.
Materiais e Métodos Trata-se de um estudo descritivo retrospectivo que incluiu 15 pacientes do autor sénior que foram tratados com a técnica One STEP no período de 2017 a 2020. Sedação e anestesia local foram utilizadas em todos os casos. O Sistema de Meara/Kolker foi utilizado para classificar a deformidade tuberosa da mama em todas as pacientes. Nosso protocolo proposto é baseado na onda da luz infravermelha de 1.210 nm, que possui propriedades fotoquímicas
Resultados Entre 2017 e 2020, 15 pacientes do sexo feminino com mama tuberosa foram tratadas com a técnica One STEP apresentando resultados atraumáticos, com menos sangramento, retração da herniação areolomamilar e do complexo aréolopapilar (CAP), e permitindo a colocação de um implante mamário subglandular com resultado satisfatório para as pacientes.
Conclusão Existem diferentes técnicas para tratar a mama tuberosa, mas elas nem sempre alcançam o mesmo resultado em classificações distintas. Em nosso estudo, as pacientes com mama tuberosa foram tratadas da mesma forma com a técnica One STEP independemente da classificação com correção em um estágio, obtendo resultados satisfatórios em todos os casos. A técnica One STEP apresentou excelentes resultados no tratamento de pacientes com mama tuberosa, com menor trauma, menor sangramento, menor edema e melhor tempo de recuperação pósoperatória.
Palavras-chave: células-tronco; implante mamário; lasers; lipectomia; mama; mamoplastia; transplante de células-tronco; stem cells
Introduction
The treatment of tuberous breasts has always been a real reconstructive challenge for plastic surgeons. Tuberous breasts are a rare congenital deformity that can be uni or bilateral and result from abnormal breast development, becoming evident in puberty. The first authors to describe it were Rees and Aston, in 1976.1 The main clinical features are reduced breast parenchyma (hypoplasia of one or all breast quadrants), abnormal inframammary fold elevation, decreased skin envelope in the horizontal and vertical dimensions, increased areolar diameter with herniation of the breast parenchyma through the nipple-areolar complex (NAC), and a constricted breast base.2,3,4,5,6 Fibrous septa are the most significant factor in this condition, affecting normal breast development.
The classification of tuberous breasts was first introduced by Von Heimburg,4 in 1996, and modified in 1999 by Grolleau,5 who described only 3 groups based on breast base deformity. In 2013, Costagliola et al.6 proposed adding type 0 for the minor forms, characterized by the simple areolar protrusion, which may be permanent or intermittent on a regular breast base. In 2017, Innocenti et al.7 proposed a new classification including all presentation forms, considering the anatomical location of the defect, breast volume, and tissue quality.
For this article, we chose the classification proposed by Kolker et al.,8 in 2015, based on the Meara et al.9 classification from 2000 for tuberous breasts. It is a three-level classification system considering anatomical features and the severity of tuberous breast deformities (►Table 1).
| TYPO | BASE | FOLD | COVERAGE | VOLUME DOS SEIOS | PTOSIS | AREOLA |
|---|---|---|---|---|---|---|
| 1 | Mild constriction | Laterally normal, slight medial elevation | Proper | Minimal deficiency, no deficiency, or hypertrophy | Mild, moderate, or severe | Enlarged |
| II | Moderate constriction | Medial and lateral elevation | Inferior insufficiency | Moderate deficiency | None or mild | Normal, mild or moderate hernia |
| III | Severe constriction | Elevation of the entire sulcus or absence thereof | Global insufficiency | Severe deficiency | Mild or moderate | Severe hernia |
Note: Meara/Kolker classification.8
In addition to the multiple classifications, tuberous breast objective confirmation relies on the Northwood index as per a review from Pacifico et al.10 This index is the relationship between the areola diameter and the herniation measured in profile. An index greater than 0.4 defines a tuberous breast; regarding severity, the disease can be mild (0.4-0.5), moderate (0.51-0.6), or severe (0.61-0.7).
The treatment of tuberous breasts has always been controversial due to their anatomical complexity, and previous techniques in two or more stages were very complex, traumatic, and unsatisfactory.1,10,11,12,13,14,15,16,17,18,19,20,21 The One Selective Tissue Engineering Photostimulation (STEP) technique uses a new infrared laser diode with a wavelength of 1,210 nm acting directly on the denaturalization of the fibrous septa, which account for the rigidity of the histological support of the affected tissue, releasing the mammary fibrosis (collagen and reticulin fibers) and inframammary fold, allowing the creation of the subglandular pocket, increasing the lower pole and lowering the fold for breast implants. The previously collected fat preserved by the One STEP technique22,23 contained stem cells stimulated by infrared light, and we immediately injected it into the areas requiring volume and skin elasticity. This technique provides satisfactory, natural, and less traumatic outcomes for patients regardless of disease classification with a one-stage correction.
The present paper presents the efficiency and simplicity of the One Step technique for adequate correction of this deformity in all its potential presentations (grades I—III) with an atraumatic postoperative period regardless of the classification in one-stage correction.
Materials and Methods
The current retrospective descriptive study included 15 patients (30 breasts) treated by the senior author, with a mean age of 28 years (range: 18-39), who underwent treatment with the One STEP technique from 2017 to 2020. Tuberous breast classification relied on the Meara et al./Kolker system (►Table 1).
Patient information included tuberous breast classification by three independent plastic surgeons, surgical outcomes, and complications. The minimum follow-up period was 10 months. We asked all patients to complete a Breast Cancer Quality of Life Questionnaire (BREAST-Q) to measure their satisfaction, using four scales from the Breast Q reduction/mastopexy module, namely, satisfaction with the outcome, satisfaction with breasts, psychosocial wellbeing, and sexual wellbeing. Patient scores ranged from 0 to 100.
The postoperative evaluation relied on photographs to analyze symmetry, breast shape, normalization of areola size, scar, and overall aesthetic outcome. We graded the postoperative outcomes as excellent, very good, good, or poor.
Surgical Technique
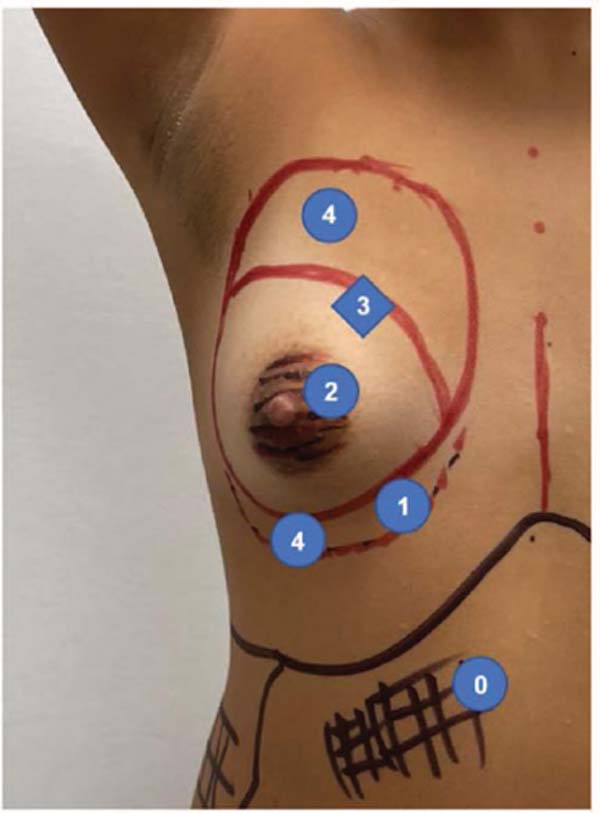
All patients underwent the same surgical procedure, regardless of their grade, starting with preoperative markings in the vertical position. Important landmarks included a vertical midline mark, the existing inframammary fold, and the proposed inframammary fold. All patients received sedation plus local anesthesia.
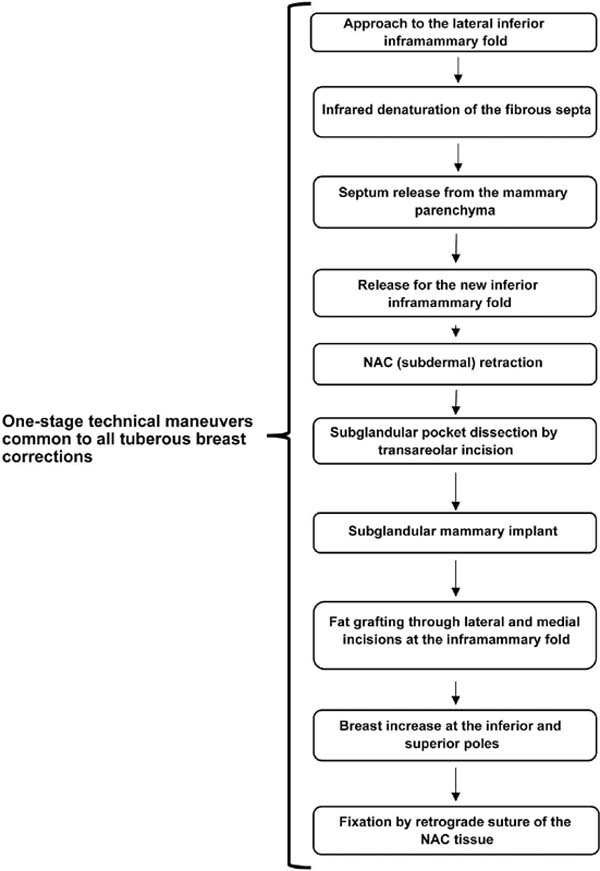
We will describe the procedure in three phases.
Laser Emission
For the denaturalization of fibrous septa, The One STEP technique used a new 1,210 nm wavelength infrared laser diode (DMC Brasil, Curitiba, PR, Brazil) in the preconfiguration body liposculpture, which emits laser energy through a 600-micron optical fiber contained in a 2 mm diameter cannula in an area to treat all the affected tissue. We infiltrated 160 mL of 0.9% saline solution, 40 mL of lidocaine, and 1 mL of adrenaline at the base of the breast and the existing inframammary fold. The entry point for the cannula was an incision in the lateral portion of the inframammary fold.
The application of the laser energy released the inframammary fold and denatured the fibrous septa and other histological supports accounting for rigidity. This procedure eliminated the fibrosis (collagen and reticulin fibers) in the breast quadrants and inframammary fold. The laser application occurred in small, slow movements until a significant reduction of tissue resistance was reached. Next, laser energy application occurred subdermally at the areola complex to achieve skin retraction with the predefined skin tightening.24
Implant Placement
After laser emission for fibrous septa denaturalization, subglandular pocket dissection was easy, increasing the lower breast pole and creating a new inframammary fold. All implants were microtextured, with volumes ranging from 240 to 280 mL, and placed subglandularly through a transareolopapilar (Pitanguy) incision.
Fat Grafting
We performed minor liposuction in the abdominal region using the One STEP9 technique to harvest adipose tissue for fat grafting. We placed the fat graft in areas requiring volume and skin elasticity using PicoGraft, with no fat manipulation and preserving all stromal regenerative elements. We used a 2-mm curved cannula connected to a 10-mL syringe through two small incisions, one in the new lateral inframammary fold and the other in the medial inframammary fold. The injected volume ranged from 120 to 220 mL. Lastly, we sutured the medial and the lateral incisions.
This method treats breast deformity with a one-stage correction; it does not require another surgical time for reconstruction and is independent of the disease classification (►Fig. 2).
Results
From 2017 to 2020, a total of 15 female patients with tuberous breasts underwent treatment with the One STEP technique. The mean postoperative follow-up time was 10 months (range: 8-12 months). ►Tables 2 and 3 summarize the patient demographics. There were eight type-I deformities, four type-II deformities, and three type-Ill deformities. In all patients, we used a 2-mm inframammary fold incision approach. The mean BREAST-Q postoperative satisfaction score was 80 ± 12. The mean breast satisfaction score was 88 ±11, the mean psychosocial wellbeing score was 83 ± 12, and the sexual wellbeing score was 80 ± 16.
| Deformity classification | Number of patients (%) |
|---|---|
| Type 1 | 8 (53.3) |
| Type II | 4 (26.6) |
| Type III | 3(20) |
| Deformity presentation | |
| Unilateral | 0(0) |
| Bilateral | 15(100) |
| Value | |
|---|---|
| Number of patients | 15 |
| Number of breasts | 30 |
| Age at surgery | |
| Mean | 28 |
| Range | 18-39 |
| Follow-up period | |
| Mean | 10 |
| Range | 08-12 |
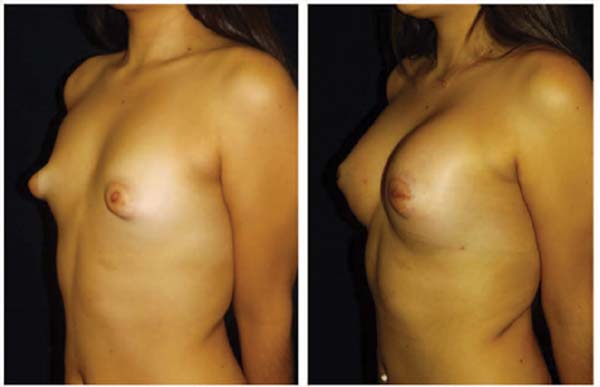
In each patient, we released the breast fibrosis in the affected quadrants and lowered the inframammary fold, allowing the placement of a round subglandular breast implant, with reduction (skin tightness pre-configuration) of the areola-nipple herniation and NAC. We observed significant retraction of the NAC skin, increasing the distance between the NAC and the new inframammary fold.
All patients presented an increase in lower pole volume and elasticity using the PicoGraft fat grafting in conjunction with subglandular breast implant and natural atraumatic results, with less bleeding and edema.
In all cases, the final aesthetic outcome was acceptable to the satisfaction of the patient and the surgical team with a one-stage correction. The aesthetic outcomes based on symmetry, breast shape, areola size normalization, scar, and overall aesthetic result by blind scoring were excellent in 9 (60%) patients and very good in 6 (40%) patients. There were no poor aesthetic outcomes.
We observed no complications, such as infection, seroma, or hematoma, during the follow-up period. The technique has no functional impact on the breasts, nor does it interfere with future lactation. We placed drains in patients receiving breast implants (►Figs. 3,4,5).
Discussion
Although different techniques can treat tuberous breast deformity, they do not always provide the same outcome in distinct patients with the same disorder classification, and some subjects require a two-phase intervention. In addition, a more noticeable deformity requires careful surgical procedure planning to provide a satisfactory outcome.1,10,13,14,15,16,17,18,19,20,21
Fasciotomies or flaps are often used to release or dissolve the fibrous septa of the lower pole of the tuberous breast and the short submammary fold. It is worth noting that the chemical connections between tissues are strong, and any attempt to use mechanical disruption for connective tissue dissolution is not feasible or complete.
The photochemical reaction from our technique can dissolve these fibrous septa by denaturalizing them without the thermal effect from other lasers.22,23,24 This denaturalization frees the subcutaneous cellular tissue and the breast tissue from the rigidity in the lower pole. In fat harvesting for grafting, this technique also allows fat preservation with a 98% viability.11,12,22,23,24
In our study, patients with tuberous breasts underwent the same treatment with the One STEP technique regardless of their disease classification in a one-stage correction. It is a much simpler way of treating the affected quadrant tissue, releasing breast fibrosis, retroareolar herniation/sagging, and NAC retraction; in addition, it allows repositioning of the inframammary fold for (previously harvested) fat grafting and preparing a wide retroglandular pocket for implant placement through a transareolapapilar (Pitanguy) incision.
No patient presented complications; however, as the literature has no clear data addressing the time to complications, such as the development of capsular contracture, our followup period may have been insufficient to detect cases of late capsular contracture, asymmetry, or deformity development.
Since complications may arise over a longer time, we cannot rule out the possibility of their late occurrence.8,9
Our study has several limitations. Although our outcomes, technique, and patient satisfaction are promising, this is a retrospective review of 30 breasts in 15 patients. Therefore, our data do not necessarily reflect the general population. However, our results are promising, and our technique may treat patients with tuberous breast deformity. Further larger studies are required to confirm our results.
Conclusion
The present case series shows that the adjuvant use of this new technology is a safe procedure allowing the release of fibrous septa through the photochemical property of light, allowing expansion of the lower pole for treatment using prostheses, high-quality fat grafts, or both.
REFERENCES
1. Rees TD, Aston SJ. The tuberous breast. Clin Plast Surg 1976;3(02): 339-347
2. Nahabedian MY. Breast deformities and mastopexy. Plast Reconstr Surg 2011;127(04):91e-102e
3. Gorvetzian J, Funderburk C, Copeland-Halperin LR, Nigriny J. Correction of the tuberous breast deformity in a prepubescent male patient: A surgical approach to an unusual problem. JPRAS Open 2019;19:98-105
4. von Heimburg D, Exner K, Kruft S, Lemperle G. The tuberous breast deformity: classification and treatment. Br J Plast Surg 1996;49(06):339-345
5. Grolleau JL, Lanfrey E, Lavigne B, Chavoin JP, Costagliola M. Breast base anomalies: treatment strategy for tuberous breasts, minor deformities, and asymmetry. Plast Reconstr Surg 1999; 104(07): 2040-2048
6. Costagliola M, Atiyeh B, Rampillon F. Tuberous breast: revised classification and a new hypothesis for its development. Aesthetic Plast Surg 2013;37(05):896-903
7. http://www.annalsplasticsurgery.com
8. Kolker AR, Collins MS. Tuberous breast deformity: classification and treatment strategy for improving consistency in aesthetic correction. Plast Reconstr Surg 2015;135(01):73-86
9. Meara JG, Kolker A, Bartlett G, Theile R, Mutimer K, Holmes AD. Tuberous breast deformity: principles and practice. Ann Plast Surg 2000;45(06):607-611
10. Pacifico MD, Kang NV. The tuberous breast revisited. J Plast Reconstr Aesthet Surg 2007;60(05):455-464
11. Centurión P, Gamarra R, Caballero G, et al. Optimizing harvesting for facial lipografting with a new photochemical stimulation concept: One STEP technique™. Eur J Plast Surg 2020;43:733-742. Doi:10.1007/S00238-020-01643-x
12. Centurion P, Noriega A. Fat preserving by laser 1210-nm. J Cosmet Laser Ther 2013;15(01):2-12. Doi: 10.3109/14764172.2012.758376
13. Aston SS, Rees TD. (1980) Mammary augmentation, correction of asymmetry and gynecomastia. In: TD Rees (ed) Aesthetic plastic surgery. Philadelphia: Saunders; 990-995
14. Puckett CL, Concannon MJ. Augmenting the narrow-based breast: the unfurling technique to prevent the double-bubble deformity. Aesthetic Plast Surg 1990;14(01):15-19
15. Ribeiro L, Canzi W, Buss A Jr, Accorsi A Jr. Tuberous breast: a new approach. Plast Reconstr Surg 1998;101(01):42-50, discussion 51-52
16. Ribeiro L, Accorsi A Jr, Buss A, Pessĵa MC. Short scar correction of the tuberous breast. Clin Plast Surg 2002;29(03):423-431, vii
17. Mandrekas AD, Zambacos GJ. Aesthetic reconstruction of the tuberous breast deformity: a 10-year experience. Aesthet Surg J 2010;30(05):680-692
18. Mandrekas AD, Zambacos GJ, Anastasopoulos A, Hapsas D, Lambrinaki N, Ioannidou-Mouzaka L Aesthetic reconstruction of the tuberous breast deformity. Plast Reconstr Surg 2003;112(04): 1099-1108, discussion 1109
19. Serra-Renom JM, Muñoz-Olmo J, Serra-Mestre JM. Treatment of grade 3 tuberous breasts with Puckett’s technique (modified) and fat grafting to correct the constricting ring. Aesthetic Plast Surg 2011;35(05):773-781
20. Silva Neto MP, Rodrigues da Cunha Colombo L, et ai. Tratamento de mamas tuberosas com incisões combinadas. Rev Bras Cir Plást 2012;27(03):421-427
21. Gutierrez-Ontalvilla P, Naidu NS, Blanco EL, Brito EC, Ruiz-Vails A. Autologous Fat Grafting with Percutaneous Fasciotomy and Reduction of the Nipple-Areolar Complex for the Correction of Tuberous Breast Deformity in Teenagers. Aesthetic Plast Surg 2020;44(02):264-269. Doi: 10.1007/s00266-019-01531-1
22. Centurion P, Caballero G, Weiss M. Comment to: "Laser-Assisted Liposuction (LAL) Versus Traditional Liposuction: Systematic Review". Aesthetic Plast Surg 2019;43(04):1122-1123
23. Centurion P Letter to Editor: Rediscovering the – involutedregenerative system? Aesthetic Plastic Surgery Journal Manuscript Number: APSU-D-21-00791. Doi: 10.1007/s00266-021-02585-w September 2021.
24. Centurion P, Delgado M, Talavera J, Dela Cruz JAmerican Journal of Surgery Case Reports Research Article. Study and Assessment of a New Stromal Vascular Fraction Harvest Technique: Subcutaneous Tissue Source Harvesting with One STEPTM Technique. Am J Surg Case Rep. 2024;5(03):1121
1. Private practice, Lima, Peru
2. Associação dos Ex-Alunos do Professor Ivo
Pitanguy (AEXPI), Rio de Janeiro, RJ, Brazil
3. Departamento of Investigation, Universidad
Ricardo Palma, Lima, Peru
Address for correspondence Alexandro Carlo Cavenago-Arce, Departamento de Investigación, Universidad Ricardo Palma, Lima, Peru (e-mail: alexandrocavenago@yahoo.com; comite.eticafamurp@urp.edu.pe).
Article received: March 11, 2024.
Article accepted: November 16, 2024.
Conflict of Interests
The authors have no conflict of interests to declare.













 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter