

Case Report - Year 2024 - Volume 39 -
Surgical Alternative for Multiple Pilar Cutaneous Leiomyoma of the Lower Limb: Case Report and Literature Review
Alternativa cirúrgica para leiomioma cutâneo pilar múltiplo de membro inferior: Relato de caso e revisão da literatura
ABSTRACT
Pilar leiomyoma, or benign neoplasia of the arrector pili muscles, is an uncommon pathology, although it is the most frequent type of cutaneous leiomyoma. It occurs in young adults, affecting both sexes equally. It presents as multiple or isolated, reddishbrown, papulonodular lesions. Although nomalignant tumors have been reported, it is important to include this pathology in the differential diagnosis of papulonodular cutaneous lesions. Surgical treatment is often reserved for prolonged and symptomatic cases, with relapse reports. In this paper, we report the case of a 28-year-old male patient with a diagnosis of pilar leiomyoma on the lateral thigh and right leg who underwent a tangential skin resection.
Keywords: plastic surgery; leiomyoma; lesion; neoplasias; skin
RESUMO
O leiomioma pilar, ou neoplasia benigna do músculo eretor do pelo, é uma patologia incomum, apesar de ser o tipo mais frequente de leiomioma cutâneo. Ocorre entre adultos jovens, acometendo igualmente ambos os sexos. Sua apresentação se dá em lesões dolorosas, isoladas ou múltiplas, papulonodulares vermelhas e castanhas. Apesar de não ter sido relatada nenhuma malignização dos tumores, é importante incluir essa patologia no diagnóstico diferencial de lesões cutâneas papulonodulares. O tratamento cirúrgico geralmente é reservado a casos extensos e sintomáticos, com relatos de recidiva. Nesse artigo, relatamos o caso de um paciente de 28 anos, do sexo masculino, com diagnóstico de leiomioma pilar em face lateral de coxa e perna direita submetido à ressecção de pele tangencial.
Palavras-chave: cirurgia plástica; leiomioma; lesão; neoplasias; pele
Introduction
Leiomyomas are benign soft tissue neoplasms arising from smooth muscle. Cutaneous pilar leiomyoma is a rare benign tumor, with an incidence of approximately 5%, and can present in solitary or multiple forms (Ragsdale, 2009). Solitarylesions are more common than multiple ones (Malhotra, 2010).
This disease is more common in adults,although there are reported cases in children. They do not have a gender predilection, although data are conflicting in the literature (Raj, 1997).
The differential diagnosis includes neurofibroma, dermatofibroma, schwannoma, fibromyoma, and smooth muscle cell hamartoma (Latoni, 2000), especially in solitary lesions. Biopsy is the test used for diagnosis confirmation.
These lesions are usually refractory to analgesic treatment. Some reports suggest the efficacy of calcium channel blocker medications (such as nifedipine), alpha-blockers (such as phenoxybenzamine), nitrates, and gabapentin (Raj, 1997). A patient with clinical contraindications for surgery underwent CO2 laser ablation with good outcomes.
Objective
We herein report the case of a 28-year-old male patient with multiple cutaneous leiomyomas who underwent surgical therapy.
Case Report
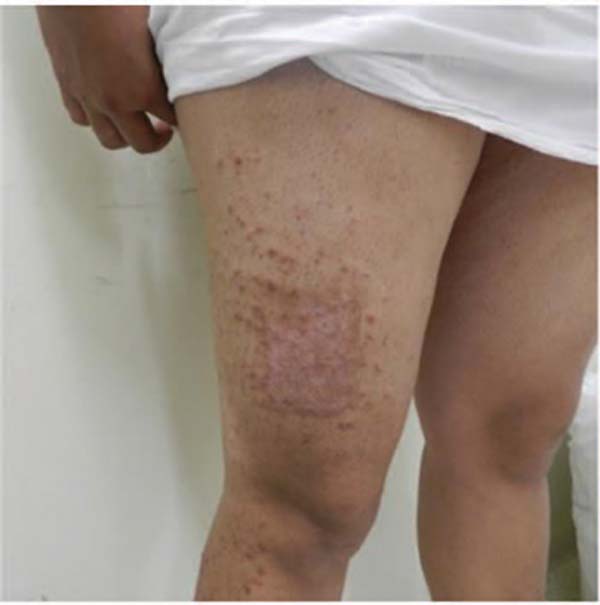
A 28-year-old male patient of mixed race presented with multiple reddish-brown papular lesions of varying sizes, isolated in some regions, and coalesced in parts of the right thigh and leg. The lesions appeared in the last 5 years. The patient presented with pain, mainly when exposed to cold, which limited his movement and work activity. The pathological diagnosis confirmation of pilar leiomyoma relied on two biopsies. It was not feasible to resect the lesions separately. The patient underwent surgery at Hospital Público Regional de Sobradinho, Brasília, DF, Brazil, on April 18, 2022. This research was approved by the Ethics in Research Committee under the protocol number 69524923.0.0000.0257.
We opted for tangential resection with a Blair knife in the thigh area with the highest density of lesions, measuring 14 by 8cm on the anterior surface (►Fig. 1). At 8 months after the procedure, the patient reported pain improvement in the operated area, with no keloid scar formation (►Fig. 2). For the anterolateral area of the thigh and right leg, we chose a wide and tangential resection with a Blair knife (►Fig. 3). The patient had no postoperative complications. In the first 6 months, he reported improvement in pain and quality of life. However, some lesions recurred in the operated area.
Discussion
Superficial (cutaneous) leiomyomas are benign smooth muscle tumors that may originate from the arrector pili muscles, dartos, vulvar, and mammary smooth muscles, or the smooth muscles surrounding the dermal blood vessels. Their classification includes piloleiomyomas (solitary or multiple), external genitalia leiomyomas, and angioleiomyomas (Kumar, Abbas, and Fausto, 2005). The first report of a cutaneous leiomyoma dates back to 1854 by Rudolf Virchow.
These are relatively uncommon neoplasms, and their exact incidence is unknown. The pathogenesis remains to be determined, but it is believed that piloleiomyomas arise from smooth cells within the arrector pili muscle of the pilosebaceous unit (Hoyt, 2015). Multiple piloleiomyomas may occur sporadically or be autosomal dominant inherited (with variable penetrance), as part of the Reed syndrome.
Piloleiomyomas, or pilar leiomyomas, may be solitary or multiple. A single patient may present hundreds of lesions. They are firm, reddish-brown to skin-colored nodules or papules (Bologna, 2010). Solitary piloleiomyomas develop mainly during adulthood, with a similar gender distribution. When multiple, the distribution pattern is most commonly clustered and linear following the Blaschko lines, but scattered lesions may occur. Most are 1 to 2 cm in diameter and usually develop on the extremities and trunk (especially the shoulder). Solitary lesions favor the limbs, while multiple ones mostly appear on the trunk (Cizmeci, 2007). They are often associated with spontaneous or induced pain, such as cold exposure.
Histologically, pilar leiomyomas are smooth muscle cell tumors intertwined and arranged in a spiral, without atypia or mitotic activity.
Surgical excision is the indicated treatment for cases with few lesions and may be curative for solitary or limited tumors. However, 50%ofmultiplelesioncasesrecur within6monthsto 15 years. For numerous and painful piloleiomyomas, some authors recommend a drug treatment, despite its limited efficacy.11 Drug treatment includes gabapentin, oral or topical nitroglycerin, lidocaine, nifedipine, verapamil, phenoxybenzamine, phentolamine, hyoscine, analgesics, and antidepressants. Cryotherapy and electrocoagulation have shown little benefit (Suzuki, 2007).
Tangential resection is frequent in plastic surgery for wound and burn debridement or skin graft removal (Bolgiani and Serra, 2010). Recurrence is probably more common in lesions in the deeper dermis, with no tangential resection. In these cases, we suggest a new, more delimited tangential resection, potentially complemented by a CO2 laser.
Conclusion
The literature does not report tangential excision for pilar leiomyoma treatment. The use of this technique in the case herein reported was efficient for multiple lesion treatment, especially for pain relief. Combined treatments may be effective in preventing recurrence and ensuring a cure with no complications.
REFERENCES
1. Martinez-Mir A, Gordon D, Horev L, et al. Multiple cutaneous and uterine leiomyomas: refinement of the genetic locus for multiple cutaneous and uterine leiomyomas on chromosome 1q42.3-43. J Invest Dermatol 2002;118(05):876–880
2. White LE, Levy RM, Alam M. Neoplasias and hyperplasias of muscular and neural origin. In: Goldsmith LA, Katz SI, Gilchrest BA, Paller AS, Leffell DJ, Wolff K, editors. Fitzpatrick’s dermatology in general medicine. 8th ed. Vol. 1. New York: McGraw-Hill; 2012. p. 1470–1.
3. Virchow R. Ueber Makroglossie und pathologische Neubildung quergestreifter Muskelfasern. Virchows Arch Pathol Anat. 1854; 7:126–138
4. Lun KR, Spelman LJ. Multiple piloleiomyomas. Australas J Dermatol 2000;41(03):185–186
5. Alam NA, Barclay E, Rowan AJ, et al. Clinical features of multiple cutaneous and uterine leiomyomatosis: an underdiagnosed tumor syndrome. Arch Dermatol 2005;141(02):199–206
6. Makino E, Yamada J, Tada J, Arata J, Iwatsuki K. Cutaneous angiolipoleiomyoma. J Am Acad Dermatol 2006;54(01):167–171
7. Kudur MH. Ageneralized multiple cutaneous piloleiomyomatosis in a young male: rare case report. Indian J Dermatol 2013;58(03):245
8. Launonen V, Vierimaa O, Kiuru M, et al. Inherited susceptibility to uterine leiomyomas and renal cell cancer. Proc Natl Acad Sci U S A 2001;98(06):3387–3392
9. Matoso A, Chen S, Plaza JA, Osunkoya AO, Epstein JI. Symplastic leiomyomas of the scrotum: a comparative study to usual leiomyomas and leiomyosarcomas. Am J Surg Pathol 2014;38(10):1410–1417
10. Idriss MH, Kazlouskaya V, Malhotra S, Andres C, Elston DM. Phosphohistone-H3 and Ki-67 immunostaining in cutaneous pilar leiomyoma and leiomyosarcoma (atypical intradermal smooth muscle neoplasm). J Cutan Pathol 2013;40(06):557–563
11. Holst VA, Junkins-Hopkins JM, Elenitsas R.Cutaneous smooth muscle neoplasms: clinical features, histologic findings, and treatment options. J Am Acad Dermatol 2002;46(04):477–490, quiz, 491–494
12. Ghanadan A, Abbasi A, Kamyab Hesari K. Cutaneous leiomyoma: novel histologic findings for classification and diagnosis. Acta Med Iran 2013;51(01):19–24
13. Aggarwal S, De D, Kanwar AJ, Saikia UN, Khullar G, Mahajan R. Disseminated cutaneous leiomyomatosis treated with oral amlodipine. Indian J Dermatol Venereol Leprol 2013;79(01):136
1. Department of Plastic Surgery, Hospital Daher
Lago Sul, Brasília, DF, Brazil
Address for correspondence Igor Moura Soares, Departamento de Cirurgia Plástica, Hospital Daher Lago Sul, Brasília, DF, Brazil (e-mail: igormoura739@gmail.com).
Article received: October 04, 2023.
Article accepted: September 29, 2024.
Conflict of Interests
The authors have no conflict of interests to declare.








 Read in Portuguese
Read in Portuguese
 Read in English
Read in English
 PDF PT
PDF PT
 Print
Print
 Send this article by email
Send this article by email
 How to Cite
How to Cite
 Mendeley
Mendeley
 Pocket
Pocket
 Twitter
Twitter