

Original Article - Year 2024 - Volume 39 -
Rehabilitation of Burn Injuries in the Lower Limbs: A Retrospective Study
Reabilitação de queimaduras em membros inferiores: Um estudo retrospectivo
ABSTRACT
Introduction Burns are among the main external causes of death in Brazil, and their occurrence in the lower limbs is less common.However, significant burns in this region are a challenge for reconstruction, especially in later stages, due to the difficulty in recreating the region's particular anatomy and sustaining limb functionality.
Materials and Methods We conducted a retrospective analysis of the medical records of burn victims with sequelae treated at a rehabilitation hospital from 2001 to 2005.
Results We evaluated 44 patients, 61.3% of whom were male and aged between 21 and 40 (mean age: 26) years. Most (98%) were of working age (< 60 years). Thermal causal agents were predominant, and 65% of the patients underwent different surgeries and rehabilitation programs.
Conclusion The analysis revealed severe deformities, including articular issues and amputations, in patients with long-standing burns, especially male individuals, of working age, and from the Midwestern, Northern, and Northeastern regions of Brazil. The required treatments involved different complex surgical procedures and physical therapy for rehabilitation depending on the causal agent and the extent of the injury, always prioritizing limb functionality and the patient's reintegration into society.
Keywords: burns; lower extremity; plastic surgery procedures; rehabilitation
RESUMO
Introdução As queimaduras estão entre as principais causas externas de morte registradas no Brasil, e a sua ocorrência nos membros inferiores é menos comum. Porém, caso ocorram queimaduras significativas nessa região, a reconstrução, sobretudo a tardia, é desafiadora, devido à dificuldade de se recriar a anatomia particular da região, o que dificulta a manutenção funcional do membro.
Materiais e Métodos Realizou-se uma análise retrospectiva de prontuários de pacientes vítimas de sequelas de queimaduras atendidos em um hospital de reabilitação de 2001 a 2005.
Resultados Foram avaliados 44 pacientes, dos quais 61,3% eram do género masculino e estavam na faixa etária de 21 a 40 (média de idade: 26) anos. Observou-se que 98% dos queimados estavam em idade produtiva (< 60 anos). Houve predomínio de agente causal térmico, e 65% dos pacientes foram submetidos a diferentes cirurgias e programas de reabilitação.
Conclusão A análise revelou deformidades severas, com comprometimento articular e amputações, em pacientes com tempo prolongado de queimadura, especialmente do sexo masculino, em idade produtiva e provenientes do Centro-Oeste, Norte e Nordeste. Os tratamentos necessários envolveram procedimentos cirúrgicos complexos e fisioterápicos para reabilitação, que variaram conforme o agente causal e a extensão da lesão, e foram priorizadas a funcionalidade do membro e a reintegração do paciente à sociedade.
Palavras-chave: extremidade inferior; procedimentos de cirurgia plástica; queimaduras; reabilitação
Introduction
Burns are serious traumatic injuries often resulting in high morbidity and mortality, which compromise the emotional well-being and quality of life of the victims. Burns are among the main external causes of death recorded in Brazil, and they are more common in populations with lower socioeconomic status and delayed growth and development.1
An adult with severe burns presents second-degree burns affecting more than 25% or third-degree burns in more than 10% of the body surface. In addition to severe and moderate burns, third-degree burns on the face, hands, and feet are severe. Burns on the lower limbs (LLs) are more frequent in children, and they are usually caused by scalding due to "reaching and pulling", for instance, in accidents with containers of hot liquids.8
The complete treatment of LL burns can be complex or direct, conservative or surgical, depending on the nature of the burn. Proper care requires experience and training. The keys to good management of LL burns are understanding burn pathophysiology, proper management of burns in the acute stage, infection prevention, and appropriate initial reconstruction guided by the patient's long-term needs.8,9,12,13
Initial care in the acute stage of the burn must be immediate and specialized to minimize sequelae and preserve the subject's functionality. Subsequently, the patient may require a prolonged rehabilitation phase and late treatment, involving a physical therapy program, orthoses, prostheses, or both, and even new surgical procedures for functional and/or esthetic reconstructions. It is worth highlighting that the therapeutic approach is multidisciplinary and requires frequent monitoring by surgeons.4,9,12
Social and psychological support are paramount, since severe sequelae with major socioeconomic repercussions are common. Scars, joint contractures, retractions, stiffness, muscle weakness, chronic pain, and LL amputations are devastating due to the impairment in the subject's functionality given the importance of this region, especially for walking. The risk of amputation after an extremity burn increases from 1.5% to 18% to 40% in the case of circumferential or fourth-degree burns.1,3,4,6,7,13
Therefore, the management of LL burns is a challenge. Thus, knowing the appropriate treatment and rehabilitation of patients with LL burns directly influences their prognosis and quality of life.
As such, the present study aimed to describe the therapeutic strategies in the late care of burn patients and to define the profile of patients with sequelae of LL burns treated at a rehabilitation hospital.
Results and Discussion
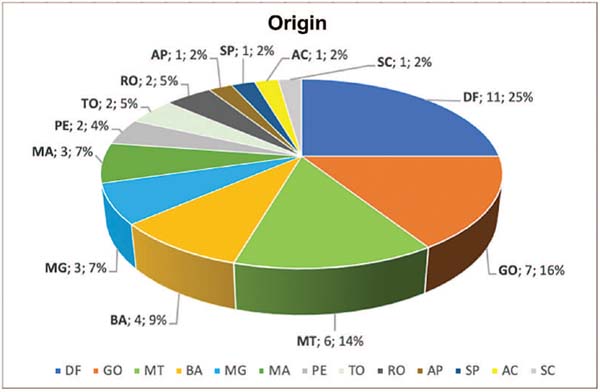
We evaluated the medical records of 44 patients with sequelae of LL burns treated at a rehabilitation hospital from 2001 to 2005, corresponding to 29% of the burn sequelae treatments at the time. The median follow-up was of 3 years (range: 1 month to 12 years). Regarding the demographic data, there was a higher frequency of male (61.3%) compared to female subjects (38.7%), in the age group from 21 to 40 (mean age: 26) years. Furthermore, 98% of the patients were of working age (< 60 years). Regarding their state of origin, 11 (25%) were from the Federal District, 7 (16%), from the state of Goiás, and 6 (14%), from the state of Mato Grosso (►Fig. 1 and ►Table 1).
| Patients | N | % |
|---|---|---|
| Gender | 27 | 61.3 |
| Male | 17 | 38.7 |
| Female | ||
| Age group (years) | 17 | 39 |
| 01-20 | 18 | 41 |
| 21-40 | 8 | 18 |
| 41-60 | 1 | 2 |
| 61-80 | ||
| Age (years): mean ± standard deviation | 26±14.86 | |
| State of origin | 11 | 25 |
| Federal District | 7 | 15.9 |
| Goiás | 6 | 13.3 |
| Mato Grosso | 20 | 45 |
| Other | ||
| TOTAL | 44 | 100 |
| Follow-up: median (range) | 3 years (1 month-11 years) |
The data on LL burns revealed that, regarding the body regions affected, 5 (11.3%) burns occurred on a single foot, 18 (40%), in both feet, eight (18%), in both LLs, and 2 (4.5%), in a single LL, involving the leg and knee. Of the initial 44 patients, 22 (50%) presented lesions in more than 1 region, mainly the hands (22.7%) and upper limbs (ULs; 18%). ►Table 2 shows the distribution of patients with sequelae according to the burned region.
| N | % | ||
|---|---|---|---|
| Causal agent | Thermal | 34 | 77.2 |
| Electric | 10 | 23.8 | |
| Total | 44 | 100 | |
| Region | Foot: unilateral | 5 | 9 |
| Foot: bilateral | 18 | 32 | |
| Lower limbs | 8 | 14 | |
| Lower limb | 2 | 3 | |
| Hand and foot | 10 | 18 | |
| Lower and upper limbs | 8 | 14 | |
| Others | 4 | 7 | |
| Total | 55 | 100 | |
| Burn time (years): median (range) | 11 years (4 months-70 years) | ||
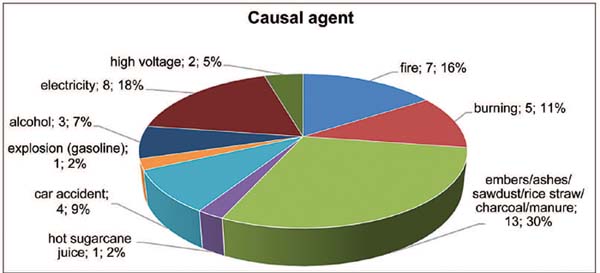
As for the causal agent (►Fig. 2), most burns resulted from embers/ash/sawdust/rice straw/coal/manure (30%), followed by electrical burns (18%), with fire being the third causal agent with the highest prevalence (11%).
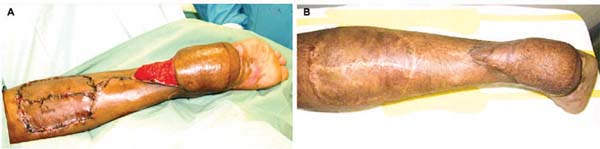
All patients with plantar burns presented contractures in the ankle and foot, dorsal flexion (►Fig. 3), plantar flexion (►Fig. 4), lateral deviation, stiffness of the entire ankle joint and the dorsum of the foot, classified as severe per Chang et al.3 (indicating functional impact), significant damage to adjacent tissues, impossibility or difficulty in using footwear, impact when walking, and involvement of deep anatomical structures (tendons, ligaments, and joint capsule).


The median time between the burn and the treatment was of 11 years (range: 4 months to 70 years). The analysis of the surgical data revealed that 29 different procedures were performed in the hospital in question (►Figs. 3 4 5 6), with 19 patients undergoing 1 procedure and 10 requiring more than 2 procedures, including 4 patients submitted to 2 surgeries, 3 patients submitted to 3 surgeries, 2 patients submitted to 4 surgeries, and 1 patient requiring more than 4 procedures.

Most surgeries were scar retraction release with reconstruction and total skin grafting (28%), multiple Z-plasty (12%), capsuloplasty, tendon lengthening or tenotomy, and Kirschner wire fixation. Among the previous complications, 9 (20%) patients presented with limb amputation upon admission (1 unilateral transtibial amputation, 1 transfemoral amputation, 5 toe amputations, 1 UL amputation, and 1 LL amputation, all performed in the emergency room).
In addition, 1 patient presented paraplegia and was using a wheelchair, 1 presented cardiorespiratory arrest, septicemia, and cerebral ischemia during emergency care, and 3 presented ulcers in burn scar areas which, on biopsy, were squamous cell carcinomas (SCC/Marjolin's ulcer). ►Table 3 outlines the surgical and non-surgical procedures.
| Patients | N | % |
|---|---|---|
| Procedures | 29 | 66 |
| Surgical | 15 | 34 |
| Non-surgical | ||
| Total | 44 | 100 |
| Number of procedures per patient | ||
| Surgical procedures | N | % |
| Full skin graft | 19 | 28 |
| Multiple Z-plasty | 8 | 12 |
| V-Y flap | 5 | 7 |
| Double Z-plasty | 2 | 3 |
| Five-flap | 4 | 6 |
| Cross-leg flap | 1 | 2 |
| Reverse sural flap | 3 | 5 |
| Skoog flap | 2 | 3 |
| Resection of ossification | 1 | 2 |
| Phalange disarticulation | 5 | 7 |
| Finger filleting | 2 | 3 |
| Capsuloplasty, tendon lengthening, | 6 | 9 |
| or tenotomy | 7 | 10 |
| Kirschner wire fixation | 3 | 5 |
| Foot squamous cell carcinoma excision | ||
| 68 | 100 | |
| Non-surgical procedures | ||
| Gait assessment in the movement laboratory | ||
| Patellar tendon bearing orthosis | ||
| Static ankle-foot orthosis | ||
| Static ankle-foot orthosis with anterior cap | ||
| Exoskeletal transtibial prosthesis | ||
| Molded insole | ||
| Assisted passive and active physiotherapy exercises and muscle strengthening | ||
| Locomotion assistance |
Non-surgical procedures were performed exclusively in 15 (34%) patients, and they consisted in physical-functional assessment, use of static ankle-foot orthoses, patellar tendon bearing (PTB), articulated plantar orthosis with dorsal or plantar traction, muscle strengthening exercises, burned skin care, and instruction on the use of oily substances, sun protection, molded insoles, orthoses, and LL prostheses (►Fig. 7). All patients, including those undergoing surgery, were referred for physical therapy and physical-functional examination, and they monitored by the physical therapy team before and after surgery to assist with locomotion, produce orthoses, and perform other procedures.
The profile of the patients treated for LL burns revealed their occurrence in young subjects of working age, mostly male. This analysis also highlighted the high morbidity of the injuries, the long time between the burn and treatment, and the number of procedures required for patient rehabilitation.
Most burns resulted from thermal injuries, and burns caused by thermal agents are always more frequent than other causes. These burns resulted from exposure to flames, superheated liquid or solid substances, hot surfaces, and friction. Thermal burns, mainly secondary to contact, expose deep structures in areas of thinner skin (back of the hand and fingers) or require skin coverage with free flaps at a later stage as a sequela due to the unfavorable evolution of tissue healing or skin graft retraction, as shown in ►Fig. 8.
The decisions regarding the treatment varied according to the time since the burn, the classification of the contracture type, and the patient's age and complaints. Given the significance of the LLs for locomotion, body weight support, and body balance, burn sequelae and complications in this region are critical and have a crucial impact on the functionality of the affected subject.
Examples of this impact include talocrural joint disorders, pain complaints, changes in the orthostatic position, gait, and posture, as well as potential consequences in the pelvis, spine, and other structures of the locomotor system.
Consistent with Ribeiro et al.,11 despite the area of body surface comprised by the feet is small, foot burns trigger great functional loss and a high morbidity rate. Recovery from this injury relies on good treatment in the acute stage, since such procedures determine a greater or lesser degree of sequelae, potentially facilitating the recovery period.
Understanding the regular and functional anatomy of the limb was fundamental in the indication of repair procedures, mainly aimed at the functional recovery of the affected area. The dorsal region was the most affected due to the orthostatic position assumed in most cases of contact with potentially harmful elements.
The present case series revealed that scar retraction release required tendon lengthening, capsulotomies, joint repositioning with metal wire fixation, closure with skin grafts or flaps, and the use of orthoses. These measures are frequently adopted to rehabilitate patients with sequelae from severe burns.
According to Tarazi and Bitterman14, circumferential and fourth-degree burns resulting from high voltage or electricity increase the chances of limb amputation. As such, acute treatments may require skin grafts, local flaps, muscle flaps, microsurgery, dermal regeneration matrices, special dressings, and other measures, just like in the late care. However, the sequelae include tissue shortening, mainly in the neurovascular bundle, compromising surgical success.
In addition to the size of the injury, the initial approach often determines the continuity of the treatment, indicating greater or lesser sequelae. According to the authors,14 although less frequent, sequelae after LL burns can cause functional changes, including limitations in walking and muscle development, as in cases of retractions in the popliteal fossa, the dorsal region of the foot, the toes, and the ankles. In these regions, conventional procedures, such as Z-plasty, grafts, and local flaps can improve most retractions. The therapeutic challenge is higher in cases involving plantar coverage and joint limitation.
Jaiswal et al.15 suggested that surgeries for the correction of LL contractures must be performed up to 6 months after the burns. These authors also recommended surgical contracture correction in 2 stages: initially with a plantar approach and, 6 months later, with a dorsal approach, or vice-versa.
Foot burns deform the toes in hyperextension and cause subluxation of the metacarpophalangeal joint. Varus or valgus plantar deformities are rarer. The treatment is performed in stages, starting with scar tissue and fibrous cord release with simple procedures, such as Z-plasty, V-Y-plasty, and double Z-plasty. When these procedures fail, skin grafting is indicated.
Interdigital space treatment may employ the Skoog technique, with a triangular flap for neocommissure and larger lesions with osteoarticular exposure. Flap use, especially local ones, should be carefully considered, if feasible. However, revisions or more than one surgical procedure may be necessary.
Stockly et al.16 studied data from the United States National Database of the Burn Model System from 1996 to 2015, which compared the demographic and clinical characteristics of adult survivors of burns by electrical and fire/flame injuries. These authors assessed the scores on the Satisfaction with Life Scale (SWLS), Short Form-12 Physical Composite Score (SF-12 PCS), Short Form-12 Mental Composite Score (SF12 MCS), and employment status 24 months after the injury. The study16 included 1,147 adult burn survivors (111 affected by electrical injuries and 1,036 affected by fire/flame injuries). Subjects with electrical lesions were more likely to be male and to be injured at work (p < 0.001). The SF-12 PCS scores were significantly worse for survivors from electrical injuries than for survivors from fire/flame injuries (p < 0.01 ) 24 months after the burn.
Pedrazzi et al.17 conducted a study at the Zurich Burn Center evaluating the surgical management and outcome of patients with electrical injuries over the past 15 years, emphasizing risk factors for amputation and reconstructive strategy. They analyzed 89 patients and performed 522 surgeries. Escharotomies and fasciotomies were performed in 40.5% and 24.7% of the cases respectively, mostly upon admission. The total amputation rate was of 13.5% (23 amputations in 12 patients).
The development of compartment syndrome, rhabdomyolysis, elevated blood levels of myoglobin and creatine kinase (CK), renal failure, sepsis, and respiratory complications were related to a higher risk of amputation (p < 0.001 ). These authors17 reported the performance of 66 flap-based reconstructions (25% of the cases): 49 locoregional flaps, 3 pedicled distant flaps, and 14 free flaps. Two flaps were lost (flap failure rate of 14%).
The authors17 concluded that both flap losses occurred in early reconstruction (within 5 to 21 days). Electrical injuries remain a cause of high morbidity and mortality, with a high amputation rate. Predictors of amputation can support physicians in surgical care and decision-making. Reconstruction of this type of injury remains challenging: surgical management with early fasciotomy, serial escharotomy, and early reconstruction are still the procedures of choice in the acute stage.
Although rare, a burn injury can also result in amputation. Regarding thermal burns, accidents due to chemical and electrical exposure are associated with a higher risk of amputation, in an ascending risk scale. Other risk factors for amputations include the presence of comorbidities, such as diabetes, and black skin color. Further studies are needed to understand this relationship.
Extensive thermal burns are also associated with an increased risk of amputation. The benefits of amputation include increased survival in patients with severe injuries. However, there are potential difficulties in rehabilitation after discharge, which is associated with poor-quality skin coverage and contracture formation over the stump. In the rehabilitation program to which the patients of the present study were submitted, 20% were amputees who were admitted for prosthetics and supplementary surgical procedures.
Burn injuries can result in a series of consequences and complications, including neurological abnormalities, such as mononeuropathy and spinal cord injury, mainly caused by exposure to high voltage.
Peripheral neuropathy is the most common neuromuscular complication. It may result from thermal and electrical burns, and there are some reports of neuropathy from chemical burns. Clinically, the condition may present with paresthesia, neuropathic pain, dysesthesia, weakness, and foot drop syndrome. The severity of the neuropathy depends on the extent and depth of the injury.
Peripheral neuropathy results from direct nerve destruction by the aggressor agents, but it can also occur due to other causes, such as neurotoxins, inflammation, vasa nervorum occlusion, splint use, surgical interventions, or edema compressing nerve structures.
The present study showed severe secondary deformities due to burns, which is consistent with the experience of many authors, confirming the importance of providing adequate care and monitoring the growth of children with LL burns until adulthood, even in the absence of functional limb abnormalities.
It is worth emphasizing that physical-functional analysis in the orthostatic position, while walking and wearing shoes, is essential in follow-up visits and upon admission to rehabilitation service. It is also crucial to pay due attention to the patient's complaints and prioritize functionality over esthetics. However, most cases with late sequelae cannot recover joint mobility, leading to stiffness and pain.
Moreover, in surgical procedures, it is important to delicately handle the burned skin, protect and preserve the vascular pedicles, address each joint, and release them with capsuloplasty, tendon lengthening or tenotomy, as well as Kirschner wire fixation. In the postoperative period, it is essential to control pain, elevate the operated limb, avoid plantar support until complete healing, and consider performing staged procedures. Furthermore, it is valuable to compensate for asymmetries in limb length, protect or remove bone projections, and offer insoles and orthoses to improve the quality of life of the patients.
Conclusion
The profile of the patients with burn sequelae treated at a rehabilitation hospital revealed severe deformities in subjects of working age, with prolonged burn time, mainly from the Midwestern, Northern, and Northeastern regions Brazil, requiring different surgical and physical therapy procedures for rehabilitation.
The right time to act in the treatment of sequelae is highly variable and depends on their severity and consequences. If the late injury represents a serious impairment to normal-life functions, it must be treated in time to avoid greater repercussions, reflecting the importance of professional training in centers treating those patients.
A careful analysis of the clinical, functional, and anatomical characteristics of the burned region enables the determination of the severity of each sequela. In addition, it dictates the interventions necessary for reconstruction and the adoption of non-surgical measures. In summary, it is crucial to understand the techniques and procedures for the rehabilitation and treatment of these patients and the profile of this population, aiming at preserving the function of the affected limb and reintegrating patients into society. It is also worth noting the existing opportunities for improving the quality of evidence-based treatment and rehabilitation in all areas of LL burns, highlighting the significance of research in this field.
REFERENCES
1. Jacobs C, Vacek J, Many B, Bouchard M, Abdullah F. An Analysis of Factors Associated with Burn Injury Outcomes in Low- and Middle-Income Countries. J Surg Res 2021;257:442-448
2. Özkal Ö, Seyyah M, Topuz S, Konan A. Lower limb functional status and its determinants in moderate/major burns 3-6 months following injury: A two-center observational study. Burns [Internet] 2020; [citado 2 nov 2023] PubMed
3. Chang JB, Kung TA, Levi B, Irwin T, Kadakia A, Cederna PS. Surgical management of burn flexion and extension contractures of the toes. J Burn Care Res 2014;35(01):93-101
4. Zoni AC, Domínguez-Berjón MF, Esteban-Vasallo MD, Velázquez-Buendía LM, Blaya-Nováková V, Regidor E. Socioeconomic inequalities in injuries treated in primary care in Madrid, Spain. J Public Health 2016; [citado 29 jun 2023]:fdw005 PubMed
5. Ngu F, Patel B, McBride C. Epidemiology of isolated foot burns in children presenting to a Queensland paediatric burns centre- a two-year study in warmer climate. Burns Trauma 2017;5:6
6. Smolle C, Cambiaso-Daniel J, Forbes AA, et al. Recent trends in burn epidemiology worldwide: A systematic review. Burns 2017; 43(02):249-257
7. Asif M, Ebrahim S, Major M, Caffrey J. The use of Integra™ as a novel technique in deep burn foot management. JPRAS Open 2018; 17:15-20
8. Ali HA, Fayi KA, Alkhathami AM, Alturaiki N, Alshammari EM. Foot drop in patients with extensive 3rd and 4th degree burn, case series study. Int J Burns Trauma 2023;13(01):8-12
9. Khan MM, Cheruvu VPR, Krishna D, Laitonjam M, Minz R, Joshi R. Post-traumatic wounds over the dorsum of the foot- our experience. Int J Burns Trauma 2020;10(04):137-145
10. Costa CF, Sousa GC, Rodrigues AC, et al. Perfil de pacientes que sofreram queimaduras no Brasil: uma revisão integrativa. Rev Eletronica Acervo Saude 2017;8:624-632
11. Ribeiro DR, Cruvinel SS, Costa PA, Valente HC, Costa TR. Epidemiological profile of burned patients at the clinical hospital of the federal university of Uberlândia in brazil. Rev Bras Cir Plast (RBCP) – Braz J Plast Sugery 2021;36(02):181-187
12. Momeni M, Sediegh-Marufi S, Safari-Faramani R, Akhoondinasab MR, Karimi H, Karimi AM. Lower Extremity Burns, Complications, and Outcome. J Burn Care Res 2020;41(02):409-415
13. Sasor SE, Chung KC. Upper extremity burns in the developing world. Hand Clin 2019;35(04):457-466
14. Tarazi JM, Bitterman AD. Thermal Injuries Occurring to the Foot: A Review. Foot Ankle Clin 2023;28(01):173-185
15. Jaiswal KS, Gupta S, Goil P, Mohammad A, Gupta P. Empirical Evidence on the Reliability of Lateral Supramalleolar Flap over Reverse Sural Flap for Local Soft Tissue Coverage of Dorsum of the Foot and Ankle Defects. Indian J Plast Surg 2023;56(02):159-165
16. Stockly OR, Wolfe AE, Espinoza LF, et al. The impact of electrical injuries on long-term outcomes: A Burn Model System National Database study. Burns 2020;46(02):352-359
17. Pedrazzi NE, Naiken S, La Scala G. Negative pressure wound therapy in pediatric burn patients: a systematic review. Adv Wound Care (New Rochelle) 2020; [Internet], 10 jun 2020 [citado 29 jun 2023]
1. Department of Plastic Surgery, Instituto
Euro-Americano de Educação, Ciência e Tecnologia, , Brasília, DF,
Brazil
1. Associação das Pioneiras Sociais, Brasília, DF,
Brazil
Address for correspondence Katia Torres Batista, PhD, Núcleo de Prática Jurídica Assistência à Comunidade, Av. das Nações trecho 0, conjunto 5, Setor de Clubes Esportivos Sul, Asa Sul, Brasília, DF, 70200-001, Brazil (e-mail: katiatb@terra.com.br).
Article received: July 25, 2023.
Article accepted: September 29, 2024.
Conflict of Interests
The authors have no conflict of interests to declare.
















 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter